In recent years, several groups including ours have reported on the feasibility of allografting debilitated or advanced-aged patients using reduced intensity conditioning (RIC) regimens.1-6 However, because of the heterogeneity in the study populations, information on the efficacy of RIC transplantations from unrelated donors to control high-risk/active elderly acute myeloid leukemia (AML)/myelodysplastic syndrome (MDS) has remained limited.
We focused on a homogenous group of 34 consecutive older patients (≥ 60 years) with high-risk, active AML/MDS (28 patients with AML; 6 with MDS) allografted from unrelated donors after conditioning with a uniform RIC regimen and receiving a uniform graft-versus-host disease (GvHD) prophylaxis (cyclosporine, mycophenolate mofetil, rabbit anti–T-lymphocyte globulin [ATG] [Fresenius, Graefelfing, Germany] 20 mg/kg per day at day -1 to day -2). The preparative regimen consisted of fludarabine (30 mg/m2 per day at day –9 to day –5) combined with 2 alkylating agents given in moderate doses (BCNU [1,3-bis(2-chloroethyl)-1-nitrosourea] 150 mg/m2 per day at day –7 to day –6; melphalan 110 mg/m2 at day –4) (FBM). Detailed information of patient characteristics and transplantation outcomes are given in Tables 1 and 2.
The high rates of sustained engraftment (100%), early full donor chimerism (97%), and blast clearance (100% patients achieved CR) obtained underscore the myeloablative character and the high antileukemic potential of the FBM/ATG/peripheral blood–hematopoietic cell transplantation (PB-HCT) strategy.
Of note, at HCT 91% of patients had active disease and 38% of patients had uncontrolled AML after a median of 2 intensive chemotherapies. On the other hand, the FBM regimen was tolerated fairly well and the procedure is relatively safe since nonrelapse mortality (NRM) was low (6 deaths; 2-year cumulative risk, 19.6% [95% CI, 9.5%-40.4%]) and mainly due to fungal infections (3 early deaths), and therefore principally related to the pretransplantation state of the patient (long neutropenia, history of aspergillosis). To avoid this complication, transplantation early during the disease course would be an option.
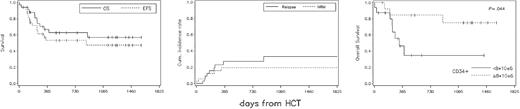
The incidence of acute and chronic GvHD was comparable with that reported in younger patients. On median day +170, 9 patients relapsed (2-year cumulative relapse risk, 27.3% [95% CI, 15%-49.7%]). Of 7 relapsed patients, 3 responded to donor lymphocyte infusions (DLIs) and 2 patients overall were successfully salvaged (1 with DLI, 1 with second HCT). After a median follow-up of 913 days (range, 55-1591 days), 22 patients (65%) are alive with all but 1 in complete remission (CR). Most of the survivors report feeling well (median Karnofsky performance score [KPS], 100%; 70-100), with only 2 patients requiring chronic immunosuppression. The actuarial 2-year overall survival (OS) and event-free survival (EFS) probability were 62.7% (95% CI, 44.9%-80.4%) and 53.1% (95% CI, 34.8%-71.4%), respectively (Figure 1). Interestingly, higher numbers of CD34+ cells in the PB graft were associated with improved outcome (P = .044). This correlation could not be explained by a higher incidence of chronic GvHD with increasing numbers of CD34+ PB cells, as suggested by others.7 Since age affects CD34+ cell yield during apheresis, it seems reasonable to consider lower age as a selection criterion when choosing a donor.
Allogeneic PB-HCT from unrelated donors using the FBM/ATG protocol is an effective treatment for patients 60 years or older with high-risk myeloid malignancies. The sustained remissions observed in 7 of 11 previously untreated sAML (AML secondary to MDS) or MDS patients suggest that at least for candidates with a slow increase of blasts over time, transplantation may be used as a front-line therapy.