Abstract
To determine the prevalence of Helicobacter pylori (H pylori) infection in North American patients with immune thrombocytopenic purpura (ITP) and the effect of H pylori eradication on the platelet count, a prospective study was performed. Seventy-four patients aged 10 years and older (mean age of 41 years) with chronic ITP and a platelet count below 60 × 109/L were enrolled. H pylori infection was found in 22% of patients by means of a breath test and could not be predicted by gastrointestinal symptoms. H pylori–positive patients (52.5 years of age) were older than H pylori–negative patients (38.5 years of age; P = .0035). Fifteen of the 16 H pylori–positive patients were treated and the bacteria was eradicated in 14 (93%). After 3 months, a significant response (platelet count > 50 × 109/L and doubling the initial count) was observed in only one patient. After a median follow-up of 11.5 months, none of the 14 patients had responded. Ten H pylori–negative patients treated with the same regimen also did not increase their platelet counts. In conclusion, unlike several previous reports, this study does not implicate H pylori in the pathogenesis of ITP since the prevalence of H pylori infection was low and eradication of H pylori did not positively influence the course of the ITP.
Introduction
Helicobacter pylori (H pylori), a ubiquitous Gram-positive bacterium, was initially discovered in 1982 as an infectious cause of peptic ulcers. Following discovery of its causative role in gastritis and peptic ulcer disease, subsequent studies implicated H pylori in the pathogenesis of gastric adenocarcinoma and mucosa-associated lymphoid tissue (MALT) lymphoma. More recently, H pylori has been suspected to be involved in various autoimmune disorders including pernicious anemia and immune thrombocytopenic purpura (ITP).1-8
In 1998, Gasbarrini et al2 reported a substantial increase in the platelet count in all 8 H pylori–positive adults with immune thrombocytopenic purpura (ITP) in whom H pylori was eradicated. Subsequent uncontrolled studies from Italy3-5 and Japan6-8 all showed an apparently higher-than-expected prevalence of H pylori9,10 in patients with ITP. Furthermore, 38%7 to 73%4 of H pylori–positive patients with ITP achieved a partial or complete platelet recovery after H pylori eradication. On the other hand, additional studies have not supported a role for H pylori in ITP. The prevalence of H pylori infection was not increased in French patients with ITP when compared with age-matched controls,11 and while the prevalence of H pylori was high, no significant improvement of the platelet count was observed after H pylori eradication in a report from Spain.12
We therefore conducted a prospective study to assess the prevalence of H pylori infection in North American patients with ITP and the efficacy of H pylori eradication on the platelet count. If eradication of H pylori was not achieved with the initial regimen, treatment was pursued with alternative regimens. To determine if the H pylori eradication regimen could have nonspecific effects on the platelet count, 10 ITP patients whose H pylori test was negative were also treated with the same eradication regimen. In addition, a short questionnaire was completed by the patients at the time of testing to see if H pylori–infected patients with ITP could be identified by symptoms referable to their gastrointestinal (GI) tract.
Patients, materials, and methods
Patients
All patients with ITP, defined according to the criteria set forth in the American Society of Hematology (ASH) Guidelines,13 who attended the Weill-Cornell center over the 12 month study period were eligible to enroll in this study if they fulfilled the following inclusion criteria: age of 10 years and older, a platelet count of less than 60 × 109/L within 2 weeks of H pylori testing, and no knowledge of a positive HIV test. Patients who were treated by immunosuppressive treatments or other drugs for their ITP at the time of inclusion were eligible if the doses of the ongoing medications were stable for at least 4 weeks before inclusion. After inclusion, both intravenous immunoglobulins (IVIg's) and intravenous anti-D (IV anti-D) were allowed as a rescue therapy if clinically required (ie, very low platelet count, grade III or IV bleeding symptoms, or scheduled invasive procedures). Patients were not eligible for the study if they had been treated for H pylori within 2 years or if they had been treated with either an antibiotic, lansoprazole (or another proton pump inhibitor), or bismuth within the past 4 weeks.
In order to see if the status of H pylori could be predicted by gastrointestinal symptoms or past medical history, all patients were asked to complete a short standardized questionnaire at the time of the breath test (Table 1).
Approval for this study was obtained from the Institutional Review Board of the New York Hospital–Cornell Medical Center and informed consent was provided by all subjects or their parents according to the Declaration of Helsinki. Patients 10 to 18 years of age provided their assent.
H pyloriinfection testing
All enrolled patients underwent at time of inclusion a BreathTek Urea breath test commercially available from Prometheus (San Diego, CA). In H pylori–positive patients, eradication was assessed by another urea breath test performed 1 to 2 months after completion of treatment. Patients not responding to eradication treatment had a third test performed after a subsequent treatment regimen was completed. The breath test initially required a 4-hour fast before it could be performed. This led several otherwise eligible patients to decline to participate.
H pylorieradication regimen
Patients infected with H pylori were treated according to a standard H pylori treatment protocol currently in use in the United States (referred to as the Prevpac, TAP Pharmaceutical Products, Lake Forest, IL). For patients older than 12 years of age, this consisted of lansoprazole 30 mg, clarithromycin 500 mg, and amoxicillin 1000 mg taken together twice a day for 2 weeks. Children 10 to 12 years of age received lansoprazole 30-mg capsules, clarithromycin tablets at a dose of 15 mg/kg/day to a maximum dose of 500 mg/day, and amoxicillin 500-mg tablets at a dose of 45 mg/kg/day to a maximum dose of 1000 mg/day. The penicillin-allergic patients were not given amoxicillin. If H pylori was not eradicated after initial treatment, the patient was referred to the study gastroenterologist (C.F.) to determine an alternative therapy.
Control groups
To see if there was an effect on the platelet count after the Prevpac administration, all of the initial patients enrolled began treatment “blindly” at the time of the breath test screening before the results had returned. After 10 patients whose H pylori test was subsequently found to be negative had been treated (ITP treatment control group), only patients whose breath test was positive received the Prevpac. Nine of the 10 control patients received the Prevpac; 1 was penicillin allergic. In order to compare the prevalence of H pylori infection in our population of ITP patients to the prevalence in healthy individuals, recent epidemiologic data available in a North American population14,15 was used.
Monitoring
As a minimum, platelet counts were performed at the time of testing, within 2 weeks of breath screening, once every 2 weeks for the first 8 weeks, and every 4 weeks for the next 4 months.
Response criteria
A complete response (CR) was defined as the achievement of a platelet count of at least 150 000/μL within 3 months (13 weeks) after completion of H pylori eradication therapy. Partial response (PR) was defined as a platelet count above 50 × 109/L and at least a doubling of the initial count. Patients considered at bleeding risk during the study period who required active treatment (higher doses of steroids, IVIg or IV anti-D) more than 8 weeks after the eradication treatment were considered as nonresponders.
Analysis
Data were expressed as mean ± standard deviation (SD) or as median (range). A chi-square or Fischer exact test were used for analysis of categoric data; the t test was used to compare groups in which the data involved continuous variables. A 2-tailed P value of less than .05 was considered significant; probabilities of .05 to .10 were considered a trend.
Results
Patient characteristics
Seventy-four consecutive consenting patients, including 50 women (67.5%) and 24 men, with a mean age of 41 years (SD ± 18.3) fulfilling the inclusion criteria were enrolled and tested for the presence of H pylori. Sixty-three of the 74 patients (85%) were white, 7 (9.5%) were Hispanic, 3 (4%) were Asian, and 1 patient was African American.
Sixty-four (90%) of the enrolled patients had chronic ITP (ie, duration > 6 months) and 21 (28%) had previously undergone splenectomy.
Prevalence of H pylori infection
Sixteen of the 74 patients (21.6%) had a positive breath test. This rate of infection was lower than the prevalence of 32.5% assessed in 7465 healthy adults in the US population by means of serology14 (P = .04).
H pylori–positive patient characteristics
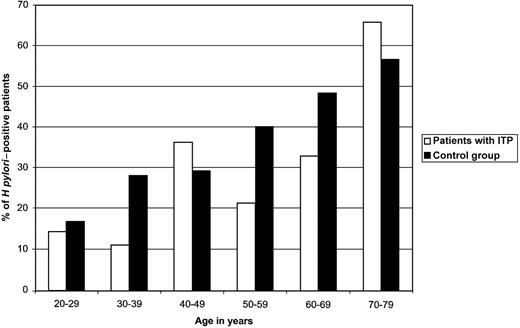
As expected, increased age was associated with a higher likelihood of H Pylori infection in both the healthy controls14 and the ITP patients (Figure 1). The mean age of the H pylori–positive patients (52.5 years, SD ± 15.9) was higher than the mean age of the H pylori–negative patients (38.5 years, SD ± 18.3; P = .0035). Although there was a trend for a longer duration of ITP in H pylori–positive patients (10.2 years versus 6.4 years in H pylori–negative patients; P = .07), only the mean age was significantly different when H pylori–positive and –negative patients were compared (Table 2).
Age distribution of H pylori infection. The rate (%) of H pylori infection according to age (≥ 20 years) found in patients with ITP and in 7465 healthy adults in the United States.14 Although the methods of diagnosis used in the 2 groups were different (ie, breath test in the ITP group and serology in the study from Everhart et al14 ), the likelihood of H pylori infection increased with age in both cases.
Age distribution of H pylori infection. The rate (%) of H pylori infection according to age (≥ 20 years) found in patients with ITP and in 7465 healthy adults in the United States.14 Although the methods of diagnosis used in the 2 groups were different (ie, breath test in the ITP group and serology in the study from Everhart et al14 ), the likelihood of H pylori infection increased with age in both cases.
Patients completed a questionnaire of GI symptoms to see if this would predict which patients were infected. There was a trend for patients with heartburn and gas or burping to be H pylori infected (Table 1).
Eradication ofH pylori
The 16 H pylori–positive patients all had chronic ITP and 15 had been previously treated for their ITP by 1 to 6 therapies including splenectomy in 5 (Table 3). Since 1 patient had her platelet count return to normal prior to beginning treatment of H pylori, only 15 of the 16 H pylori–positive patients were treated. Fourteen patients received the Prevpac, one patient who was allergic to penicillin was first treated with clarithromycin and lansoprazole. Overall, H pylori was successfully eradicated in 14 of the 15 patients (93%). The H pylori was allowed to persist in a 74-year-old woman whose platelet count was stably greater than 50 × 109/L; she did not respond to the Prevpac and then developed diarrhea and vomiting during alternative treatment with metronidazole and doxycyclin.
Platelet outcome in H pylori–positive patients
The median follow-up of infected patients was 11.5 months (range, 3-18 months; Table 3). Three months after the treatment, the time point at which responses were seen in other studies, a significant increase of platelet count was observed in only one patient (patient no.12; Table 3). However, since the patient had a chronic relapsing ITP, the role of the Prevpac was difficult to ascertain. Moreover, after 7 months of follow-up, her platelet count was 53 × 109/L; a breath test was not performed at time of relapse. In another case (no. 13) in which no platelet change was seen at 3 months, mycophenolate mofetil and cyclosporin were begun and at 6 months the count was 100 000/μL. In total, 11 of the 15 patients (73%) required changes in their baseline treatment within 6 months after receiving the eradication regimen (Table 3).
Platelet outcome in H pylori–negative patients
After 3 months of follow-up, no significant increase in the platelet count was observed in any of the 9 consecutive H pylori–negative patients who were treated by the Prevpac or the one receiving an alternative regimen (Table 4). The increase in the platelet count observed in patient no. 5 was likely to be a consequence of the administration of mycophenolate mofetil that was started a month before for an underling systemic lupus erythematosus. After 6 months of follow-up, a CR or a PR was achieved in 4 patients (nos. 3, 4, 5, and 8) but in all cases after the initiation of new treatment (Table 4). Patient no. 10 was the only who did not require any change in her baseline ITP treatment after receiving the H pylori eradication regimen (Table 4).
Discussion
Whether the investigation and eradication of H pylori infection should be pursued in patients with ITP is a matter of debate. Infectious agents such as HIV and hepatitis C virus (HCV) may trigger an immune-mediated thrombocytopenia and/or cause it to persist13 while other viruses resulting in chronic infections, such as human T-cell lymphoma/leukemia virus 1 (HTLV-1), do not seem to have this effect.16 Recent studies in primarily Italian and Japanese populations2-8 have suggested that H pylori could initiate and perpetuate ITP. Initiation would be suggested by an increased mutual coincidence of H pylori and ITP over that observed in the general population. Perpetuation would be suggested by amelioration of ITP as a result of H pylori eradication. In the studies cited above, although approximately half of the patients in whom H pylori was eradicated did not change their platelet counts (Table 5), perpetuation has been better demonstrated than initiation. If H pylori perpetuated ITP in as few as 10% to 20% of patients, then an appropriate strategy for management of ITP might involve testing for H pylori and eradicating it in those patients who were infected.
Since the relationship between H pylori and ITP remains controversial in adults11,12 and is far from being established in children,17 this study was performed to investigate the prevalence of H pylori infection in 74 North American patients with ITP aged 10 and older and to determine the effect of H pylori eradication. The determination of active H pylori infection was assessed by a breath test, a noninvasive, highly sensitive and specific method18 that has been used in almost all of the previous studies (Table 5 includes a literature review).
The prevalence of 21.6% of H pylori infection found in the 74 patients with ITP was surprisingly low compared with the prevalence of 32.5% assessed by presence of serum IgG antibodies in 7465 healthy adults in the United States.14 The difference in the method of H pylori detection and the ethnic distribution of our patient population are unlikely to explain this low rate of infection. Indeed, in a previous study, the prevalence of H pylori infection among 239 healthy white Americans was 34% using a urea breath test.19 While 25% of children 6 to 19 years old are infected in the United States,15 none of the 11 patients aged of 19 or younger included in the series reported here had a positive breath test. Even eliminating these adolescents, the prevalence of H pylori infection only reached 25.3% in the adults (16/63). These data do not support H pylori initiating ITP in our patient population.
Could H pylori infection be predicted? The questionnaire contained 2 variables that showed a trend toward identifying H pylori infection: heartburn or gas burping. As with the healthy controls, increased age was associated with a higher likelihood of H pylori infection. Therefore, if one wished to test ITP patients, one approach would be to test those older than 50 years of age and those younger than 50 years of age with heartburn or gas burping. In the series reported here, this would have identified 15 of the 16 infected patients while testing only 52 of the total of 74.
Can eradication of H pylori cure ITP? One limitation of previous studies was that at most 25% of the H pylori–positive patients who received the eradication regimen were those with chronic severe thrombocytopenia (ie, platelet count < 30 × 109/L and/or previous splenectomy4 ; Table 5). By comparison, among the 15 H pylori–positive patients treated in this study, all had chronic ITP with a platelet count less than 55 × 109/L (7 were < 30 × 109/L) and all have been previously treated for their ITP by 2 to 6 different treatments including splenectomy in 5 cases (33%). Therefore, these patients had a very low likelihood of spontaneous improvement and the effectiveness of H pylori eradication on ITP outcome was easier to assess. The eradication rate was 93% since alternative treatment was pursued when the initial regimen was ineffective. However, despite this good rate of eradication and unlike previous studies,2-8 only one of our H pylori–positive patients achieved a significant response 3 months after eradication and this response did not last.
In this study, 3 months was chosen as the time limit for seeing an effect of H pylori eradication. If no response was seen at that time, other therapies were initiated if necessary. Previous studies that provided time frames all demonstrated platelet recovery within 60 days after H pylori eradication.2,6,8 In this study, extending the time beyond 3 months following H pylori eradication did not seem to affect the response since the only platelet changes observed were in those patients who had initiated other therapies. To explain the high rates of response reported by others (Table 5), a nonspecific effect of the drugs used to eradicate the bacteria seems unlikely since in this present study none of the 10 H pylori–negative patients who received the Prevpac experienced a significant improvement in their platelet count.
The striking discrepancies between this report and those from Italy and Japan suggest several hypotheses. One hypothesis is that the response to H pylori infection could be influenced by the host's immunogenetic background.20,21 However, the contradictory findings reported in patients of similar European origin (ie, Spain, France, and Italy)2-4,11,12 (Table 5) do not support this hypothesis. Another possibility is that different strains of H pylori, namely those with different cag or vag (cytotoxicity/virulence-associated genes) proteins,20 could exert different immunologic effects on the host T and B cells and hence on ITP. A third hypothesis is that the expression of various Lewis (Le) antigens by H pylori isolates22 and the subsequent production of anti-Le antibodies could play a role in ITP pathogenesis since platelets may adsorb Lewis antigens from the serum.
The management of ITP in adults is complex and may require immunosuppressive therapies and/or splenectomy. One of the challenges for physicians caring for patients with ITP is to find less toxic and more effective approaches. The expectation at the beginning of this study was that a percentage of patients could be “cured” by administration of the Prevpac for 2 weeks. Unexpectedly, in this study there was not a greater prevalence of H pylori in ITP patients. Furthermore, and unlike most of the previous studies, none of the patients substantially improved their platelet count as a result of H pylori eradication. Therefore, even if the success of treatment of the H pylori–infected patients could be predicted by age and questionnaire, it is not obvious from this study that one would choose to test and eradicate infection in them. Future studies performed in this setting should be randomized and controlled and should include large numbers of patients requiring therapy. In addition to tracking the platelet count, other parameters that might be important determinants of response as suggested in the hypotheses considered above should also be studied.
Prepublished online as Blood First Edition Paper, August 14, 2003; DOI 10.1182/blood-2003-03-0900.
The publication costs of this article were defrayed in part by page charge payment. Therefore, and solely to indicate this fact, this article is hereby marked “advertisement” in accordance with 18 U.S.C. section 1734.