Introduction
Polycythemia vera is a clonal disorder arising in a multipotent hematopoietic progenitor cell that causes the accumulation of morphologically normal red cells, white cells, platelets, and their progenitors in the absence of a definable stimulus and to the exclusion of nonclonal hematopoiesis.1,2 First described in 1892,3 polycythemia vera is not a new disease and while uncommon, with an incidence of at least 2 per 100 000,4-6 it is not a rare disease. Yet, after 10 decades of careful clinical and laboratory investigation, the etiology of polycythemia vera remains unknown and there is no consensus as to the optimal therapy for the disorder.7 There is, however, no reason for this to be so. Although the molecular basis of polycythemia vera remains elusive, it is the central thesis of this review that the pathophysiology of polycythemia vera is sufficiently well defined for the provision of a rational treatment program that prolongs life, alleviates the specific morbidities associated with the disease, and avoids complications related to the consequences of the underlying molecular defect. However, for such an approach to be successful, it is first necessary to recognize the contradictions between what is actually known about this disease and how that knowledge has been interpreted and applied clinically, and that is the purpose of this review.
The pathogenesis of polycythemia vera: polycythemia vera is a myeloaccumulative disorder not a myeloproliferative disorder
Erythropoiesis and growth factor hypersensitivity
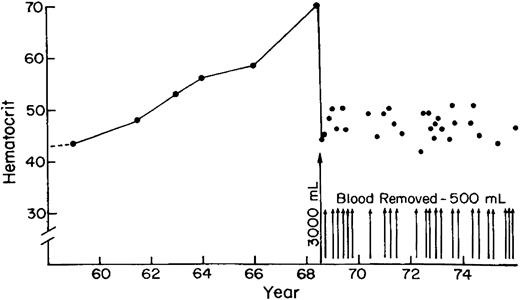
Because it involves a multipotent hematopoietic progenitor cell, the hallmark of polycythemia vera is trilineage hematopoietic cell hyperplasia. However, erythrocytosis is its most prominent clinical manifestation, the cause of its most serious complications, and the “sine qua non” for its diagnosis. Therefore, most investigations of the pathogenesis of polycythemia vera have focused on erythropoiesis but with paradoxical results. Red cell life span is not prolonged in polycythemia vera8 and the erythroid progenitor cell pool is not expanded at the expense of the myeloid progenitor cell pool.9 At the same time, neither hyperoxia10nor renal failure11 suppress erythropoiesis in polycythemia vera patients, phlebotomy does not stimulate it,12,13 and serum erythropoietin levels are lower than in any other disease14 (Figure1).
Relationship between serum erythropoietin and hemoglobin in patients with polycythemia vera (○), secondary erythrocytosis (●) or relative erythrocytosis (x).
Adapted from Handin et al369 with permission of the publisher, Lippincott, Williams, and Wilkins.
Relationship between serum erythropoietin and hemoglobin in patients with polycythemia vera (○), secondary erythrocytosis (●) or relative erythrocytosis (x).
Adapted from Handin et al369 with permission of the publisher, Lippincott, Williams, and Wilkins.
These paradoxical results are due to the ability of polycythemia vera erythroid progenitor cells to proliferate in vitro in the absence of erythropoietin.15 This unusual behavior, however, does not define the limits of the abnormal clone since not all polycythemia vera erythroid progenitor cells exhibit erythropoietin-independence in vitro.16,17 Importantly, primitive polycythemia vera erythroid progenitor cells exhibiting either erythropoietin-dependence or -independence could give rise to both erythropoietin-dependent and -independent progeny, a characteristic that appeared fixed given that it remained constant over time when these progenitor cells were cultured in vitro. It is also worth noting that the in vitro proliferation of polycythemia vera erythroid progenitor cells in the absence of erythropoietin was not robust.17 This may be a consequence of the tendency of these cells to differentiate faster in vitro than normal erythroid progenitor cells in the absence of erythropoietin.18 Thus, the dominance exerted by the polycythemia vera erythroid clone over polyclonal erythroid precursors2 could be due in part to its ability to complete its differentiation more efficiently in a low erythropoietin milieu.
This dominance may also involve transforming growth factors produced by polycythemia vera mononuclear cells19 and the hypersensitivity of polycythemia erythroid progenitor cells to interleukin 3 (IL-3), granulocyte macrophage–colony-stimulating factor (GM-CSF),20 stem cell factor (SCF),21 and insulinlike growth factor (IGF-1).22 Despite claims to the contrary,23,24 this hypersensitivity does not appear to be the consequence of an abnormality in the negative regulatory hematopoietic phosphatase, SHP-1.25,26Indeed, evidence has been obtained for increased activity of a membrane-associated protein tyrosine phosphatase in polycythemia vera erythroid progenitor cells27 and although overexpression of INK4a and ARF has also been documented in these cells28 and constitutive phosphorylation of STAT3 has been observed in the granulocytes in a minority of patients,29no consistent abnormality of signal transduction or cell cycle regulation has been identified to date in polycythemia vera nor have mutations been identified in p53 or Ras during the chronic phase of the illness.30 There is evidence for both gain31,32 and loss33 34 of suppressor genes in polycythemia vera but exactly which genes and how they might affect erythroid progenitor cell behavior remain unknown.
Erythropoietin receptor function
Given the ability of polycythemia vera erythroid progenitor cells to survive in vitro in the absence of erythropoietin as well as their hypersensitivity to erythropoietin in particular and hematopoietic growth factors in general, there has been substantial interest in growth factor receptor function in this disease. c-Kit expression, ligand affinity, and internalization were normal in polycythemia vera erythroid progenitor cells35 but the development of erythropoietin hypersensitivity or independence as a consequence of gain in function mutations in the ligand-binding and cytoplasmic domains of the erythropoietin receptor36 raised the possibility that this receptor was involved in the pathogenesis of the disease. However, erythropoietin receptor expression and ligand binding were not different in polycythemia vera erythroid progenitor cells compared with normal erythroid progenitor cells.37,38Furthermore, no erythropoietin receptor gene amplification, rearrangements, or functional mutations have been identified in polycythemia vera patients.39 This is not surprising because forced expression of the erythropoietin receptor in primitive hematopoietic stem cells did not induce autonomous proliferation, enhance progenitor cell renewal, or stimulate granulopoiesis,40 all of which are features of polycythemia vera. Furthermore, although expression of a constitutively-active erythropoietin receptor caused both erythrocytosis and thrombocytosis in vivo,41 it did not cause trilineage hematopoietic progenitor cell hyperplasia.
Alternatively spliced forms of the erythropoietin receptor have been identified, one of which has a truncated cytoplasmic domain and was expressed at high levels in immature erythroid progenitor cells in contrast to the full-length receptor, expression of which increased with progenitor cell maturation.42 The function of the truncated receptor splice variant has been a matter of controversy.43,44 It was incapable of transmitting a signal but interfered with the proliferative activity of the full-length erythropoietin receptor44 while promoting differentiation.45 The truncated erythropoietin receptor splice variant was either not expressed well or at all in various erythroleukemia cell lines42,46 and its expression was also decreased or absent in polycythemia vera mononuclear cells.46 Since polycythemia vera erythroid progenitor cells differentiate more quickly than their normal counterparts,18 the significance of these observations with respect to the pathophysiology of the disease remains to be established.
Programmed cell death
The diverse and often conflicting observations concerning the behavior of polycythemia vera erythroid progenitor cells can be reconciled by the recent recognition that polycythemia vera erythroid progenitors overexpressed the antiapoptotic protein Bcl-xl and were resistant to apoptosis in the absence of erythropoietin.47Under normal circumstances, early erythroid progenitor cells are largely dormant and require erythropoietin as a mitogen to initiate their entry into cell cycle,48 while late erythroid progenitor cells which are largely cycling require only erythropoietin as a survival factor to allow completion of terminal differentiation.49 Erythropoietin deprivation results in cell cycle arrest in G0/G1,50 and down-regulation of expression of the antiapoptotic proteins Bcl-2 and Bcl-xl followed by programmed cell death.51 By contrast, overexpression of Bcl-2 or Bcl-xl allowed erythroid progenitor cells to maintain their viability while undergoing terminal differentiation in the absence of erythropoietin.51
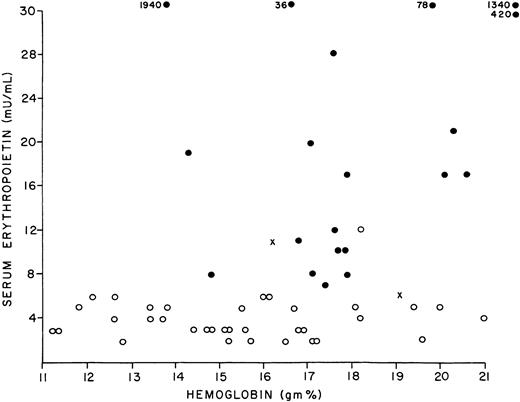
This behavior is not unique to erythroid progenitor cells, since multipotent hematopoietic progenitor cells overexpressing Bcl-2 not only remained viable in the absence of both growth factors and serum but were also able to undergo unrestricted lineage-specific commitment and terminal differentiation under these conditions as well.52 A significant feature of Bcl-2 overexpression was prolongation of the G1 phase of the cell cycle.52 Importantly in this regard, in vitro, the duration of G1 in erythroid progenitor cells appeared to be erythropoietin dependent; low concentrations of erythropoietin were associated with G1 prolongation and initiation of differentiation while high concentrations were associated with G1 shortening and cell proliferation.53 Thus, Bcl-xl overexpression could explain the accelerated differentiation of polycythemia vera erythroid progenitor cells in vitro in the absence of erythropoietin in contrast to their normal counterparts, as well as their survival advantage in vivo where erythropoietin production is suppressed, since both conditions promote G1 arrest and terminal differentiation. Therefore, the excess of erythroid cells that defines this disorder is more likely a consequence of cell accumulation than cell proliferation. This type of behavior is also consistent with and explains the incremental nature of the erythrocytosis in polycythemia vera (Figure 2) since only a fraction (5%-25%) of the erythroid progenitor cell population exhibited this behavior and its expression appeared to be random.17 Whether resistance to apoptosis in the absence of growth factors is a feature of myelopoiesis or thrombopoiesis in this disorder remains to be determined. One caveat with respect to this mechanism is that Bcl-xl expression is normally up-regulated with terminal erythroid differentiation54 and whether accelerated terminal erythroid differentiation in polycythemia vera was the cause of increased Bcl-xl expression or its consequence, and thus, whether another antiapoptotic mechanism might be involved, has not been established.
Rate of rise of the hematocrit level in a patient with polycythemia vera who sought treatment for the disease 9 years after the hematocrit level began to increase.
Adapted from Conley368 with permission of the publisher, The McGraw-Hill Companies.
Rate of rise of the hematocrit level in a patient with polycythemia vera who sought treatment for the disease 9 years after the hematocrit level began to increase.
Adapted from Conley368 with permission of the publisher, The McGraw-Hill Companies.
IGF-1
Insight into the mechanism for the resistance of polycythemia vera erythroid progenitor cells to apoptosis was provided by the observation that in the absence of serum, polycythemia vera erythroid progenitor cells were not more sensitive to erythropoietin than their normal counterparts. Rather, they were more sensitive to the antiapoptotic growth factor IGF-1.22 Furthermore, IGF-1 receptors on polycythemia vera peripheral blood mononuclear cells were constitutively tyrosine phosphorylated in contrast to those of normal blood mononuclear cells and also more sensitive to IGF-1.55 The serum concentration of IGF-1 binding protein-1 was increased in polycythemia vera patients and this protein was capable of stimulating erythroid burst formation in vitro.56 Importantly in this regard, it was recently demonstrated that cells expressing truncated erythropoietin receptors lacking their negative regulatory cytoplasmic domain and thought to be hypersensitive to erythropoietin36 were actually hyposensitive to the hormone in the absence of serum and hypersensitive to IGF-1.57 Thus, growth factor hypersensitivity in polycythemia vera could be a result of compensation for defective receptor-mediated signal transduction.
The thrombopoietin receptor, Mpl
Based on studies to date, the erythropoietin receptor cannot be implicated in such a process but the thrombopoietin receptor, Mpl, is a candidate. Mpl is expressed not only by megakaryocytes and platelets but also by pluripotent hematopoietic progenitor cells,58the survival of which is enhanced by the cognate ligand of Mpl, thrombopoietin.59 Thrombopoietin also acts synergistically with SCF and IL-3 to promote the proliferation of pluripotent hematopoietic stem cells,60 while impaired Mpl or thrombopoietin expression results in a reduction in the number of both multilineage and committed hematopoietic progenitor cells.61 Thrombopoietin in conjunction with SCF promotes the production of neutrophils from CD34+cells62 and in conjunction with erythropoietin, the production of erythroid progenitor cells,63 an effect that may be due to abrogation of apoptosis.64 Thrombopoietin overexpression in mice caused granulocytosis, thrombocytosis, osteomyelofibrosis with extramedullary hematopoiesis, and death,65 while ectopic expression of Mpl caused fatal erythroblastosis.66 Importantly, the retrovirus, MPLV, which encodes an Mpl gene truncated in its extracellular domain and fused with a viral envelope protein gene, induced a syndrome in mice that mimicked polycythemia vera,67 while hematopoietic progenitor cells infected with MPLV were growth factor–independent in vitro and capable of terminal differentiation in the absence of growth factors.68 Finally, Mpl expression and, therefore, its responsiveness to thrombopoietin in the megakaryocytes and platelets of polycythemia vera patients, were defective due to an as-yet-undefined impairment of its posttranslational glycosylation that became more profound with disease duration and extent.69These observations, taken together with the recent demonstration that removal of the Mpl distal extracellular cytokine receptor domain conferred growth factor–independent survival on hematopoietic cells expressing these truncated receptors,70 support the contentions that impaired hematopoietic growth factor receptor signaling has a fundamental role in the pathophysiology of polycythemia vera, that Mpl is a candidate receptor in this regard, and that polycythemia vera is a disorder of cell accumulation not cell proliferation.
The diagnosis of polycythemia vera: Osler's legacy; polycythemia vera is a clinical diagnosis
Diagnostic criteria
William Osler was not the first to describe a patient with polycythemia vera.3 He was, however, the first to emphasize that phenotypic mimicry could confound the diagnostic process and to propose clinical criteria to distinguish polycythemia vera from other disorders causing erythrocytosis71 (Table1). Remarkably, the Osler diagnostic criteria omit leukocytosis or thrombocytosis, an omission that may have diagnostic connotations as discussed below, but are otherwise similar to the major diagnostic criteria proposed by the Polycythemia Vera Study Group (PVSG) 6 decades later72 (Table 1). These diagnostic criteria are as important for what they do not specify as for what they do. First, bone marrow examination is not part of the diagnostic criteria. This is appropriate because bone marrow abnormalities, such as an increase in megakaryocytes and cellular hyperplasia with a loss of the fat spaces, while characteristic, can never alone be diagnostic for polycythemia vera,73 and if the other major PVSG diagnostic criteria are met, bone marrow examination is unnecessary. Furthermore, while nonrandom cytogenetic abnormalities and myelofibrosis have diagnostic implications, neither has prognostic implications74,75 and their frequency is too low to make bone marrow examination cost-effective. Even if bone marrow examination were diagnostic, that would still not abrogate the need for red cell mass and plasma volume determinations, tests that are justifiably cost-effective. Consequently, marrow examination is useful only when there is a change in the clinical course of the disease, for research purposes or for clinical trials. Yet, bone marrow aspiration and biopsy are frequently performed in the initial evaluation for polycythemia vera.7 This only confirms or generates an unexpressed fear of leukemia on the part of patients; a fear often validated by their physicians with respect to prognosis when in fact, with appropriate management, such an occurrence is only a remote possibility. Second, assays for erythropoietin and erythroid colony-forming cells are not part of the PVSG diagnostic criteria. While it can be argued that 30 years ago these tests were either insensitive or unavailable, it is equally easy to argue for the latter test that availability is still restricted clinically and that for both, specificity and sensitivity are unsatisfactory.
Serum erythropoietin
The development of a sensitive and specific assay for circulating erythropoietin for the purpose of distinguishing autonomous from secondary erythrocytosis was long a holy grail of hematologists. Although we now have such an assay, it is an irony that due to the unique physiology of erythropoietin, measurement of the hormone in the circulation cannot be relied on to distinguish between autonomous and erythropoietin-driven erythrocytosis. This is because as the red cell mass expands, both improved tissue oxygenation and the associated increase in blood viscosity serve to depress erythropoietin production,76 while the plasma residence of erythropoietin is simultaneously reduced through increased catabolism by the expanded erythroid progenitor cell pool.77 The net result is that while the lowest erythropoietin levels occur in polycythemia vera14 (Figure 1), this is not absolute and a “normal” erythropoietin level is common in hypoxic erythrocytosis unless the hypoxia is extreme.78 Indeed, given the wide range of normal for serum erythropoietin (4 mU/mL-26 mU/mL), unless the premorbid serum erythropoietin level is known, a 6-fold elevation could occur without exceeding the normal range. Thus, while an elevated serum erythropoietin level suggests tissue hypoxia as a cause for erythrocytosis, a normal serum erythropoietin level does not exclude an hypoxic cause. Only an arterial oxygen saturation determination, as stipulated by the PVSG criteria, will suffice for this purpose.
Erythroid progenitor cell assay
Similarly, although erythropoietin-independent erythroid colony formation in vitro is characteristic of polycythemia vera15 and has been widely embraced as a diagnostic test for the disease, it cannot be recommended for this purpose. The reasons are many and cogent. Erythropoietin-independent erythroid colony formation is not specific for polycythemia vera. Although it is most obvious in this disorder, it can be seen in nonclonal causes of erythrocytosis79,80 and in healthy controls79,81 as well as in essential thrombocytosis.81-84 Furthermore, endogenous erythroid colony formation has been absent in some patients who meet the PVSG criteria for polycythemia vera.85 Part of the problem may be methodologic since the greatest specificity and sensitivity has been observed when bone marrow was used as the source for erythroid progenitor cells as opposed to peripheral blood and when erythroid colony-forming units (CFU-Es) were analyzed as opposed to erythroid burst-forming units (BFU-Es).86 The in vitro clonal assay for erythroid progenitor cells is also neither standardized nor widely available. For these reasons and because this assay does not establish clonality, it cannot be recommended as a routine clinical diagnostic test for polycythemia vera.
PVSG minor criteria
In an effort to improve diagnostic accuracy, particularly in the absence of splenomegaly, the PVSG added additional criteria such as the presence of leukocytosis and thrombocytosis. Approximately 60% of patients will not have both of these abnormalities initially4,87,88 nor will leukocyte alkaline phosphatase expression, serum vitamin B12, and unbound serum vitamin B12 binding capacity be uniformly elevated.88 89
Impaired platelet Mpl expression
A number of other phenotypic abnormalities of the red cells (eg, microcytic erythrocytosis,90 increased hemoglobin F synthesis18), white cells (eg, increased surface expression of IgG receptors,91 impaired responsiveness to chemotactants92), and platelets (eg, reduced PGD2 receptor expression,93 impaired lipoxygenase generation94,95) have been observed in polycythemia vera but none of these abnormalities are either specific for the disease or suitable clinically for diagnostic use. Recently, impaired expression of the thrombopoietin receptor, Mpl, by the platelets of polycythemia vera and idiopathic myelofibrosis patients was documented96 and the severity of this defect correlated with the duration and extent of disease.69 A similar abnormality was not present in secondary erythrocytosis or chronic myelogenous leukemia (CML) but was present in some patients with essential thrombocytosis.97 Interestingly, recently the development of polycythemia vera or idiopathic myelofibrosis was observed in 3 of 4 essential thrombocytosis patients with reduced platelet Mpl expression,98 suggesting that the abnormality could have prognostic significance in this disorder. Whether impaired platelet Mpl expression will prove clinically useful for distinguishing polycythemia vera from other types of erythrocytosis or to identify polycythemia vera in the absence of erythrocytosis remains to be established. However, the consistency with which impaired platelet and megakaryocyte Mpl expression was observed in polycythemia vera patients96 99 suggests that it may be useful diagnostically.
PRV-1 expression
Recently, overexpression of the mRNA of a novel member of the uPAR receptor superfamily, designated PRV-1, was identified in polycythemia vera granulocytes by subtractive hybridization.89 This GPI-linked surface membrane receptor was detected only in normal granulocytes after exposure to granulocyte–colony-stimulating factor (G-CSF), was not expressed in the mononuclear cells from patients with secondary erythrocytosis, CML, or acute myelogenous leukemia (AML) and did not correlate with the expression of leukocyte alkaline phosphatase, another GPI-linked protein.89 Interestingly, like impaired Mpl expression, PRV-1 expression has also been detected in certain patients with essential thrombocytosis who also demonstrated in vitro erythropoietin-independent colony formation.100Quantitation of PRV-1 mRNA expression may also prove useful diagnostically in distinguishing polycythemia vera from other disorders causing erythrocytosis.
Clonality assays
The most important omission from the PVSG diagnostic criteria for polycythemia vera was a requirement for the establishment of clonality. Unfortunately, however, in contrast to CML, there has been no clinically applicable clonal assay for polycythemia vera or its companion myeloproliferative disorders, idiopathic myelofibrosis and essential thrombocytosis. Nonrandom chromosome abnormalities are not uncommon in these disorders and in polycythemia vera the most frequent are trisomies of 1q, 8, 9 or 9p, del13q, del20q, or interstitial deletions of 13 or 20; occasionally multiple defects are present.31,74,101,102 However, there is no consistent or unique cytogenetic abnormality associated with any of these disorders and at the time of diagnosis, using conventional cytogenetic techniques, less than 20% of polycythemia vera patients exhibit a cytogenetic abnormality and many patients never develop one.74 In this regard, the use of interphase fluorescence in situ hybridization (FISH) may increase the diagnostic yield.32 However, bone marrow aspiration is still required for cytogenetic analysis unless there are numerous primitive cells in the circulation.
In the absence of a specific and consistent cytogenetic marker, clonality assays in the chronic myeloproliferative disorders other than CML have been limited to genes on the X chromosome whose expression in women is subject to random inactivation. It was on this basis that the clonality of polycythemia vera was first established.1However, this type of clonal analysis is limited to women who are informative with respect to the expression of G-6PD isoenzymes or specific DNA polymorphisms. Expression of the former is restricted while the latter analysis is not informative in up to 30% of female patients103 and its utility is further limited by nonrandom, age-associated X-linked gene inactivation.104-106 Thus, although it has been clearly established as a general principle that polycythemia vera is a clonal disorder and represents the consequences of transformation of a multipotent hematopoietic progenitor cell, there is currently no way to establish clonality in the majority of patients considered to have the disease. While this is not an issue in patients exhibiting trilineage hematopoietic cell hyperplasia and extramedullary hematopoiesis, it is a critical issue in patients with erythrocytosis alone since in the absence of proof of clonality, it is difficult to justify the use of mutagenic drugs. Osler was well aware of the phenotypic mimicry that complicated the diagnosis of polycythemia vera71 and given the well-documented existence of unidentified and newly recognized nonclonal forms of erythrocytosis107 108 we would do well to follow his lead.
Measurement of the red cell mass and plasma volume
With respect to what the PVSG diagnostic criteria do stipulate, the most important is elevation of the red cell mass. Admittedly, this criterion does not establish clonality or even distinguish polycythemia vera from other disorders that cause erythrocytosis. However, it makes a vitally important point with respect to the evaluation of a high hematocrit level in general and polycythemia vera in particular—that only direct measurement of the red cell mass and plasma volume will suffice to distinguish absolute erythrocytosis from so-called spurious or relative erythrocytosis due to plasma volume contraction or red cell redistribution.109-111 Indeed, it is not hyperbole to state that failure to appreciate this basic concept has been responsible for more diagnostic and therapeutic failures in patients with polycythemia vera than any other single factor. The reason appears to be a lack of understanding of the pathophysiology of the red mass and plasma volume in disorders causing erythrocytosis.
Normally, the hematocrit or hemoglobin is maintained at a constant level that is characteristic for each individual but varies between individuals of the same sex by as much as 15% and between sexes by approximately 10%. As a corollary, erythropoietin production as represented by the serum erythropoietin level also remains constant.112 With tissue hypoxia, regardless of cause, as the red cell mass increases there is usually a concomitant reduction in plasma volume. Given the other factors involved in plasma volume regulation as well as in its measurement, the magnitude of plasma volume reduction reported with hypoxic erythrocytosis due to right-to-left cardiac shunts,113 impaired pulmonary gas exchange,114 carbon monoxide poisoning,115and low ambient oxygen tension116 varies but the downward trend is unmistakable. It should not be surprising, therefore, that therapy with recombinant erythropoietin,117 androgenic steroids,118 and even blood transfusion119also leads to a reduction in plasma volume; the mechanisms involved are unknown but may in part be protective since increasing whole blood viscosity suppresses endogenous erythropoietin production.76,120 By contrast, in polycythemia vera where erythropoiesis is autonomous and erythropoietin production is suppressed, as the red cell mass increases the plasma volume may be unchanged or increase121 until the hematocrit level is more than 60%.122
Unfortunately, the hematocrit level, whether directly determined by centrifugation or calculated from the mean corpuscular volume (MCV) and the red cell count, will not reflect these changes because even under normal circumstances, the distribution of red cells and plasma is not uniform throughout the circulatory system.123-125Rather, as demonstrated by independent determinations of the red cell mass and plasma volume, the ratio of red cells to plasma is higher in the peripheral vessels, venous or arterial, than it is in the body as a whole (ie, whole body hematocrit derived from independent measurements of red cell mass and plasma volume/peripheral venous hematocrit = 0.92).126,127 This is a consequence of both the slower flow of the peripherally displaced plasma compared with the axial red cells and plasma skimming in the smaller vessels.123,125,128,129 With disease, changes occur in the plasma volume and red cell mass or in their distribution, particularly if there is splenomegaly121,130-132 that will not be evident by hematocrit level determination alone.109,133-136 Indeed, the assumption that the hematocrit accurately reflects the red cell mass or, stated differently, that the red cell mass:plasma volume ratio is constant in health and disease or even for all parts of the circulation, is simply incorrect and nowhere more so than when erythrocytosis is present.114,127,134 136
Remarkably, although it was established in 1921123 and repeatedly confirmed125,126,137,138 that only by independently measuring the red cell mass (currently with51chromium) and the plasma volume (with125I-albumin) could an accurate assessment of each as well as the total blood volume be obtained, there is still resistance to this standard of practice. The reasons for this are several. First, the range of normal for such measurements, not unlike the range of the hematocrit, is wide, which affects their sensitivity. Consequently, only values more than 2 standard deviations (25%) above the mean are considered abnormal.139 Second, since adipose tissue has a low vascularity, red cell mass correlates better with lean body mass than body weight127 but, unfortunately, there is no simple method for clinically assessing lean body mass.111Therefore, if body weight in mL/kg is used as standard, the red cell mass will be underestimated in the obese,140 requiring correction factors based on weight.139 For these reasons and because of the need to use 2 radioisotopes, it has been variously advocated that the red cell mass be calculated from the plasma volume and the hematocrit141 by a mathematical formula based on the regression of the red cell mass on the hematocrit,142or dispensed with altogether on the grounds that the diagnosis of polycythemia vera is usually clinically apparent on the basis of other findings.143 None of these approaches are either physiologically sound or clinically acceptable because they rely on assumptions about the red cell mass:plasma volume ratio derived from measurements in healthy individuals that are not valid in disease.109,127 Simply stated, in disease, the red cell mass and plasma volume can vary independently of each other and it is no more possible to assess the red cell mass from the hematocrit than it is to determine total body sodium from the serum sodium concentration. Splenomegaly, of course, just compounds the problem.130-132 144 Stated differently, it is the author's opinion that whenever the diagnosis of polycythemia vera is considered, due to the potential of plasma volume expansion, a “normal” hematocrit value can never be considered normal and an independent determination of both the red cell mass and plasma volume by isotope dilution is mandatory for diagnostic and therapeutic purposes. Examples of the usefulness of red cell mass and plasma volume measurements in the evaluation of the cause of a high hematocrit level are shown in Table 2.
Anecdote as paradigm: the natural history of polycythemia vera has not yet been defined
The description of the natural history of polycythemia vera in current hematology textbooks disguises the fact that little more is known today about its clinical course than was known 80 years ago. Attempts to define the natural history of polycythemia vera then as now have been frustrated not only by the low incidence of the disorder but also its chronic nature which precludes most physicians from seeing more than a few of these patients or even following them for a sufficient duration to encounter the full scope of the disease. These factors coupled with an initial lack of appreciation of the effect of radiation or chemotherapy on bone marrow function led to the acceptance of anecdotal case studies as representative of the natural history of polycythemia vera.
The natural history hypothesis
In 1954, based on such anecdotal reports, a hypothetical description of the natural history of polycythemia vera was proposed by Wasserman according to which the disease evolved through a series of clinical stages beginning with an asymptomatic phase and proceeding through erythrocytotic, compensated or inactive, and spent or postpolycythemic myeloid metaplasia phases before terminating in acute leukemia if death from another cause did not intervene first.145 Given the similarity of this proposed natural history to that of CML, it is not surprising that without either testing or debate, the status of dogma was promptly conferred on this hypothetical description, and for the past 46 years it has been reiterated unchanged in greater or lesser detail in virtually every major hematology textbook when in fact the clinical data from which it was derived fail to meet the lowest standard of evidence-based medicine. Indeed, the basis for this concept of the natural history of polycythemia vera was a 1938 publication by Rosenthal and Bassen describing 13 patients from a series of 75 who were thought to be representative of the various hematologic manifestations of the disease.146 Of the 13 patients. 2 were anemic and thereby thought to manifest the so-called “spent” phase of the disorder, a concept first proposed by Minot and Buckman.147 Both, however, had previously been treated with radiation therapy.
Dameshek had earlier proposed a similar natural history scheme148 but qualified his proposal as follows: “it is difficult to state what the ‘normal’ course of the disease would be without the various therapeutic methods which undoubtedly influence it.” Unfortunately, this caveat was disregarded and only rarely have polycythemia vera patients been followed long enough without exposure to therapeutic interventions such as radiation or 32P that significantly alter bone marrow function for any meaningful appreciation of the natural history of the disorder to be obtained. When this has been achieved, a different picture of the disease emerges.149,150 Additionally, it is not widely appreciated that the disease may have different manifestations depending on the age at onset and the patient's sex.151 Finally, adding to the confusion has been the uncritical acceptance or misuse of terms such as “spent phase” and “postpolycythemic myeloid metaplasia” together with the assumption that the various chronic myeloproliferative disorders are interrelated152 when in fact proof is lacking that they are.153
The spent phase of polycythemia vera
While it has been clearly established that polycythemia vera can be complicated by anemia, myelofibrosis, and myeloid metaplasia, the frequency with which these complications occur and their clinical significance in the absence of cytotoxic therapy has rarely been ascertained prospectively. For example, the development of anemia due to bone marrow exhaustion has been considered an inevitable event in the natural history of polycythemia vera and possibly a forerunner of leukemia.145,154 As mentioned above, it was in this context that the term “spent phase” was initially used.147 However, in a large series of polycythemia vera patients managed without radiation therapy, anemia was most often due to chemotherapy, hemorrhage, deficiency of iron, folic acid or vitamin B12, or another disease and not to intrinsic marrow failure.149 Importantly, the role of iron deficiency as a cause for anemia was not recognized in early descriptions of the disease,147 nor was it appreciated that the plasma volume expansion associated with splenomegaly could mask the true red cell mass. Furthermore, in some patients, the “spent phase” proved to be reversible with therapy.150When these facts, together with ferrokinetic studies in patients with advanced disease155 are taken into account, it is clear that that there is not necessarily an irreversible exhaustion of erythropoiesis with disease progression or duration and that while the frequency with which refractory anemia is a direct consequence of polycythemia vera remains to be established, from the available data, it appears to be uncommon.156 157 More important than the so-called spent phase is the peculiar wasting syndrome that can develop late in the course of polycythemia vera in which intractable weight loss is associated with extramedullary hematopoiesis and substantial elevation of the white cell and platelet counts.
Finally, the term “spent phase” as used today also appears to mean different things to different authors. Initially and still employed to denote the progression of polycythemia vera to a state of bone marrow failure and possibly a prelude to leukemia145,146 it has also been used to describe a phase of polycythemia vera with splenomegaly without either myelofibrosis or myeloid metaplasia in which erythrocytosis continues unabated with its extent masked by plasma volume expansion.136 As indicated above, the former use of the term has never been authenticated in a scientifically acceptable fashion and the latter use, of course, is actually contradictory since in the type of patients described, bone marrow function was actually robust.155,158 Furthermore, such patients have also been described by others as being in the “stationary phase” of the disease,148 a designation that is equally improbable since no evidence has been provided that disease activity has changed. All of this only serves to illustrate the confusion that results when anecdotal experiences are uncritically elevated to the status of paradigm and medical jargon is substituted for medical judgment. In a disease such as polycythemia vera, anecdotal case reports are invaluable for defining what is possible but only prospective longitudinal studies of well-defined patient cohorts can establish what is probable.
Myeloid metaplasia
This conclusion also applies to 2 other complications of polycythemia vera, myeloid metaplasia and myelofibrosis. Since splenomegaly in polycythemia vera is initially due to red cell congestion,13,159-161 without a tissue biopsy, the assumption that splenic enlargement represents extramedullary hematopoiesis could be erroneous.133,162 It is probably for this reason that estimates of the frequency of myeloid metaplasia, based on the presence of immature myeloid and erythroid cells in the circulation or organomegaly, have varied from 7% to 14%.75,145,157,163 Furthermore, the widely used term “postpolycythemic myeloid metaplasia”164 is more than imprecise; it is an oxymoron since it implies that myeloid metaplasia is a terminal complication or conversion of polycythemia vera to another disorder rather than being an integral component of the disease itself165 that may not shorten survival.75,166,167 It also implies that bone marrow activity is impaired when in fact, in the absence of radiation or chemotherapy, there is no correlation between the extent of extramedullary hematopoiesis and bone marrow hematopoietic activity in polycythemia vera.168
As originally used, “postpolycythemic myeloid metaplasia” was a synonym for the spent phase of polycythemia vera in which the predominant features were myeloid metaplasia, splenomegaly, myelofibrosis, and anemia.164 However, as indicated above with respect to anemia, there have been few attempts to analyze the influence of radiation or chemotherapy on the development of “postpolycythemic myeloid metaplasia” but when this has been done, the majority of patients fitting this description have been exposed to agents toxic to the bone marrow.163,164,169 Thus, a century after the description of polycythemia vera, judgment must remain suspended as to the frequency with which bone marrow failure is a terminal feature of this disease in the absence of an exogenous cause but published data suggest that it is not high.157
Myelofibrosis
Given the above, it should not be surprising, therefore, that substantial misconceptions also exist with respect to significance of myelofibrosis in polycythemia vera. This is because the mechanisms for myelofibrosis are poorly understood170-172 and the means for quantitating it imprecise due to the patchy nature of the process.168,173-175 Furthermore, with respect to diagnosis, it has generally been assumed that polycythemia vera and idiopathic myelofibrosis are closely related disorders,152although apart from phenotypic similarities, this assumption has never been substantiated scientifically. Indeed, some investigators have considered the development of myeloid metaplasia and myelofibrosis in polycythemia vera as indicating the onset of a “transitional myeloproliferative disorder”135 rather than part of the natural history of the disease, while others have considered erythrocytosis to be a complication of idiopathic myelofibrosis.134 The development of myelofibrosis per se in the setting of polycythemia vera has also been considered to have adverse prognostic implications,176 another erroneous assumption.75,150,156,174 177
Because there is no widely accepted standard for the quantitation of marrow reticulin158 nor a universally acknowledged definition for the term “myelofibrosis” outside the setting of the disease, idiopathic myelofibrosis,178 it is difficult to obtain a precise frequency for its occurrence in polycythemia vera as well as the impact of therapy on this. Within the limitations of these data, it appears that increased marrow reticulin is part of the natural history of the disease, presumably reflecting in part the increase in marrow cellularity158,179 and possibly disease duration.180 However, an increase in marrow reticulin, or even osteosclerosis, is certainly not synonymous with a “spent” phase75,134,135,155,158,181-183 and can be modified to a certain extent by therapy,75 particularly with busulfan.182,184 Spontaneous regression of myelofibrosis has also been observed,168,175,182,185,186 although the patchy nature of the process makes this observation as difficult to substantiate as the contention that myelofibrosis is a progressive and destructive process.173-175 187
If studies of idiopathic myelofibrosis patients can be used as a guide, myelofibrosis and osteosclerosis are not usually progressive processes.168,174,188 There does, however, appear to be a higher incidence of “myelofibrosis” in polycythemia vera patients exposed to either radiation or chemotherapy than those treated by phlebotomy alone, 8.4%156,163,164,173,189 versus 4.5%,149,156,163 but there is not absolute agreement on this point.75,176 As a corollary, in studies of idiopathic myelofibrosis, polycythemia vera patients comprised 16% (range, 7%-38%) of the patients and most had been treated with radiation or chemotherapy.173,175,177,190-193 To the extent that it has been evaluated, marrow reticulin was increased in 8% to 15% of polycythemia vera patients at the time of diagnosis,73,181,194,195 a finding that appeared to have no prognostic significance.75,150,167 This is in contrast to development of myelofibrosis in CML, which is generally associated with disease acceleration.196 Taking everything together, while it is clear that the hematologic manifestations of polycythemia vera include myeloid metaplasia and myelofibrosis, it is not yet established that these processes indicate terminal bone marrow failure or that marrow failure is an inevitable consequence of the disease in the absence of cytotoxic therapy. Certainly, given the limitations of the data upon which the current concept of the natural history of polycythemia vera is based, it is time to abandon uncritical and unphysiologic terms such as “stationary,” “spent,” “transitional,” and “postpolycythemic myeloid metaplasia” in favor of descriptions based on quantitative, prospective, and biologically sound observations.
Acute leukemia: relationship to therapy
The relationship between polycythemia vera and acute leukemia also requires clarification because it is central to the management of polycythemia vera. In 1950, Schwartz and Ehrlich reviewed the published evidence that acute leukemia was a feature of polycythemia vera in the absence of exposure to mutagenic therapy.197 Of 83 published cases, only 30 had unequivocal evidence of polycythemia vera preceding the development of acute leukemia and 25 of these patients had been irradiated. Of the remaining 5 patients, data supporting the absence of radiation exposure were available for only one. Since the criteria employed by Schwartz and Ehrlich for the diagnosis of polycythemia vera and the diagnosis of acute leukemia were stringent, it is ironic that in the one case of polycythemia vera that they accepted as spontaneously developing acute leukemia, the diagnosis was not histologically confirmed.146 They also emphasized the association of the newly introduced 32P therapy with acute leukemia in polycythemia vera patients and correctly predicted that this complication would increase in frequency. By contrast, the advocates of 32P therapy thought that the development of acute leukemia was an inevitable consequence of extended patient survival.133 198
Modan and Lilienfeld's landmark 1965 paper unequivocally demonstrated that the leukemogenic effect of irradiation or 32P was not a consequence of prolonged survival,163 but the impact of their observations was blunted by the report of Halnan and Russell in which the incidence of acute leukemia in 32P-treated polycythemia vera patients was negligible.199 Any doubt about this issue, however, was eliminated by the PVSG-01 trial which established that therapy with either 32P or the alkylating agent, chlorambucil, resulted in an incidence of acute leukemia far exceeding that observed with phlebotomy alone without prolonging survival.200 The apparent conflict between the Modan and Lilienfeld data and that of Halnan and Russell was in part due to study design, since the mean time of onset of 32P-induced acute leukemia is approximately 8.5 years201 while most of Halnan and Russell's patients were followed for only 5 years, and in part to differences in radiation dose. Parenthetically, this episode serves to remind us that the absence of evidence is not proof of its absence.
Polycythemia vera has the dubious distinction of being the first hematologic malignancy and only the third disorder temporally—ankylosing spondylitis202 and thymic enlargement203 being the other 2—in which an association between acute leukemia and therapeutic irradiation was identified.197 Unfortunately, acceptance of the leukemogenicity of irradiation in polycythemia vera was delayed by the belief that leukemia was an inevitable feature of the disease.145,154,204 As a consequence, practitioners in this area were denied an essential paradigm to guide their therapy until similar observations had been well established for other hematologic205 and nonhematologic neoplasms.206 Importantly, from a biologic perspective, the leukemogenic effect of irradiation or alkylating agents in polycythemia vera was neither qualitatively nor quantitatively different from that observed for other neoplasms treated in the same fashion with respect to drug or radiation exposure, latency, type of leukemia, cytogenetic abnormalities, and response to treatment.180,207,208 Although data have been presented suggesting that myeloid metaplasia and myelofibrosis predispose to acute leukemia in polycythemia vera,145,193,209 this contention remains controversial since the number of patients involved was small and the observations were not confirmed in other studies.163,167,180 Furthermore, therapy-induced acute leukemia has also been observed in patients with secondary erythrocytosis mistakenly treated with chemotherapy or radiation.163,210 211 These considerations are not trivial since they speak to the larger underlying issue of the spontaneous development of acute leukemia in polycythemia vera.
Spontaneous acute leukemia: Richter syndrome revisited
In contrast to the well-established body of data on treatment-induced acute leukemia in polycythemia vera,163,180,197,200,207,212-214 few data exist other than anecdotal case reports with respect to the spontaneous occurrence of acute leukemia. As mentioned above, up to 1950, Schwartz and Ehrlich accepted as valid only one published report describing such an event.197 In the same year, Dameshek reported that one of his 50 patients and 2 of 100 Mayo Clinic patients treated only by phlebotomy had developed acute leukemia.148 Since then there have been 12 individually published case reports215-217 and an additional 11 patients identified by questionnaire215 in whom acute leukemia complicated polycythemia vera in the absence of irradiation or chemotherapy, while in 4 published series comprising 505 patients, 3 cases of spontaneous acute leukemia were observed.149,156,163,218Demographically, these patients are of interest because 90% were men with a mean age of 60.5 years, in contrast to those developing acute leukemia following alkylating agent therapy, of whom 54% were men with a mean age of 52.5 years. The interval for the former group between the onset of polycythemia vera and acute leukemia was 4.8 years (range, 1-13 years) and in the chemotherapy-treated group 6.7 years (range, 1-20 years), but these latter data are not comparable because the time of initiation of alkylating agent therapy relative to the onset of the polycythemia vera was not defined. It is also of interest that 3 of the 10 patients in the spontaneous leukemia group for whom the information was available had undergone splenectomy 2 to 8 years before the onset of the leukemia.193,219 Finally, in contrast to the chemotherapy-treated patients, patients developing spontaneous acute leukemia could still have concomitant erythrocytosis and only partial bone marrow transformation at the time that the leukemia was recognized.220
Second cancers occur more often than can be explained by chance in patients already afflicted by a malignancy221 but with the exception of exposure to radiation, radiomimetic drugs, or a combination of these, the mechanisms involved are undefined. With respect to the development of secondary acute leukemia, age, disease stage, type of cancer,221 and immunologic status including the postsplenectomy state222-225 have all been considered to have a role. In some instances, the development of myelodysplasia or acute leukemia could even be considered a paraneoplastic syndrome226,227 since there is precedent for the cytokine-driven development of acute leukemia.228 With respect to polycythemia vera, given the increasing incidence of acute leukemia with age,5 the mean age of polycythemia vera patients, and the restoration of the polycythemic state with successful remission induction therapy,220,229,230 the possibility of a chance occurrence cannot be excluded particularly with the simultaneous presence of both disorders.229 At the same time, given the evidence of clonal evolution or succession in polycythemia vera,74 the possibility of leukemia arising from the malignant clone is also likely. The role of splenectomy is intriguing since this has been implicated in the evolution of acute leukemia in idiopathic myelofibrosis223 although the observation remains controversial.231
Importantly, the polycythemia vera patients with spontaneous acute leukemia described to date differ from those with treatment-induced acute leukemia not only by their male predominance but also by their age at onset and the short interval between the diagnosis of polycythemia vera and the development of acute leukemia, thereby excluding prolonged survival, myeloid metaplasia, or myelofibrosis as antecedent factors as claimed.209,218 In fact, the situation is similar in many respects to Richter syndrome, in which chronic lymphocytic leukemia is complicated by either the development of a diffuse large cell lymphoma or transformation to prolymphocytic leukemia.232 These uncommon events can occur in untreated patients without regard to disease duration and may arise from either the original malignant clone or one immunologically distinct.233 However, regardless of mechanism, the important point is that the spontaneous development of acute leukemia in polycythemia vera is uncommon and certainly not inevitable, and our patients deserve to know this.
Survival with polycythemia vera: hematology's second amendment privilege
Probably no myth has been more pernicious with respect to the well being of polycythemia vera patients than the myth of survival which exists in 2 versions. It is difficult to understand how this myth attained credibility since there were both anecdotal reports185,234,235 and observational series146,147,149,236 that firmly established the prolonged survival of polycythemia vera patients in an era when the mainstays of therapy were phlebotomy, phenylhydrazine, and sporadic irradiation. Unfortunately, these observations were ignored in favor of the first version of the myth which arose from the assumption that leukemia was an inevitable feature of polycythemia vera.198 This position was stated most emphatically by Osgood,237 “…for any treatment the benefits to be obtained must be weighed against the risks incurred. Most patients would rather die at an advanced age with some risk of leukemia than at an earlier age from some other cause.” However, no patients appear to have been polled about this contention but it would be more realistic to conclude that most would rather die at an advanced age with no risk of leukemia.
The second version derived from an early attempt to study survival in polycythemia vera in a systematic fashion. In 1962, Chievitz and Thiede reviewed the causes of death in 250 Danish polycythemia vera patients. Among their conclusions were the following: “Out of the untreated patients, 50% had died 18 months after the onset of the first symptom or sign, and out of patients treated with venesection half had died 3 1/2 years after this juncture. Out of patients treated by X-rays half were alive 12 1/2 years after the first sign.”156 This article was one of the first to report survival data and has been the rationale for the implementation of various treatments for polycythemia vera without provision for the inclusion of the appropriate phlebotomy control group.238And this was true even though 12 years previously, another Danish physician, Videbaek, reporting on a series of 125 patients, noted a 50% survival of 4.5 years for men and 8.5 years for women treated with phlebotomy or irradiation but not 32P.239Indeed, Videbaek came to the conclusion that “…a large proportion of the high mortality which is known to attend polycythemia vera is not due to inadequacy of the therapeutic measures, but rather to the fact that the patients are not followed up as they should be,” a point ignored not only by Chievitz and Thiede but also by many in the hematology community.201 240-242
The differences between the experience of Videbaek and that of Chievitz and Thiede can be explained in part by the fact that more than twice as many of the patients in the latter series were older than 65 years and age of onset appears to influence survival.215 At the same time, Videbaek's patients undoubtedly had less access to medical care, which was also likely to have been of a lower standard, making the differences in survival even more striking. Furthermore, as stated previously, the literature contains sufficient other support for the contention that the clinical course of polycythemia vera, without treatment or treatment mainly by phlebotomy, was not as dismal as described above.149,150 Therefore, it is difficult to explain the universally uncritical acceptance of Chievitz and Thiede's conclusions except on the grounds that they either suited the prejudice of those who were enamored of particular therapies such as32P204,237 or provided hematologists with the same type of “constitutional privilege” with respect to the treatment of polycythemia vera200,201,243,244 that is invoked by those American citizens who support the right to bear arms without restriction. Indeed, even today, there are advocates of32P therapy,201,245 although it has been widely appreciated for 50 years that this agent was least effective against the most troublesome feature of polycythemia vera, extramedullary hematopoiesis.167,189 246
Central to the myth of survival is the assumption that polycythemia vera is a monolithic disease when in fact it is not122,146,246,247 and while no one would advocate withholding treatment once the diagnosis was established, it is important to emphasize that the disease can develop gradually and be substantially advanced before it becomes clinically problematic (Figure2). Presumably, this is a consequence not only of the slow rate of hematopoietic cell accumulation but also the concomitant compensatory expansion of the plasma volume. The occurrence of a preclinical or asymptomatic phase was first documented by Rosenthal and Bassen,146 confirmed by Dameshek,148 and calculated to be between 17 and 80 months by Swolin et al based on the rate of accrual of cytogenetic abnormalities.74 The Gruppo Italiano Studio Policitemia documented a significant incidence of thrombosis more than 2 years before the diagnosis of polycythemia vera,244 as did the PVSG,248 and in another study, 11 of 13 patients with an intraabdominal venous thrombosis had an elevated hematocrit level for 6 or more months before onset of thrombosis,249 also supporting a significant latent period even in symptomatic patients. Finally, Rozman et al250 and others251 have presented data suggesting that the life expectancy of polycythemia vera patients in the modern era was not greatly different from normal. Since both retrospective163and prospective controlled clinical trials have established that radiation or chemotherapy did not prolong life more than phlebotomy,200 and that the course of polycythemia vera is generally indolent, its management should be in keeping with its tempo and not with what we should acknowledge to be historical inaccuracies.
Phlebotomy and polycythemia vera: women are not small men
Thrombosis and hemorrhage in polycythemia vera
Erythrocytosis not only distinguishes polycythemia vera from its companion myeloproliferative disorders but is also responsible for its most frequent and serious complications. Published data indicate that thrombosis was the presenting feature in 12% to 49% of patients,133,149,156,194,239,244,252,253 occurred in up to 40% during the course of the illness,194 and was the cause of death in 20% to 40%.145,149,156,239,244,254Furthermore, in 2 studies, 14% to 15% of patients had a history of a thrombotic event at least 2 years before diagnosis.244,248In general, the central nervous system was the most frequent site of thrombosis,156,244,253,255 arterial thrombosis was more common than venous156,244,253-255 and the latter was characteristically cerebral or intraabdominal and more frequent in women,151,194,241 possibly in keeping with their higher incidence of splenomegaly at presentation.239 Indeed, polycythemia vera was the most common cause of hepatic vein thrombosis in the Western hemisphere.256 Finally, although not as frequent as thrombosis, hemorrhage in polycythemia vera was generally considered to be a consequence of vascular stasis and thrombocytosis133,149,257 and like thrombotic events, primarily involved the central nervous system and the gastrointestinal tract, was a presenting manifestation in 6% to 58% of patients149,156,194,239 and fatal in up to 30.149,156,239 254
Whole blood viscosity
The mechanisms involved in the hypercoagulable state that characterizes polycythemia vera are currently still under scrutiny258 even though they were apparent to the first clinicians to study the disease. The hematocrit is the principal determinant of blood viscosity259-261 and nowhere is this more evident than in polycythemia vera. Perhaps the most cogent observation in this regard was made by Weber in 1908, “In every case examined after death the distention of the visceral vessels has been very striking, the mesenteric vessels presenting sometimes the appearance of having been forcibly injected for purposes of anatomical demonstration.”262 Brown and Giffin added to that description in 1923 with their study of nail-fold capillaries, which were elongated and engorged to capacity due to the formation of red cell aggregates, leading to diminution of blood flow that was most marked in the venous limb.263 Since cardiac output was either normal or increased in polycythemia vera patients due to an increased stroke volume,264,265 the diminution in capillary flow appeared to represent the influence of both peripheral vasodilatation and increased blood viscosity. In this regard, it needs to be emphasized that major vessel venous thrombosis in polycythemia vera most likely represents the end stage of a process beginning in very small vessels.266 These observations are also compatible with the preponderance of thrombotic events in the brain and the abdomen. In the former, an increase in hematocrit was associated with a decrease in blood flow,267-269 while the latter appears to be particularly vulnerable to disorders conducive to stasis or endothelial damage such as sickle cell anemia or paroxysmal nocturnal hemoglobinuria.
Although it has been argued that the decrease in cerebral blood flow associated with a high hematocrit level is a physiologic response to increased oxygenation not increased viscosity,270 the data upon which this contention are based either actually support the latter process270,271 or fail to substantiate the former since the subjects studied were actually not sufficiently hyperviscous.272,273 On the contrary, there are physiologically sound data indicating that cerebral blood flow like blood flow elsewhere274 declines independently of oxygen transport when blood viscosity increases.275
Blood viscosity is an exponential function of the hematocrit259 and red cell aggregation increases at high hematocrit levels,276 creating the potential for vascular stasis if red cell production is left checked. While no other mechanism for thrombosis need be invoked in this circumstance, other mechanisms could contribute. Thus, increasing the hematocrit at flow rates found in the arterial circulation enhanced platelet-vessel wall interactions277 and this mechanism could be involved in the high incidence of arterial thromboses without requiring an elevation in platelet count.255 Additionally, a high hematocrit level has also been found to interfere with the vasodilatory effects of nitrous oxide278 which could account for the hypertension associated with polycythemia vera133,149,239,279 as well as its thrombotic tendency. Leukocytes can impede red cell migration in capillaries,280 interact with platelets at the vessel wall,281 and appear to be activated in polycythemia vera,282,283 but their role in the thrombotic process remains undefined because polycythemia vera patients treated with chemotherapy did not have a greatly diminished risk of thrombotic events.200 Finally, although impairment of the fibrinolytic system284 and platelet activation285 have been observed in polycythemia vera patients, such defects were not limited to this myeloproliferative disorder. For example, spontaneous platelet aggregation was most marked in patients with idiopathic myelofibrosis286 who were more prone to hemorrhage than thrombosis.287 Finally, there is no evidence that other coagulation defects predisposing to hypercoagulability are more prevalent in polycythemia vera patients than in the general population, although they are certainly not immune to them.288 289
Phlebotomy therapy: pros and cons
Not only is there compelling evidence that increased blood viscosity due to an elevated red cell mass is the principal basis for the hypercoagulable state in polycythemia vera, there is equally strong evidence that phlebotomy, a venerable practice that was well known in the Hippocratic era, is the most effective remedy. Unfortunately, it is both an irony and a tragedy that this is one Hippocratic principle that many hematologists have been reluctant to embrace wholeheartedly. The reasons are many but none are clinically tenable or physiologically sound. First, although phlebotomy was recognized by early clinicians as an effective method of bringing symptomatic relief to polycythemia vera patients, the adequate or consistent application of phlebotomy was deterred by the concern that it would stimulate new blood formation. Thus, in 1928, an authoritative review of the disease stated “One must conclude that while venesection is an important and useful in relief in emergency in the treatment of these patients, it cannot be looked upon in any other light than as a further, and therefore undesirable stimulant to new blood formation.”159 This contention, reaffirmed more than once in modern times in the absence of any data,87,145,148,290 is, of course, erroneous, since bone marrow function in polycythemia vera, as in the other myeloproliferative disorders, is autonomous and erythropoiesis can neither be suppressed by hyperoxia10,291 nor substantially stimulated by hypoxia292 or phlebotomy,12,13,293 and this appears to be true for thrombopoiesis as well in the absence of anemia.150,182 293-295
Second, it has been contended that phlebotomy provokes hypercoagulability. As stated by Osgood, “The major risks from phlebotomy are that it sets in motion all the clotting mechanisms plus suddenly reducing blood volume and possibly slowing the blood current and results in increased risk of thromboses and iron deficiency.”238 All aspects of this contention are indefensible. First, to the extent that any form of erythrocytosis provokes a hemorrhagic diathesis, phlebotomy restores coagulant activity toward normal by reducing blood viscosity296,297and thereby improving blood flow, platelet function,298,299 and the balance between coagulation factor concentration and red cell number, and this is as true in polycythemia vera133,300 as in the erythrocytosis of cyanotic congenital heart disease.301 Second, in contrast to 32P therapy, venesection actually expands the plasma volume and thus results in a greater reduction in blood viscosity for any reduction in red cell mass than the former297 (Table3). Paradoxically, this effect of venesection is also observed in pseudoerythrocytosis in which the plasma volume is reduced,302 an effect not always recognized.110 Moreover, in addition to a direct reduction in total blood volume, plasma volume expansion is another relatively immediate effect,303 making phlebotomy at once both corrective and protective. Finally, the effectiveness of venesection in relieving symptoms due to an elevated red cell mass has been repeatedly documented in patients with secondary forms of erythrocytosis.304-307
Iron deficiency and whole blood viscosity
Concerns over the adverse effects of phlebotomy-induced iron deficiency relate to both its side effects and the potential for increased blood viscosity.308,309 The former concern was addressed by exercise studies of chronically iron-deficient polycythemia vera patients in whom no impairment of aerobic capacity was detected,310 nor were functional signs of iron deficiency observed other than the gustatory perversion pica.311 Iron deficiency–related hyperviscosity is a test tube artifact308,309 that also has no physiologic basis.312,313 Although iron-deficient red cell membranes may be less deformable than normal,314 this abnormality is apparently offset by their reduced size and internal viscosity since their hemoglobin content is also reduced.315 Thus, at comparable hematocrit levels, iron-deficient blood was not more viscous than normal.312,313 Furthermore, red cell–platelet interactions are influenced by red cell diameter and such interactions are reduced with small red cells.315 Finally, a state of chronic iron deficiency that limits erythropoiesis is actually the ultimate goal of phlebotomy therapy in polycythemia vera, a goal that is unfortunately frequently not achieved judging from published results.156,200,239 244
Phlebotomy and myelofibrosis
A more serious claim has been that the use of phlebotomy therapy alone in polycythemia vera results in a high incidence of myelofibrosis,316 a claim that is difficult to understand except as population specific since it is contrary to most published experience. For example, in a series of 207 patients followed for more than 10 years, only 4 patients treated solely by phlebotomy developed myelofibrosis,149 while in another series of 250 patients, none of the patients treated solely by phlebotomy developed myelofibrosis.156 Indeed, this experience has been the rule148,156,163 rather than the exception. As a corollary, the low incidence of polycythemia vera patients recorded in a published series of myelofibrosis patients173,175,190,192 as well as the high incidence of myelofibrosis observed in patients treated with hydroxyurea169 suggest that this complication is neither frequent nor limited to patients exposed only to phlebotomy. Furthermore, since myelofibrosis can be a presenting manifestation of polycythemia vera73,317 and also occurs in patients exposed to 32P163,189,318 and x-ray therapy,156,163,234 there are no grounds to implicate venesection as a specific causal factor. An additional difficulty in this regard, as discussed above, is the definition of myelofibrosis; a dry tap or increased reticulin is not sufficient for this purpose.158,179 Finally, implicit in this contention is the notion that myelofibrosis is deleterious in polycythemia vera, when in fact it is perfectly compatible with normal bone marrow function,134,155,181,183 is a reversible process,168,175,184-186 and has not been shown to impact adversely on survival.150,174 177 Indeed, failure to recognize polycythemia vera presenting as myelofibrosis is potentially more deleterious than the development of myelofibrosis during the course of the disease.
Phlebotomy and thrombosis
The most serious and damaging criticism of phlebotomy therapy in polycythemia vera is that it was associated with an excess of thrombotic events compared with other treatments.200Unfortunately, the data upon which this criticism is based were the consequence of a complete misunderstanding of the pathophysiology of erythrocytosis in polycythemia vera. In contrast to other forms of erythrocytosis in which expansion of the red cell mass is typically accompanied by a reduction in plasma volume, expansion of the plasma volume is common in polycythemia vera.110,132 That this was not initially appreciated was presumably due to the practice of measuring only the red cell mass.319 Plasma volume expansion is associated with a concomitant reduction in peripheral vascular resistance and an increased cardiac stroke volume for its accommodation. As a consequence, although peripheral vascular resistance eventually increases, it does so more slowly than when erythrocytosis occurs in a normovolemic setting and systemic oxygen transport is actually increased at any given hematocrit level.320 However, because of the plasma volume expansion, the hematocrit is no longer an accurate indicator of the red cell mass in polycythemia vera patients and this is particularly true when splenomegaly is present.130-132 Therefore, it is not surprising that PVSG data indicated that approximately 15% of patients with a hematocrit level of 50% and up to 40% with hematocrit levels of up to 55% had an elevated red cell mass88; similar observations have been made by others.321 More importantly, not only is cerebral blood flow impaired in polycythemia vera patients when the hematocrit level is more than 45%,267 but the incidence of thrombotic events shows a linear increase above the same hematocrit level.322 Thus, hematocrit values that are apparently within the normal range cannot be considered as safe in polycythemia vera patients and it is this syndrome of masked or inapparent erythrocytosis132 due to plasma volume expansion that is not only responsible for what has been termed a latent,323 “prethrombotic,”244or “forme fruste”324 myeloproliferative disorder but also the increased incidence of thrombotic events in such patients. Since even under normal circumstances, the hematocrit level in most organs with the exception of the spleen is much lower than the venous hematocrit level,124 it is clear that the situation in polycythemia vera is actually more serious than it appears and that the so-called “prethrombotic state” of polycythemia vera merely reflects inadequate reduction of the red cell mass.
The physiology of red cell mass expansion in polycythemia vera appeared to have been disregarded in the defining PVSG protocol-01, in which the phlebotomy treatment threshold was initially set at 50%,72 even though as indicated above, a minimum of 15% of male patients would be undertreated at this hematocrit level, as would 100% of women, since no woman normally has a hematocrit level of 50%. Unfortunately, even when the hematocrit threshold for phlebotomy was subsequently lowered to 45%,248 women patients were still at risk of undertreatment. Thus, the therapeutic conundrum of the PVSG, that treatment by phlebotomy alone resulted in a higher incidence of thrombosis during the first 3 years of therapy while chemotherapy or radiotherapy resulted in a high incidence of malignancy thereafter,243 was not a conundrum at all but rather the consequence of inadequate reduction of the red cell mass to begin with. Furthermore, since in polycythemia vera red cell production is tightly linked to the iron supply,325 differences in phlebotomy requirements were not a function of a difference in disease activity243 but rather in the extent of iron stores or availability. Unfortunately, based on a recent survey, an inappropriately high threshold for phlebotomy therapy is still being employed by many American hematologists.7
Thrombocytosis and polycythemia vera: platelets at your finger tips
Fact versus fiction
Perhaps no other medical condition has caused more otherwise astute clinicians to abandon disbelief than thrombocytosis, particularly with respect to its contribution to the coagulopathy of polycythemia vera. The high frequency of vascular occlusion associated with this disease had been recognized for many years159but not until 1938, in the absence of any proof, was it suggested that thrombocytosis was a cause of major vessel thrombosis,146a suggestion subsequently accepted by influential clinicians145,154,290 without corroborating evidence. There is a particular irony in this since when essential thrombocytosis was first recognized, not only was it called hemorrhagic thrombocythemia326 but many of the patients described actually had unrecognized polycythemia vera.327,328 More importantly, no study to date, either prospective or retrospective, has demonstrated a correlation between platelet number or function and major vessel thrombosis. For example, in the PVSG prospective trial involving 431 patients, there was no correlation between an elevated platelet count and the risk of thrombosis,243 while a follow-up study employing antiplatelet agents failed to demonstrate a reduction in thrombotic events.329 This should not have been surprising considering the number of retrospective studies that failed to identify a correlation between the platelet count and risk of thrombosis,87,150,255,330,331 the well-established correlation of thrombosis with an elevated hematocrit level,322,331 and the failure of the PVSG to ensure adequate reduction of the red cell mass in their patients.72,200 Furthermore, even though a large number of platelet function abnormalities have been identified in polycythemia vera, they did not correlate with the development of thrombosis332 nor did age in some series.333Additionally, even when patients with isolated thrombocytosis were considered, it was difficult to incriminate the platelet count as a thrombotic risk factor. For example, most patients with familial thrombocytosis did not have an increased incidence of thrombosis334-338 nor did those with reactive thrombocytosis339 and in the only prospective, controlled study of essential thrombocytosis to date, the incidence of thrombosis in untreated patients was not greater than in the control population.340
Part of the problem with defining the role of thrombocytosis as a thrombotic risk factor has been the intuition that it must be. This has led to reportorial bias with the publication and uncritical acceptance of anecdotal and incompletely studied case reports of unexpected thrombotic events occurring in association with thrombocytosis.242,341-343 These, unfortunately, not only fail to establish a cause and effect relationship but also merely provide a numerator without any denominator. As an example, when the factors associated with hepatic vein thrombosis were evaluated retrospectively, it was found that this event was actually preceded by a high hematocrit level and followed by thrombocytosis.249A second issue has been failure to consider other causes for hypercoagulability within the population under study such as the antiphospholipid syndrome344 or cardiovascular risk factors.345,346 In this regard, it is worth noting that the frequency of coronary artery thrombosis in the PVSG-01 trial243 was more in keeping with the latter than the frequency found by others for polycythemia vera patients in the absence of atherosclerotic disease.253 Indeed, when one considers the vaso-occlusive havoc initiated by heparin-induced thrombocytopenia or thrombotic thrombocytopenic purpura, it becomes immediately obvious that platelet number alone is not a critical determinant of hypercoagulability.
Hemorrhage and microvascular thrombosis
However, there is definitely a role for platelets in the coagulopathy that complicates polycythemia vera. With respect to bleeding, it has been established that platelet counts of more than 1 000 000/μL were associated with a hemorrhagic diathesis regardless of the cause.347,348 This was thought to be due to a reduction in high-molecular-weight von Willebrand multimers owing to their adsorption to platelets349 and was reversible with a reduction in platelet number350 or treatment with DDAVP.351 Equally important, and paradoxically, considering its effect on von Willebrand multimers, thrombocytosis can cause microvascular arteriolar thrombosis. This is manifest most often in peripheral vessels by the syndrome of erythromelalgia,352,353 and in the nervous system by a constellation of symptoms such as headache or ocular disturbances, often migrainous in type, amaurosis fugax, vertigo, diplopia, vertigo, hemiparesis, paresthesias, numbness, dysarthria, aphasia, and syncope.354 Usually transient and rarely progressive, these symptoms are distressing to patients and alarming to their physicians. Not infrequently, they may occur as the presenting manifestation of polycythemia vera and if superimposed on an already compromised vascular system could lead to a stroke, myocardial infarction, or peripheral gangrene.352,355 While the mechanism for platelet-associated microvascular occlusion is unknown, it is associated with increased platelet thromboxane B formation356 and increased platelet turnover.357,358 Both can be reversed or prevented by aspirin-induced platelet inactivation or a reduction in platelet count, though not necessarily to normal, suggesting that both platelet activation and platelet number are important. However, as demonstrated clinically,329 unless the red cell mass is appropriately reduced, antiplatelet therapy or chemotherapy will be futile, and this stipulation should be mandatory for any prospective study of the effect of antiplatelet therapy on large vessel thrombosis in polycythemia vera.
The management of polycythemia vera: first, do no harm
From the foregoing it is clear that the diagnosis and management of polycythemia vera continue to present formidable problems: polycythemia vera is a clonal disorder for which there is as yet no clinically validated clonal marker; trilineage hyperplasia is the hallmark of polycythemia vera but clinically the disease can mimic not only its companion myeloproliferative disorders, idiopathic myelofibrosis, and essential thrombocytosis, but also nonclonal causes of erythrocytosis; the disease is uncommon but its presenting manifestations are protean, ranging from intractable pruritus to the Budd-Chiari syndrome. Moreover, due to plasma volume expansion, splenomegaly, or hemorrhage, erythrocytosis, the one feature that sets polycythemia vera apart from the other chronic myeloproliferative disorders, may not be clinically obvious.132 Furthermore, contrary to conventional wisdom, the natural history of polycythemia vera has not been completely defined and neither staging criteria nor the factors affecting prognosis have been established even though it is well documented that the clinical course of the disorder is variable and that age and sex have an important influence in this regard.
While the currently accepted diagnostic criteria for polycythemia vera are useful for protocol studies, they do not define the limits of the disease, and a recent poll suggests considerable ambivalence among hematologists as to the optimal approach to the diagnosis of the disease as well as to its treatment.7 Remarkably, although erythrocytosis is the one feature that distinguishes polycythemia vera from its companion myeloproliferative disorders and the most frequent cause of serious complications, the utility of red cell mass and plasma volume determinations for diagnosis has been questioned as has the effectiveness of phlebotomy therapy. Unfortunately, the only prospective, controlled clinical trial of the disorder to date with respect to phlebotomy therapy, that of the PVSG, was flawed because the target hematocrit level chosen for phlebotomy therapy was too high.200 Thus, the therapeutic dilemma that patients treated initially with phlebotomy had an unacceptably high incidence of early thromboses while those treated with chemotherapy or32P later had a high incidence of leukemia, lymphoma, or cancer,243 is probably more apparent than real, at least with respect to the phlebotomy group. In the same fashion, given the lack of attention to reducing blood viscosity in this disorder, it can be seriously questioned whether a prior history of thrombosis and advanced age are truly risk factors for thrombosis in polycythemia vera patients.331 Certainly, neither chemotherapy nor radiotherapy has proved superior to phlebotomy in preventing thrombosis but both have proved to be more toxic.244 Furthermore, since polycythemia vera appears to be a myeloaccumulative disorder rather than a myeloproliferative one, at least with respect to the erythrocytosis and a disorder that is often indolent and of long duration, its treatment should be commensurate with that behavior.
The first issue with respect to management is diagnosis and it should be obvious that it is not possible to accurately estimate the red cell mass from the hematocrit level when polycythemia vera is a diagnostic consideration and the hematocrit level is less than 60% in a man or 50% in a woman. Measurement of the red cell mass and plasma volume by isotope dilution should be a standard of care but unfortunately this standard is more often honored in the breach than in the observance. In some locales, bogus medical economics have been allowed to dictate the availability of these procedures, which can only be seen as an abdication of our professional responsibilities as hematologists. While elevation of the red cell mass does not establish the diagnosis of polycythemia vera, the diagnosis cannot be made in its absence. Even if a clonal assay for polycythemia vera were available, such an assay would not abrogate the need for red cell mass and plasma volume determinations in this disease any more than the HFE assay for hemochromatosis has abrogated the need for serum transferrin saturation measurements as a guide to both diagnosis and therapy.
Reduction of the red cell mass and maintaining it at a safe level by phlebotomy (hematocrit level of < 45% in men and < 42% in women and < 36% during pregnancy) is the first principle of therapy in polycythemia vera. Venesection is a safe and immediately effective therapy and its desired side effect, iron deficiency, is not a liability,310 claims that cannot be made for any of the surrogate therapies for polycythemia vera that have been proposed to date. Reduction of the red cell mass and maintaining it at a physiologic level removes a major source of complications and may also alleviate systemic hypertension and pruritus359 and reduce splenomegaly.161,360 For many patients, no other therapy may be necessary for many years. Aspirin or anticoagulants such as coumadin are not substitutes for adequate phlebotomy; low doses of aspirin block urate excretion while titration of the coumadin dose can be difficult if the red cell mass is not controlled. Occasionally, with blood loss or overzealous phlebotomy, symptomatic anemia can ensue. Judicious iron replacement can accelerate the recovery process but too much iron will result in an explosive increase in red cell mass. The other complications of polycythemia vera (Table4), with the exception of leukemic transformation, represent the consequences of cell accumulation manifested as organ enlargement, microvascular occlusive or hemorrhagic phenomenon, hyperuricemia, or cytokine-mediated events such as pruritus and acid-peptic disease, but their treatment need not necessarily be genotoxic. For example, aspirin alone353,361 or anagrelide362 may be sufficient to combat the microvascular occlusive syndrome associated with thrombocytosis. It is, of course, important to remember that polycythemia vera patients are not immune to other illnesses causing thrombosis. Similarly, a modest leukocytosis requires no correction; however, if progressive, leukocytosis is a harbinger of extramedullary hematopoiesis or disease acceleration. In which case, the leukocytosis can serve as a guide to disease control following the institution of therapy.
Because there is currently no clonal marker for polycythemia vera, it is currently impossible to determine if a particular therapy is curative or merely palliative. In this regard, the long natural history of the disorder and the infrequent and unpredictable occurence of spontaneous leukemic transformation make it difficult to establish the superiority of any therapy or to recommend a potentially curative therapy such as allogeneic bone marrow transplantation that carries an immediate obligate mortality as well as the potential for substantial chronic morbidity. We are, however, fortunate to have a variety of symptomatic remedies for the many complications of polycythemia vera because no single remedy has proved completely effective for any of them. However, many of these remedies are not without risk and have their own unique toxicities. For example, pruritus can prove to be so intractable to phlebotomy, antihistamines, or psoralen-activated light therapy that resort must be made to suppression of hematopoiesis with alpha interferon, hydroxyurea, or even busulphan. Splenomegaly due to extramedullary hematopoiesis can be similarly difficult to manage. Yet attempts to avoid the complications of cell accumulation by chemotherapy or irradiation have not been without substantial toxicity,163,200,244 and while alpha interferon is a promising agent in this regard,363 it can have substantial side effects, particularly in the elderly364; it is also unknown whether this agent can alter the natural history of polycythemia vera. Tolerance to alpha interferon may be aided by starting with a low dose (500 000 U, 3 times per week) and escalating slowly; the addition of an antidepressant has also been found helpful.365 Although alpha interferon is expensive and its side effects can be debilitating, it has not been demonstrated to cause permanent marrow damage. The same may not be true for hydroxyurea,212,214 366 although the evidence is not entirely conclusive at this time. However, this was also the situation initially for other cytotoxic agents that subsequently proved to be leukemogenic in this disease. Therefore, it seems prudent to employ hydroxyurea only when other remedies have failed and to avoid long-term exposure whenever possible.
Since few physicians see many of these patients, the concerns described above emphasize the need to gain greater insight into the natural history of polycythemia vera and to reinitiate prospective, controlled multicenter clinical trials using the wisdom gained from such initiatives as the Cooperative Study of Sickle Cell Disease367 and the PVSG. Until such a time as those goals are realized, we can do no better than to heed the advice of William Dameshek, a proponent of phlebotomy therapy in polycythemia vera:“There seems to be a tendency in medical practice—by no means limited to hematologists—to treat almost every condition as vigorously as possible. In hematology, this consists in attempting to change an abnormal number—whether this number is hemoglobin, hematocrit, WBC, platelet count to normal values whether the patient needs it or not!”238
Prepublished online as Blood First Edition Paper, August 8, 2002; DOI 10.1182/blood-2001-12-0349.
References
Author notes
Jerry L. Spivak, Traylor 924, Johns Hopkins University School of Medicine, 720 Rutland Ave, Baltimore, MD 21205; e-mail: jlspivak@jhmi.edu.