Comment on Bakanay et al, page 545
Even treated with hydroxyurea, severe sickle cell anemia has higher mortality than milder disease. Understanding how early in the disease process this treatment can be safely started is now paramount.
The outlook for patients with sickle cell disease has improved, at least in developed countries. Early disease detection, prophylactic penicillin, better supportive care, and greater awareness of severe complications, such as acute chest syndrome, with more skilled treatment, are responsible for increased longevity. The introduction of hydroxyurea treatment with its reduction in morbidity and mortality, associated decreased medical costs, and restored well being should lead to further patient benefits.1,2 Nevertheless, most patients with sickle cell disease reside in lands where death from this disease in early childhood is often the norm, so attention must be paid to moving current advances to developing countries.
Bakanay and colleagues now report their observations from a single clinic that has laudably managed to convince a large number of patients to be treated with hydroxyurea—more than were treated with hydroxyurea in the randomized Multicenter Study of Hydroxyurea (MSH) trial—and show, again, that severe disease with organ damage, severe anemia, and incipient renal failure presages earlier death. Even in the hands of these skilled practitioners, more than 15% of patients died.FIG1
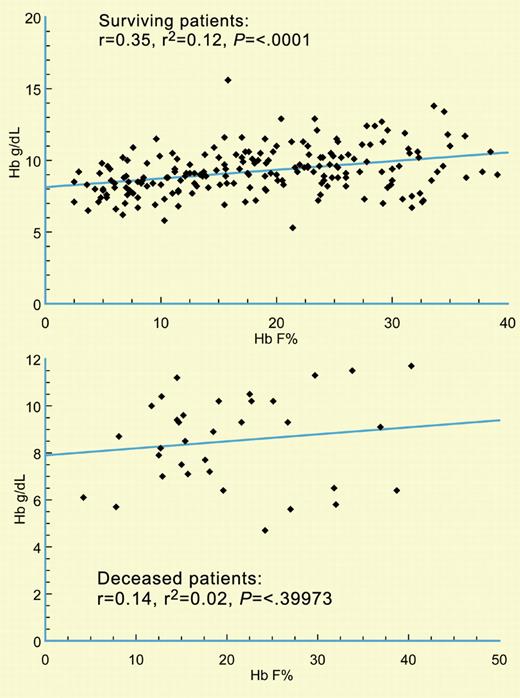
Sickle cell patients surviving during the observation period have a good correlation between the increase in Hb F and total hemoglobin concentration (top) while this relationship is lost in patients who died during the observation period. See the complete figure in the article beginning on page 545.
Sickle cell patients surviving during the observation period have a good correlation between the increase in Hb F and total hemoglobin concentration (top) while this relationship is lost in patients who died during the observation period. See the complete figure in the article beginning on page 545.
I believe that these and other studies in adults and children with sickle cell anemia, which have shown impressive results of treatment with minimal adverse effects, beg answers to the following questions: How early in life can this treatment be safely started? Will early treatment prevent the accumulation of organ damage that appears to explain the death of hydroxyurea-treated adults? Why aren't most eligible adults treated with hydroxyurea? Is hydroxyurea useful in sickle-hemoglobin C (HbSC) disease?
We know that children with sickle cell anemia have a more robust fetal hemoglobin (Hb F) response to treatment than adults. Safely maintaining high Hb F levels from very early life may forestall the pulmonary, renal, cardiac, hematopoietic, and neurologic impairment that typifies adult disease. A study is now in progress that will formally test this notion. Interestingly, among the deceased patients in Bakanay et al's study, an increment in Hb F was not always reflected in higher hemoglobin levels. Perhaps this is a result of increased organ damage.
If competently used—that is, patients cannot be given a fixed dose and asked to return in 6 months for a new prescription—hydroxyurea usually has important clinical benefits.3 The problem is that despite its ample benefits and apparent safety observed during more than 10 years of use in sickle cell anemia, only a fraction of patients who might benefit from hydroxyurea receive it. Whether this paradox is due to physician reluctance to use the drug or lack of patient acceptance is unclear but a worthy topic for study so that an efficacious therapy can benefit more of the population at risk.
Hydroxyurea has been studied most intensively in homozygotes for the HbS gene (sickle cell anemia). While it is also effective in HbS-β thalassemia,4 few studies have been done in HbSC disease, a genotype almost as common as sickle cell anemia with a similar profile of complications.
Even when given by a capable practitioner and faithfully taken, all patients do not have a good Hb F response so a search for additional Hb F–inducing drugs must continue.5 ▪