Abstract
Gram-negative bacterial endotoxemia may lead to the pathological increase of vascular permeability with systemic vascular collapse, a vascular leak syndrome, multiple organ failure (MOF), and/or shock. Previous studies demonstrated that C1 inhibitor (C1INH) protects mice from lipopolysaccharide (LPS)–induced lethal septic shock via a direct interaction with LPS. Here, we report that C1INH blocked the LPS-induced increase in transendothelial flux through an endothelial monolayer. In addition, LPS-mediated detachment of cultured endothelial cells was prevented with C1INH. C1INH also inhibited LPS-induced endothelial cell apoptosis as demonstrated by suppression of DNA fragmentation and annexin V expression. As illustrated by laser scanning confocal microscopy, C1INH completely blocked the binding of fluorescein isothiocyanate (FITC)–LPS to human umbilical vein endothelial cells (HUVECs). C1INH protected from localized LPS-induced increased plasma leakage in C57BL/6J mice and in C1INH-deficient mice. Local vascular permeability in response to LPS was increased to a greater extent in C1INH-deficient mice compared with wild-type littermate controls and was reversed by treatment with C1INH. Systemic administration of LPS to mice resulted in increased vascular permeability, which was reduced by C1INH. Therefore, these studies demonstrate that C1INH, in addition to its role in suppression of LPS-mediated macrophage activation, may play an important role in the prevention of LPS-mediated increased vascular permeability, endothelial cell injury, and multiple organ failure.
Introduction
Gram-negative bacterial infection is often complicated with systemic vascular collapse, disseminated intravascular coagulation, or vascular leak syndromes.1-3 Although much of lipopolysaccharide (LPS)–induced vascular pathophysiology can be explained through host responses to LPS,2 some evidence suggests that LPS also may play a direct role.4-7 In particular, LPS may be responsible for much of the endothelial cell injury associated with Gram-negative sepsis and septic shock.2,3,8,9 One of the pathophysiological changes in sepsis is altered microvascular permeability to macromolecules. The microvascular inflammatory response is characterized by activation of the endothelium, loss of arteriolar tone, and tissue damage. One common element to these complications is endothelial cell barrier injury and/or dysfunction. The pathophysiology of severe sepsis involves a highly complex, integrated response that includes the activation of a number of cell types, the generation of inflammatory mediators, and activation of the complement, coagulation and contact systems. Central to many of theses processes is an alteration of endothelial cell function. Multiple organ failure (MOF), a frequent complication of sepsis, is characterized by microvascular injury and increased vascular endothelial permeability.
The endothelial cells lining the vasculature are the first host tissue barriers encountered by circulating LPS. Once LPS has been localized on the endothelium, it directly evokes a number of endothelial cell responses.10 In addition to a direct role, LPS stimulates the production of inflammatory cytokines, including tumor necrosis factor (TNF)–α, interleukin (IL)–1β, IL-6, and IL-8. LPS, either alone or combined with cytokines, induces endothelial expression of adhesion molecules including E-selectin, intercellular adhesion molecule (ICAM)–1, vascular cell adhesion molecule (VCAM)–1, and tissue factor.10-12 The endothelial cell response to LPS also includes cytoskeletal protein reorganization, monolayer barrier dysfunction,6,7,13 and cell detachment from the underlying extracellular matrix.14-16 This response results in altered cell morphology, intercellular gap formation, and increased transendothelial permeability. It is possible that cytoskeletal alterations in LPS-induced endothelial cell injury are closely linked to intercellular gap formation and endothelial barrier dysfunction.16 In addition, increased protein tyrosine phosphorylation and activation of mitogen-activated protein kinases occur rapidly after LPS stimulation of endothelial cells.6,17,18 The vascular endothelium is also sensitive to LPS-induced apoptosis. This effect has been demonstrated both in vivo and in vitro.19,20 Endotoxin-induced disruption of endothelial and survival signaling is mediated through caspase cleavage of adherens junction proteins.5,16
C1 inhibitor (C1INH), a plasma glycoprotein that belongs to the serpin superfamily of serine proteinase inhibitors, regulates both complement and contact system activation. Both of these systems are activated during sepsis and appear to play complex roles in both mediation of, and protection from, endotoxin shock. Levels of proteolytically inactivated C1INH are increased in fatal septic shock, which suggests an increased turnover and a relative secondary deficiency of biologically active C1INH.21 C1INH also can be inactivated by limited proteolytic cleavage by elastase released from activated neutrophils.22,23 The inactivation of C1INH may occur locally in inflamed tissue and thereby contribute to increased local complement activation.22,23 C1INH protected mice from lethal Gram-negative endotoxin shock and blocked the binding of Salmonella typhimurium LPS to the murine macrophage cell line, RAW 264.7, and to human blood cells via its interaction with LPS.24 Deletion of the amino terminal 97 amino acid residues abrogated the ability of C1INH to bind to LPS. In addition, N-deglycosylated C1INH failed to protect from lethal Gram-negative endotoxin shock. It also did not suppress LPS binding and LPS-induced TNF-α mRNA expression in RAW 264.7 cells or human blood cells. As with intact LPS, binding of N-deglycosylated C1INH to diphosphoryl lipid A (dLPA) or monophosphoryl lipid A (mLPA) was diminished compared with the native protein.25 Therefore, C1INH, in addition to its function as a serine protease inhibitor, has a novel anti-inflammatory function mediated via the heavily glycosylated amino terminal nonserpin domain, and N-linked glycosylation of this domain is essential to mediate its interaction with the LPA moiety of LPS and to protect mice from endotoxin shock.
The overall aim of this study was to investigate the role of C1INH in the vascular permeability response induced by Gram-negative endotoxin LPS. We demonstrated that LPS-mediated endothelial barrier injury and/or dysfunction, and endothelial cell apoptosis were suppressed by treatment with C1INH. C1INH protected against increased vascular permeability in C57BL/6J mice induced by local administration of LPS. Local injection of LPS led to a greater increase in vascular permeability in C1INH-deficient mice than in wild-type littermate controls. The increased vascular permeability induced in multiple organs by intraperitoneal LPS also was reversed by administration of C1INH. These data demonstrate a potential novel biologic role of C1INH in the response to LPS exposure via protection of the vascular endothelial cell barrier and regulation of vascular permeability.
Materials and methods
Reagents
C1INH was obtained from Advanced Research Technologies (San Diego, CA). LPS from Salmonella typhimurium, fluorescein isothiocyanate (FITC)–conjugated LPS from Salmonella typhimurium, Chicago sky blue dye 60B, and Evans blue dye were purchased from Sigma Chemical (St Louis, MO). The apoptotic DNA Ladder Kit was purchased from Roche Diagnostics (Indianapolis, IN).
The vascular permeability response to LPS in mice
C57BL/6J mice (6-8 weeks old, 18-22 g; Charles River Laboratories, Wilmington, MA) were injected intravenously with Chicago sky blue dye 60 B (100 μL of 10 mg/mL) through the tail vein 5 minutes prior to subcutaneous injection of LPS (10, 25, and 50 μg in 100 μL phosphate-buffered saline [PBS]) in the abdominal skin. In other experiments, mice injected with subcutaneous LPS (10 μg) were treated with intravenous C1INH (200 μg). Control mice were injected subcutaneously with PBS or intravenously with either PBS or C1INH (200 μg/per mouse) alone. Similar experiments were performed with C1INH-deficient26 and wild-type littermate mice, except that the doses of LPS used were 0, 5, and 10 μg. In other experiments, C1INH-deficient mice injected with subcutaneous LPS (10 μg) were treated with C1INH, either by mixing the C1INH (200 μg) with LPS or by administering the C1INH (200, 400, and 600 μg) intravenously. Mice were housed in a pathogen-free environment. Mice were killed 2 hours after LPS injection, and the abdominal skin was removed. Photographs of the abdominal skin were taken with a digital Sony Cyber 3.2-megapixel camera (Sony, Tokyo, Japan). Images were processed with Adobe Photoshop 6.0 software (Adobe, San Jose, CA). For the measurement of microvascular permeability in multiple organs, C57BL/6J mice were injected intraperitoneally with LPS (20 mg/kg/mouse) in the presence or absence of C1INH (200 μg/mouse). At 5 hours after LPS, mice were injected with Chicago blue dye 60B (100 μL of 10 mg/mL) through the tail vein. At 30 minutes after dye injection, mice were killed and tissues (abdominal skin, lungs, heart, liver, and intestine; 0.1 g) were removed and put into 0.6 mL of 0.5% Na2SO4 and 1.4 mL of acetone.
The dye was extracted at 55°C for 24 h, and the absorbance measured at 630 nm using Revelation Microsoft in an MRX microplate reader (DYNEX Technologies, Chantilly, VA). The vascular permeability index for each mouse was determined by dividing the absorbance value from the LPS-injected skin by the value from the PBS-injected skin.27 All experiments were performed in compliance with relevant laws and institutional guidelines, and were approved by the CBR Institute for Biomedical Research Animal Care and Use Committee, Boston, MA.
HUVEC culture
The human umbilical vein endothelial cell (HUVEC) line HUV-EC-C (ATCC, Rockville, MD) and primary HUVECs (Cambrex, East Rutherford, NJ) were cultured in endothelial cell basal medium and endothelial cell growth medium (Cambrex) containing 5% fetal bovine serum (FBS) and gentamycin (0.05 mg/mL) at 37°C in 5% CO2. The cells were washed gently with PBS and detached with trypsin-EDTA (ethylenediaminetetraacetic acid) solution.
Transendothelial flux
HUV-EC-C (1 × 105 cells) and primary HUVECs (1 × 105 cells) were cultured to confluence on tissue-culture Transwell plates (polycarbonate membrane, 12-mm diameter, 0.4-μM pore size; Becton Dickinson Labware, Bedford, MA), as described.6,7 Culture medium was replaced with colorless Hanks balanced salt solution (HBSS) supplemented with 5% FBS and gentamycin (0.05 mg/mL). Experimental wells were treated with LPS (175 ng/mL) in the presence or absence of C1INH (150 μg/mL). Control wells were treated with either C1INH (150 μg/mL) or PBS alone. Evans blue dye (20 μL of 0.5% wt/vol) was added to the upper compartment following the addition of the LPS. The liquid was collected from the lower wells after 30 and 60 minutes, and permeability measured spectrophotometrically at 630 nm.
Endothelial cell detachment. HUV-EC-C (1 × 105 cells) and primary HUVECs (1 × 105 cells) were cultured in 24-well plates from Becton Dickinson Labware with endothelial cell basal medium and endothelial cell growth medium (1 mL) containing 5% FBS and gentamycin (0.05 mg/mL) for 72 hours. Following treatment with LPS (175 ng/mL) in the absence or the presence of C1INH (150 μg/mL) for 4 hours, 1 mL of the supernatant medium and 1 mL of the wash medium from each well were collected. The remaining cells were detached with trypsin (1 mL of 0.5 mg/mL) for 15 minutes. The cells were stained with 0.4% Trypan Blue (Invitrogen, Carlsbad, CA) and then counted in triplicate. Percentage of detachment was expressed as (total number of cells in the supernatant and wash)/(total number of cells in the supernatant and the wash, plus those cells detached from the plate by trypsin) × 100%.5,16
Analysis of apoptosis
HUVECs (1 × 105) treated with LPS (175 ng/mL) in the presence or absence of C1INH (150 μg/mL) for 0, 1, 2, and 4 h and harvested with a cell scraper from treated monolayers were centrifuged (200g, 5 min) and resuspended in PBS (200 μL). DNA was isolated using the Apoptotic DNA Ladder Kit. Isolated DNA was incubated with DNase-free RNase (2 μg/mL) for 20 minutes at room temperature and resolved on a 1.5% agarose gel containing 0.5 μg/mL ethidium bromide. Annexin V binding was analyzed by fluorescence-activated cell sorting (FACS). HUVECs (1 × 105 cells) were incubated with LPS (175 ng/mL) in the presence or absence of C1INH (150 μg/mL) at 37°C for 0, 1, 2, and 4 hours. The cells were incubated with FITC-conjugated annexin V for 1 hour at room temperature and then fixed with FACS solution. The positive cells stained with FITC-conjugated annexin V were analyzed on a FACS Calibur using CellQuest software (Becton Dickinson, San Jose, CA).
Laser scanning confocal microscopy
HUVECs (1 × 105) were cultured in 8-well culture slides from Becton Dickinson Labware, incubated for 48 hours, and then incubated with FITC-LPS (175 ng/mL) for 10, 15, 30, 60, 120, and 180 minutes in the absence or presence of C1INH (150 μg/mL). The cells were stained with AlexaFluor 488–conjugated donkey anti–mouse IgG (Molecular Probes, Eugene, OR). After extensive washing with I × PBS, slides were mounted with ProLong anti-fade medium (Molecular Probes). Confocal microscopy was performed on an Olympus BX 50 WI microscope (Olympus, Melville, NY) coupled with a TI:Sapphire laser (Spectraphysics, Irvine, CA) and a Radiance 2000MP scanning confocal multiphoton imaging system (BioRad Laboratories, Hercules, CA). The microscope was equipped with an Olympus UPlanApo 60 ×/1.20 objective lens controlled by Lasersharp 2000 acquisition software (BioRad); images were taken at room temperature. Adobe Photoshop 6.0 software (Adobe, San Jose, CA) was used for subsequent image processing.
Statistical analysis
Data were analyzed using the Mann-Whitney test. All the experimental data were presented as mean ± standard deviation (SD). A P value of less than .05 was considered significant.
Results
The effect of C1INH on LPS-induced in vitro transendothelial flux and endothelial detachment
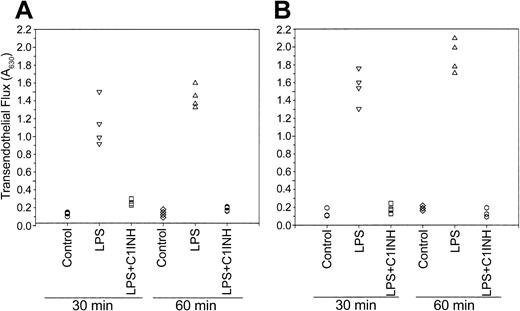
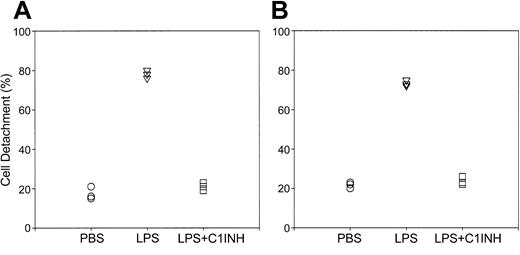
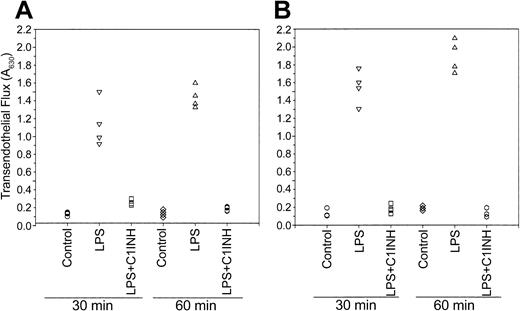
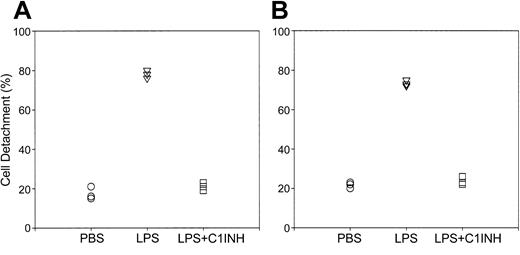
The endothelial cell lining of the vasculature is the first host tissue barrier encountered by circulating LPS. The alteration in endothelial cells induced by LPS is accompanied by gap formation between adjacent cells and cell detachment, which results in endothelial barrier dysfunction and increased vascular endothelial permeability.5,6,16 To determine whether C1INH blocked LPS-induced endothelial barrier disruption and plasma leakage, we investigated in vitro transendothelial flux in response to LPS in the presence and absence of C1INH. Following the addition of LPS (175 ng/mL) to cultured HUV-EC-C (Figure 1A) or to primary HUVECs (Figure 1B), dye leakage had increased by 30 minutes and did not appear to change further by 60 minutes. Treatment with C1INH (150 μg/mL) reduced LPS-induced transendothelial flux (Figure 1). In the case of HUV-EC-C, following exposure to LPS (175 ng/mL), the percentage of detached cells increased from 17.6% ± 3.4% to 78.8% ± 1.6%, but when treated with C1INH (150 μg/mL), cell detachment remained at 21.4% ± 2.1% (Figure 2A). The reaction of the primary HUVECs to LPS exposure and to treatment with C1INH was essentially identical to that of the endothelial cell line; detachment increased from 21.7% ± 1.53% to 73.3% ± 1.53% in the presence of LPS and was only 23.7% ± 2.08% with C1INH treatment of LPS-exposed cells (Figure 2B). These studies demonstrate that C1INH, in tissue culture, reduces LPS-induced vascular endothelial cell injury.
The effect of C1INH on LPS-induced in vitro transendothelial flux. The HUVEC cell line HUV-EC-C (A) and primary HUVECs (B) were cultured in Transwell plates and treated with LPS (175 ng/mL), either alone or in the presence of C1INH (150 μg/mL). Control HUVEC cultures were treated with PBS alone as the control. Evans blue dye (20 μL, 0.5%) was added to the upper compartment and absorbance of the medium in the lower compartment was measured at 630 nm.
The effect of C1INH on LPS-induced in vitro transendothelial flux. The HUVEC cell line HUV-EC-C (A) and primary HUVECs (B) were cultured in Transwell plates and treated with LPS (175 ng/mL), either alone or in the presence of C1INH (150 μg/mL). Control HUVEC cultures were treated with PBS alone as the control. Evans blue dye (20 μL, 0.5%) was added to the upper compartment and absorbance of the medium in the lower compartment was measured at 630 nm.
The effect of C1INH on LPS-induced endothelial cell detachment in vitro. The cell line HUV-EC-C (A) and primary HUVECs (B) were incubated with LPS (175 ng/mL) in the absence (▿) or presence of C1INH (150 μg/mL; □). Control cultures were treated with PBS alone (○). The cells in the supernatant and wash, as well as those detached from the filter with trypsin were stained with 0.4% Trypan Blue and counted. The percentage of cell detachment was calculated as described in “Materials and methods.”
The effect of C1INH on LPS-induced endothelial cell detachment in vitro. The cell line HUV-EC-C (A) and primary HUVECs (B) were incubated with LPS (175 ng/mL) in the absence (▿) or presence of C1INH (150 μg/mL; □). Control cultures were treated with PBS alone (○). The cells in the supernatant and wash, as well as those detached from the filter with trypsin were stained with 0.4% Trypan Blue and counted. The percentage of cell detachment was calculated as described in “Materials and methods.”
C1INH blocks LPS-induced endothelial cell apoptosis
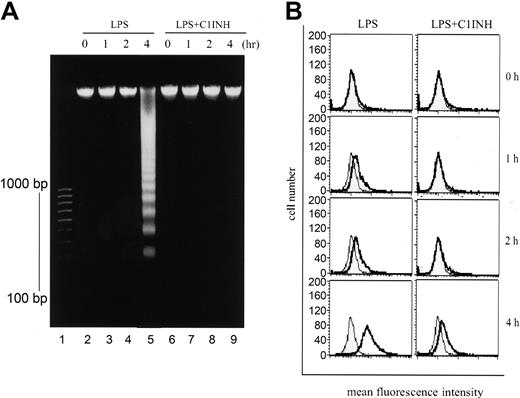
LPS is a key proinflammatory mediator and potent activator of the vascular endothelium that can induce endothelial cell apoptosis, an event that may contribute to the pathogenesis of sepsis and its attendant complications.10,20 We investigated whether C1INH prevented LPS-induced apoptosis of endothelial cells. HUVECs were exposed to LPS (175 ng/mL) for 0, 1, 2, and 4 hours in the presence or absence of C1INH (150 μg/mL). DNA from these cells was analyzed by agarose gel electrophoresis for DNA fragmentation and the cells were examined by FACS for the binding of FITC-annexin. In agarose gel electrophoresis, DNA ladder formation consistent with the typical DNA fragmentation associated with apoptosis was identified following LPS exposure for 4 hours (Figure 3A). C1INH (150 μg/mL) completely suppressed this change. The early molecular events in apoptosis include translocation of phosphatidylserine from the interior to the exterior of the cell membrane. HUVECs exposed to LPS in the presence or absence of C1INH was analyzed using FACS for the binding of FITC-conjugated annexin V to phosphotidylserine on the surface of the cells as a measure of apoptosis (Figure 3B). LPS (175 ng/mL) led to a maximum shift in fluorescence intensity at 4 hours. C1INH (150 μg/mL) markedly suppressed this shift. These data indicate that C1INH suppresses LPS-mediated apoptosis in HUVECs.
The effect of C1INH on LPS-induced endothelial cell apoptosis. HUVECs were incubated with LPS (175 ng/mL) in the presence or absence of C1INH (150 μg/mL). (A) Isolated DNA from HUVECs was resolved on a 1.5% agarose gel and stained with ethidium bromide, and was then visualized by ultraviolet (UV) light. DNAmolecular weight markers, expressed as base pair (bp), are indicated to the left of lane 1 on the gel. (B) The binding of FITC-conjugated annexin V to apoptotic cells was analyzed on a FACS Calibur (FITC–annexin V binding, thick line; control, shaded field).
The effect of C1INH on LPS-induced endothelial cell apoptosis. HUVECs were incubated with LPS (175 ng/mL) in the presence or absence of C1INH (150 μg/mL). (A) Isolated DNA from HUVECs was resolved on a 1.5% agarose gel and stained with ethidium bromide, and was then visualized by ultraviolet (UV) light. DNAmolecular weight markers, expressed as base pair (bp), are indicated to the left of lane 1 on the gel. (B) The binding of FITC-conjugated annexin V to apoptotic cells was analyzed on a FACS Calibur (FITC–annexin V binding, thick line; control, shaded field).
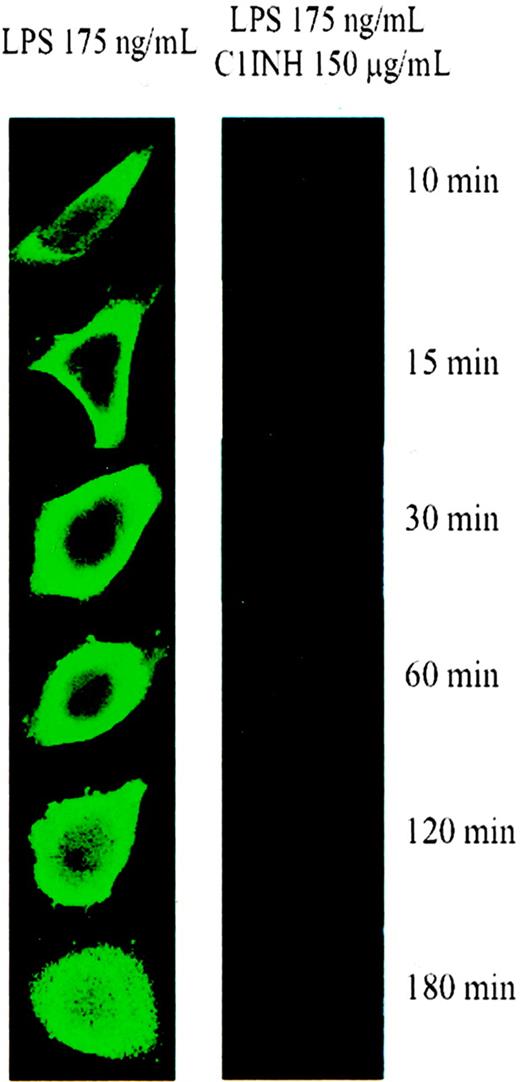
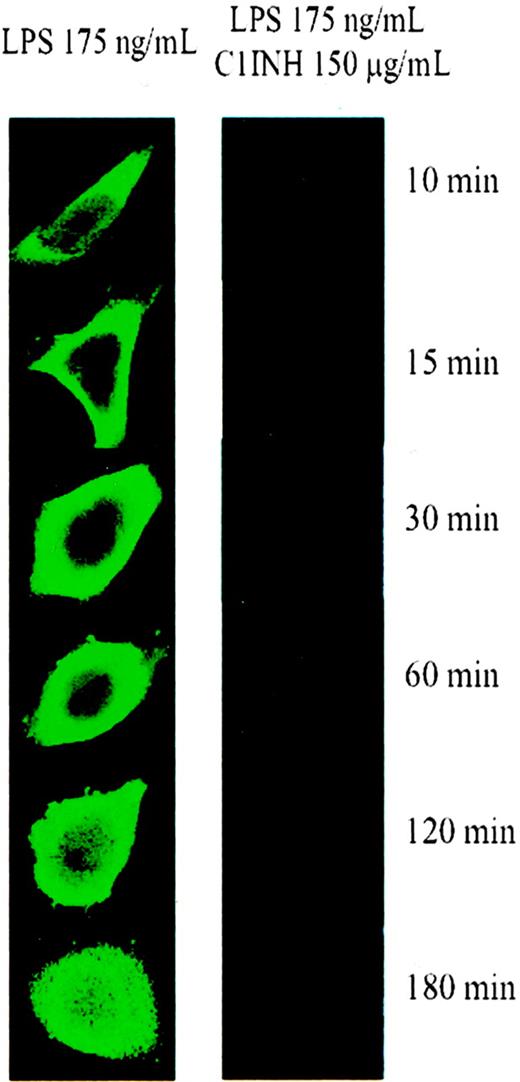
To characterize the LPS-induced morphologic changes, HUVECs were incubated with FITC-LPS (175 ng/mL) for 10 to 180 minutes. When incubated for more than 15 to 30 minutes, the fluorescent intensity on the surface of the cells increased. In addition, cell shape changed during the incubation period, with the cells becoming more rounded (Figure 4A). C1INH (150 μg/mL) completely blocked FITC-LPS (175 ng/mL) binding to the cells (Figure 4B). This suggests that the previously characterized C1INH-endotoxin interaction prevents the binding of LPS to the endothelial cell surface.24
Binding of FITC-labeled LPS to endothelial cells. HUVECs were incubated with FITC-LPS (175 ng/mL) for 10, 15, 30, 60, 120, and 180 minutes in the absence (left column) and in the presence (right column) of C1INH (150 μg/mL) and then were examined using laser scanning confocal microscopy.
Binding of FITC-labeled LPS to endothelial cells. HUVECs were incubated with FITC-LPS (175 ng/mL) for 10, 15, 30, 60, 120, and 180 minutes in the absence (left column) and in the presence (right column) of C1INH (150 μg/mL) and then were examined using laser scanning confocal microscopy.
C1INH protects against LPS-induced local increased vascular permeability in the skin of mice
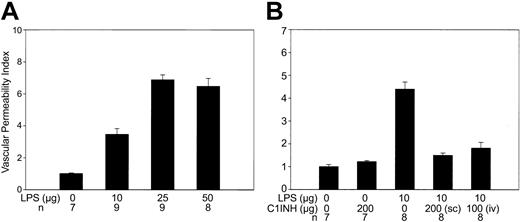
C57BL/6J mice were injected subcutaneously with LPS (0, 10, 25, and 50 μg/site) 5 minutes after intravenous injection of Chicago sky blue dye. LPS (10 μg) increased the vascular permeability index 3-fold compared with control sites injected with PBS (P = .002) (Figure 5A). LPS at doses of 25 and 50 μg/site each increased the vascular permeability index approximately 6- to 7-fold (P = .0002 and .0003, respectively). Subcutaneous administration of a mixture of LPS (10 μg) with C1INH (200 μg) reduced vascular permeability by approximately two-thirds (P = .0002) compared with untreated LPS-induced mice (Figure 5B). In addition, intravenous administration of C1INH (200 μg) suppressed the LPS-induced plasma leakage by one-half (P = .0002; Figure 5B).
C1INH protects C57BL/6J mice from increased cutaneous vascular permeability in response to local LPS injection. (A) C57BL/6J mice were given subcutaneous injections of LPS at the indicated doses in the abdominal skin (n = 9 with the 10 μg dose, 9 with 25 μg, and 8 with 50 μg). Control mice were injected with PBS alone (n = 7). (B) Mice were injected subcutaneously in the abdominal skin with LPS (10 μg) alone (n = 8), a mixture of LPS (10 μg) with C1INH (200 μg; n = 8) (SC), or LPS (10 μg) subcutaneously with an intravenous dose of C1INH (200 μg; n = 8)(IV). Control mice were injected with PBS (n = 7) or with C1INH (n = 7) alone. Experimental data were presented as means ± standard deviation using GraphPad Prism 3.0 software (GraphPad Software, San Diego, CA).
C1INH protects C57BL/6J mice from increased cutaneous vascular permeability in response to local LPS injection. (A) C57BL/6J mice were given subcutaneous injections of LPS at the indicated doses in the abdominal skin (n = 9 with the 10 μg dose, 9 with 25 μg, and 8 with 50 μg). Control mice were injected with PBS alone (n = 7). (B) Mice were injected subcutaneously in the abdominal skin with LPS (10 μg) alone (n = 8), a mixture of LPS (10 μg) with C1INH (200 μg; n = 8) (SC), or LPS (10 μg) subcutaneously with an intravenous dose of C1INH (200 μg; n = 8)(IV). Control mice were injected with PBS (n = 7) or with C1INH (n = 7) alone. Experimental data were presented as means ± standard deviation using GraphPad Prism 3.0 software (GraphPad Software, San Diego, CA).
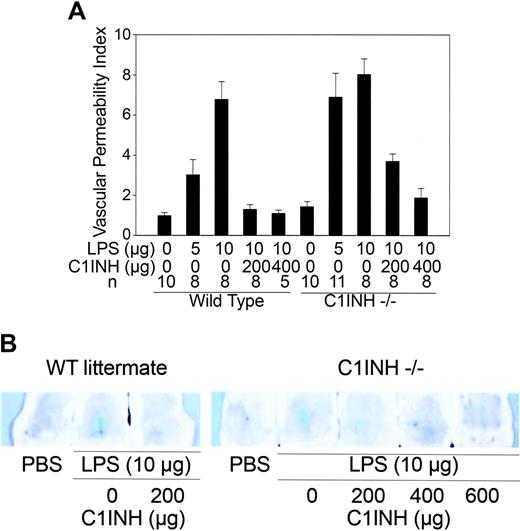
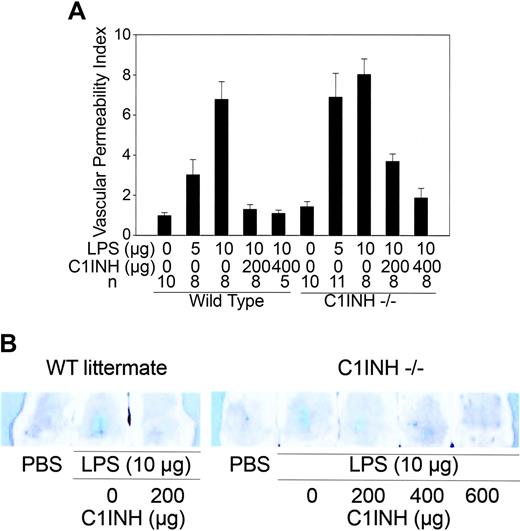
To further analyze the role of C1INH in the vascular permeability response to endotoxin, we compared the response of C1INH-deficient mice to that of wild-type littermates following subcutaneous injection of LPS. C1INH-deficient mice were injected with different concentrations of LPS (0, 5, and 10 μgin100 μL PBS). In response to 5 μg LPS, the vascular permeability index was significantly higher in C1INH-deficient mice than in their wild-type littermates (P = .02; Figure 6A). However, with 10 μg LPS, no significant difference was detected. When treated with C1INH (200 μg intravenously), the vascular permeability index induced by LPS (10 μg) in the C1INH-deficient mice was reduced by approximately 50%, while that of wild-type littermates was reduced by 80% (P = .0003; Figure 6). C1INH at doses of 400 and 600 μg, however, reduced the vascular permeability response of the C1INH-/- mice to levels comparable to the reduction achieved with 200 μg in the wild-type mice. These data suggest that C1INH may play an important role in the regulation of vascular permeability after LPS challenge.
C1INH-deficient mice are more susceptible to local subcutaneous injection of LPS. C1INH-/- or C1INH+/+ littermate mice were given subcutaneous injections of LPS, with or without C1INH, in the abdominal skin. (A) C1INH-/- (right) and wild-type littermate (left) mice were injected subcutaneously with LPS (5 or 10 μg), either alone or following intravenous C1INH (200 and 400 μg). Control mice were injected with PBS alone. The numbers of mice in each experimental group were as indicated in the figure. (B) Photographs of the abdominal skin of the wild-type littermate (top) and the C1INH-/- mice (bottom) showing the leakage of the dye at the site of subcutaneous injection of LPS and its inhibition when the mouse was treated with intravenous C1INH. Experimental data were presented as means ± standard deviations using GraphPad Prism 3.0 software.
C1INH-deficient mice are more susceptible to local subcutaneous injection of LPS. C1INH-/- or C1INH+/+ littermate mice were given subcutaneous injections of LPS, with or without C1INH, in the abdominal skin. (A) C1INH-/- (right) and wild-type littermate (left) mice were injected subcutaneously with LPS (5 or 10 μg), either alone or following intravenous C1INH (200 and 400 μg). Control mice were injected with PBS alone. The numbers of mice in each experimental group were as indicated in the figure. (B) Photographs of the abdominal skin of the wild-type littermate (top) and the C1INH-/- mice (bottom) showing the leakage of the dye at the site of subcutaneous injection of LPS and its inhibition when the mouse was treated with intravenous C1INH. Experimental data were presented as means ± standard deviations using GraphPad Prism 3.0 software.
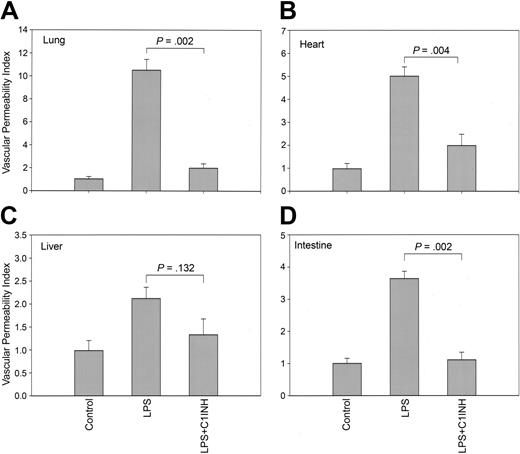
C1INH suppresses the systemic LPS-induced increase in microvascular permeability in mice
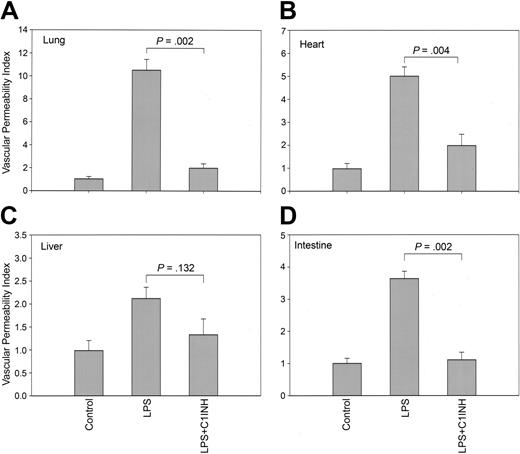
C57BL/6J mice were injected with a lethal dose of LPS (20 mg/kg), either in the presence or absence of C1INH (200 μg intraperitoneally).24 Vascular permeability was evaluated 5 hours after a lethal dose of LPS administration. Challenge with LPS resulted in approximately 10-, 5-, 2-, and 4-fold increases in the microvascular permeability index in lungs, heart, liver, and intestine, respectively. Treatment with C1INH resulted in significant reductions of permeability in the lung, heart, and intestine (Figure 7). These studies indicate that C1INH suppresses LPS-induced microvascular permeability in multiple organs.
C1INH suppressed the increase in microvascular permeability in mice in response to systemic administration of LPS. C57BL/6J mice were injected with LPS (20 μg/kg per mouse, intraperitoneally) in the absence of C1INH (n = 6; 200 μg per mouse, intravenously). Control mice were injected with PBS (n = 6). The microvascular endothelial permeability index in the lungs (A), heart (B), liver (C), and intestine (D) were determined, respectively.
C1INH suppressed the increase in microvascular permeability in mice in response to systemic administration of LPS. C57BL/6J mice were injected with LPS (20 μg/kg per mouse, intraperitoneally) in the absence of C1INH (n = 6; 200 μg per mouse, intravenously). Control mice were injected with PBS (n = 6). The microvascular endothelial permeability index in the lungs (A), heart (B), liver (C), and intestine (D) were determined, respectively.
Discussion
A capillary leak syndrome may complicate sepsis and septic shock.28 The molecular mechanisms causing the increased vascular permeability and vasodilation are incompletely understood. Although the vascular pathophysiology associated with Gram-negative sepsis can be explained largely by mediation via host responses to LPS, particularly via the induction of increased TNF-α expression,19 LPS may be directly responsible for a portion of the endothelial cell injury.6,7,27 In addition, endothelial damage resulting from interactions with activated neutrophils and/or natural killer cells are likely to be involved. Bradykinin also may play a role. Degradation of bradykinin depends on the activity of angiotension-converting enzyme, which is severely decreased in patients with septic shock and septic adult respiratory distress syndrome. Pretreatment with C1INH has been shown to attenuate endotoxin-induced leukocyte–endothelial cell adhesion and vascular leakage in postcapillary venules of rat mesentery during endotoxemia.29 The mechanism underlying this effect has not been defined. The data described here, combined with previous data, suggest that this effect may be partly the result of the direct interaction of C1INH with endotoxin (Figures 5B, 6A-B).24,25 This interaction blocks the binding of Salmonella typhimurium LPS to macrophages which results in suppression of TNF-α production by these cells. The present data demonstrate that this C1INH-LPS interaction also results in a diminished direct toxic effect of endotoxin on the endothelial cell.24,25 This mechanism very likely is at least partially responsible for C1INH-mediated protection from Gram-negative endotoxin shock in a variety of animal models.24,25,29-36 In addition to suppression of the systemic effects of endotoxin, C1INH also suppresses the direct vascular permeability-enhancing activity of LPS (Figures 1, 5B, 6). Inhibition of activation of the contact and complement systems also may play a role. Finally, based on recently published data, C1INH may interfere directly with leukocyte–endothelial cell adhesion via its ability to interact with endothelial cell E- and P-selectins.37
C1INH also reverses the episodic increased vascular permeability (angioedema) observed in patients with C1INH deficiency (hereditary angioedema). However, clinical data, in vitro data, and in vivo data from the analysis of C1INH-deficient mice indicate that the increased vascular permeability in this condition is mediated by bradykinin, which is released from high-molecular-weight kininogen by cleavage with plasma kallikrein as a result of contact system activation.26,38-42 C1INH is the primary plasma inhibitor of the 2 proteases activated during contact system activation, coagulation factor XIIa and plasma kallikrein. The mechanism of angioedema in this situation is less complex than is the increased vascular permeability induced by endotoxin. However, as referred to in the first paragraph of “Discussion,” it is likely that, in vivo, contact system activation, in addition to the TNF-α–mediated and direct endotoxin effects, might be involved. C1INH, therefore, may play multiple roles in suppression of increased vascular permeability mediated by LPS.
The endothelial cell response to LPS includes monolayer barrier dysfunction, cell detachment from the underlying extracellular matrix, and induction of endothelial cell apoptosis. In the studies described here, LPS induced characteristic morphologic changes in HUVECs (Figure 4). These changes were reversed by C1INH. LPS induces apoptosis in vitro and in vivo, which may contribute to the pathophysiology of septic shock. Apoptotic endothelial cells have been detected in murine models of sepsis.43,44 In vivo, TNF-α appears to be the major mediator of apoptosis,19 although previous in vitro data and the data shown in Figure 3 indicate that endotoxin also can induce apoptosis directly.10,16,20 Other cytokines (eg, IL-1, IL-8), proteases, various vasoactive compounds (eg, bradykinin, histamine, endothelin-1), growth factors, and complement activation products (eg, C3a, C5a) are also endothelial agonists.45 Caspase inhibition blocked LPS-induced cleavage of adherens junction proteins, which are tethered to the actin cytoskeleton, and endothelial cell detachment, but failed to inhibit the LPS-induced increase of transendothelial 14C–bovine serum albumin (BSA) flux.16 Protein tyrosine kinase (PTK) inhibition protected against LPS-induced actin depolymerization, opening of the paracellular pathway, loss of barrier function and transendothelial 14C-BSA flux, but did not block cleavage of adherens junction proteins and therefore, did not prevent cell detachment.4,16 On the other hand, C1INH interferes with the interaction of endotoxin with the endothelial cell and, therefore, suppresses all of these responses (Figures 1, 2, 3).
In summary, these studies provide further support for the observation that C1INH has a novel biological role as an anti-inflammatory protein.24,25 In addition to its ability to suppress the systemic effects of endotoxin via inhibition of the interaction of endotoxin with macrophages, it also inhibits the direct effects of LPS on the endothelium, as demonstrated here both in vitro and in vivo. One effect of this inhibition is the prevention of LPS-mediated increased vascular permeability.
Prepublished online as Blood First Edition Paper, November 2, 2004; DOI 10.1182/blood-2004-05-1963.
Supported by Public Health Service grants HD22082 and HD33727 from the National Institute of Child Health and Human Development.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.