Abstract
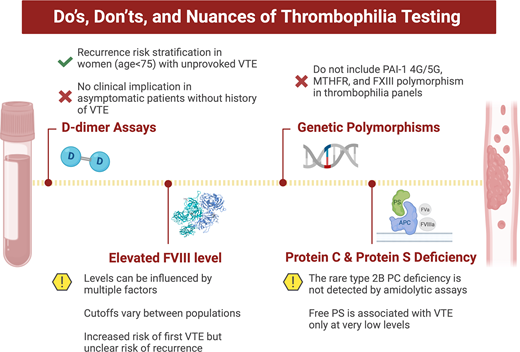
Considerable progress has been made in elucidating genetic and biologic risk factors for venous thromboembolism (VTE). Despite being able to identify heritable defects in a substantial proportion of patients with VTE, testing has not, in general, proven useful in management. Despite efforts to reduce inappropriate testing, it often falls to the hematologist to consult on patients having undergone thrombophilia testing. Through a series of cases, we discuss how D-dimer testing can be helpful in VTE recurrence risk stratification in younger women as well as how to approach patients with persistently elevated D-dimer levels in the absence of thrombosis. While elevated factor VIII coagulant activity levels are a significant risk factor for a first episode of VTE, its biologic basis is not fully understood, and studies have not shown it to be a useful predictor of recurrence. Abnormal results of genetic tests for methylene tetrahydrofolate reductase or plasminogen activator 1 promoter polymorphisms may be encountered, which carry little if any thrombotic risk and should never be ordered. We also discuss protein S deficiency, the most difficult of the hereditary thrombophilias to diagnose due to a wider “normal” range in the general population as compared with protein C, the presence of both free and bound forms in plasma, and the characteristics of the various assays in use. We also present a rare type of protein C deficiency that can be missed by functional assays using an amidolytic rather than a clotting end point.
Learning Objectives
Identify patients with venous thromboembolism in whom D-dimer can be useful for VTE risk stratification
Understand why an elevated FVIII:C level and testing for polymorphisms in PAI-1 and MTHFR lack clinical utility in the evaluation of VTE
Know the criteria for diagnosing clinically relevant protein S deficiency and a rare subtype of protein C deficiency
Introduction
Thrombosis is a multicausal disease that is associated with acquired and inherited risk factors. Abnormalities have been identified in 5 genes that increase the risk of venous thromboembolism (VTE), but there is limited clinical utility in testing for the defects. Testing is also done for FVIII coagulant activity (FVIII:C) as well as variants in other genes for which the thrombotic risk is uncertain. The utility of measuring D-dimer has been evaluated for predicting recurrence risk in unprovoked VTE. Through a series of cases, we discuss the utility or lack thereof of measuring D-dimer and FVIII:C and testing for polymorphisms in the plasminogen activator 1 (SERPINE1) and methylene tetrahydrofolate reductase (MTHFR) genes. Issues in diagnosing deficiencies of protein C and protein S are also addressed.
Role of D-dimer testing for VTE risk stratification
CLINICAL CASE
A 22-year-old woman presented with chest pain and shortness of breath and was diagnosed with bilateral pulmonary emboli (PE) by computed tomography (CT) pulmonary angiography. She was started on apixaban and her symptoms resolved over several weeks. An etonogestrel implant, a progestin contraceptive that had been in place for 3 years, was removed per recommendation in the Food and Drug Administration (FDA) label. She then developed iron deficiency anemia due to menorrhagia. There was no family history of VTE; screening tests for thrombophilia were normal (Table 1). She completed 6 months of rivaroxaban and was referred regarding the need for long-term anticoagulation.
Screening laboratory testing for hereditary thrombophilia in patients with venous thromboembolism
| Hereditary thrombophilia |
| Factor V Leiden mutation (using PCR-based assay) |
| Prothrombin G20210 mutation (using PCR-based assay) |
| Protein C deficiency (functional amidolytic assay) |
| Free protein S antigen |
| Antithrombin deficiency (heparin cofactor assay, save for patients on oral factor Xa inhibitors in whom antithrombin antigen is recommended to prevent “false normal” levels) |
| Hereditary thrombophilia |
| Factor V Leiden mutation (using PCR-based assay) |
| Prothrombin G20210 mutation (using PCR-based assay) |
| Protein C deficiency (functional amidolytic assay) |
| Free protein S antigen |
| Antithrombin deficiency (heparin cofactor assay, save for patients on oral factor Xa inhibitors in whom antithrombin antigen is recommended to prevent “false normal” levels) |
PCR, polymerase chain reaction.
This case illustrates a common question as to whether to extend anticoagulation beyond 3 to 6 months. The first consideration is whether etonogestrel constitutes a transient risk factor for VTE. Despite the information on the Food and Drug Administration label, studies have not shown an increased risk in users of progestin-only contraceptives. A population-based study showed that the use of oral low-dose progesterone, levonorgestrel intrauterine devices, and levonorgestrel implants was not associated with an increased risk of VTE.1
This patient therefore had unprovoked VTE, for which the risk of recurrent VTE after discontinuation of anticoagulation is 10% in the first year, 25% at 5 years, and 36% at 10 years.2 Men have a higher rate of recurrent VTE compared with women.2 While long-term anticoagulation is now recommended for many such patients, individualized decision-making is appropriate, taking into account its benefits and risks as well as patient preference.
D-dimer testing could be a useful risk stratification tool in this young woman (Table 2). Based on the PROLONG study, patients with a first unprovoked VTE who completed 3 months of anticoagulation had a VTE recurrence rate of 4.4% per year if a D-dimer test was negative 1 month after stopping warfarin.3 Women younger than 65 with non-hormone related VTE had a lower recurrence risk of 1.1%.4 In the subsequent DULCIS study, patients with persistently negative D-dimer tests at 15, 30, 60, and 90 days after discontinuation of anticoagulation had a VTE recurrence rate of 3% per year.5 The D-dimer Optimal Duration Study reported that women with a negative D-dimer while on anticoagulation and 1 month after discontinuation had a recurrence rate in the first year of 5.4%; the rate was 9.7% per year in men.6 The cumulative risk of recurrence at 5 years was 29.7% in men and 17.0% per year in women with non-estrogen-related VTE.7 A negative D-dimer result 1 month after discontinuing anticoagulation in this woman therefore translates to a recurrence rate of approximately 1.1% to 5.4% per year. With respect to bleeding, a meta-analysis of 14 randomized trials of indefinite anticoagulation for preventing recurrent VTE found annualized rates of major bleeding of 1.12% for direct oral anticoagulants and 1.74% for warfarin.8 The predictive value of D-dimer is diminished in men and older women (ages >65-70) who have high recurrence rates despite low D-dimer levels (ie, 7.5% per year in men, 6.6% per year in older women).4,7 Of note, the D-dimer “cutoff” (negative vs positive) varies among assays that have reported the risk of recurrent VTE; this should be considered in interpreting results.9
D-dimer testing for recurrent VTE risk stratification
| . | Population . | N . | D-dimer assay . | Cutoff values . | VTE recurrence rate after stopping anticoagulation (per year) . | |
|---|---|---|---|---|---|---|
| Negative D-dimer . | Positive D-dimer . | |||||
| PROLONG3,4 | First unprovoked VTE | 608 | Clearview Simplify (whole blood; qualitative) | Positive | Overall: 4.4% (1st year) 0.4% (women, age <65) 6.7% (women, age >65) 5.1% (men, age <65) 8.2% (men, age >65) | Overall: 10.9% 5.4% (women, age <65) 8.9% (women, age >65) 12.9% (men, age <65) 11.8% (men, age >65) |
| DULCIS5 | First unprovoked VTE or VTE with minor risk factors | 1010 | 5 quantitative assays | Predefined age- and sex-specific values | Overall: 3.0% (median 1.93 years) 2.1% (age ≤70) 8.9% (age >70) 4.7% (men) 4.8% (women) | Overall: 8.8% 14.3% (age ≤70) 12.5% (age >70) 10.0% (men) 20.5% (women) |
| DODS6 | First unprovoked VTE | 410 | Clearview Simplify® (whole blood; qualitative) | Positive | Overall: 6.6% (1st year) 9.7% (men) 5.4% (women, non-estrogen) 0% (women, estrogen) | —- |
| DODS extended follow-up7 | First unprovoked VTE | 293 | Clearview Simplify® (whole blood; qualitative) | Positive | Overall: 5.1% (median 5 years) 7.5% (men) 3.8% (women, non-estrogen) 0.4% (women, estrogen) | —- |
| . | Population . | N . | D-dimer assay . | Cutoff values . | VTE recurrence rate after stopping anticoagulation (per year) . | |
|---|---|---|---|---|---|---|
| Negative D-dimer . | Positive D-dimer . | |||||
| PROLONG3,4 | First unprovoked VTE | 608 | Clearview Simplify (whole blood; qualitative) | Positive | Overall: 4.4% (1st year) 0.4% (women, age <65) 6.7% (women, age >65) 5.1% (men, age <65) 8.2% (men, age >65) | Overall: 10.9% 5.4% (women, age <65) 8.9% (women, age >65) 12.9% (men, age <65) 11.8% (men, age >65) |
| DULCIS5 | First unprovoked VTE or VTE with minor risk factors | 1010 | 5 quantitative assays | Predefined age- and sex-specific values | Overall: 3.0% (median 1.93 years) 2.1% (age ≤70) 8.9% (age >70) 4.7% (men) 4.8% (women) | Overall: 8.8% 14.3% (age ≤70) 12.5% (age >70) 10.0% (men) 20.5% (women) |
| DODS6 | First unprovoked VTE | 410 | Clearview Simplify® (whole blood; qualitative) | Positive | Overall: 6.6% (1st year) 9.7% (men) 5.4% (women, non-estrogen) 0% (women, estrogen) | —- |
| DODS extended follow-up7 | First unprovoked VTE | 293 | Clearview Simplify® (whole blood; qualitative) | Positive | Overall: 5.1% (median 5 years) 7.5% (men) 3.8% (women, non-estrogen) 0.4% (women, estrogen) | —- |
VTE, venous thromboembolism.
CLINICAL CASE (continued)
D-dimer levels on rivaroxaban and 1 month after discontinuation were 228 ng/mL and 235 ng/mL (reference range, 0-500 ng/mL FEU), respectively. Following discussion of the benefits and risks of long-term anticoagulation, she preferred to discontinue rivaroxaban. She was advised of the need for prompt medical attention for symptoms or signs of VTE and appropriate thromboprophylaxis in high-risk situations.
Persistently elevated D-dimer levels in the absence of thrombosis
CLINICAL CASE
A 28-year-old woman was referred for a persistently elevated D-dimer. A level of 604 ng/mL was noted on presentation to the emergency department with chest pain; evaluation including CT pulmonary angiography and ultrasound of both lower extremities was negative for VTE. Despite being in good general health, follow-up testing showed persistently elevated D-dimer levels (>2,000 ng/mL).
D-dimer is a product of fibrin formation and degradation. In cases of suspected VTE, clinical assessment using validated tools (ie, Wells criteria) along with a negative D-dimer assay can exclude a diagnosis of VTE. When D-dimer is elevated and imaging is negative for VTE, it is unclear whether further evaluation should be done. Aside from VTE, elevated D-dimer levels are observed in a variety of physiologic and pathologic conditions, such as increased age, hormonal use, pregnancy, infections including COVID-19, cancer, inflammatory diseases, atrial fibrillation, acute aortic dissection, and disseminated intravascular coagulation.10,11 Clinical evaluation, including a detailed medical history, physical examination, routine laboratory tests (ie, complete blood count, basic metabolic profile, liver function tests), and age-appropriate cancer screening, are reasonable to identify such conditions.
D-dimer levels vary among healthy individuals, and a small percentage have very high levels.11 Studies of healthy populations have shown that elevated D-dimer levels are associated with an increased risk of VTE and overall mortality.12,13 These effects, however, are small and should not prompt extensive laboratory testing (eg, testing for thrombophilia) and imaging to exclude occult disorders that are not suspected clinically. It should be noted that interference with D-dimer assays can lead to spurious elevations (eg, presence of heterophilic antibodies).8
CLINICAL CASE (continued)
Evaluation did not reveal any causes of a persistently elevated D-dimer level, and no further diagnostic testing was deemed necessary. The patient was reassured.
Testing for elevated FVIII:C
CLINICAL CASE
A 53-year-old woman was diagnosed with PE 4 weeks after sustaining a left fibula fracture while on an estrogen-containing oral contraceptive. She remained active following the fracture. Her mother had a history of recurrent VTE following surgeries after age 60. She was initiated on apixaban and the oral contraceptive was discontinued. She was seen by her primary care physician 2 weeks later, at which time she was asymptomatic. Laboratory testing for hereditary thrombophilia and APS was negative; FVIII:C was elevated at 234% (reference range, 57%-163%).
This hematology consultation resulted from an elevated FVIII:C found as part of a thrombophilia evaluation. Despite the Choosing Wisely campaign's recommendation against testing for thrombophilia in patients with VTE in the presence of transient risk factors, such testing and referrals are frequent.14,15
An elevated FVIII:C, defined as the top decile of the population, has been identified in 25% of patients with a first unprovoked venous thrombotic event.16,17 Several factors affect FVIII:C, including von Willebrand factor level and ABO blood group. Individuals with non-O blood groups have von Willebrand factor and FVIII:C levels that are approximately 25% higher than type O.18 Genetics also plays a role in an individual's FVIII:C, and studies have identified familial clustering of high levels.19-21 However, the genetic basis and inheritance patterns have not been determined. Acute thrombosis can result in transient elevations in FVIII:C for up to 3 to 6 months. In some cases of venous thrombosis, the concomitant presence of an underlying inflammatory disorder is present in association with elevated C-reactive protein (CRP) and fibrinogen levels along with FVIII:C.17,22 Other factors such as body mass index, age, glucose, and triglyceride levels have been associated with elevations.19
In the Leiden Thrombophilia Study, patients with FVIII:C >150 IU/dL had an increased risk of venous thrombosis compared with those with FVIII:C <100 IU/dL (OR 4.8, 95% CI 2.3-10.0).16 Levels were obtained at a median interval of 18 months following the diagnosis of deep venous thrombosis (DVT) and at least 3 months after anticoagulation was discontinued. The risk of VTE increased with higher FVIII:C in a dose-dependent fashion. This finding was confirmed by several subsequent studies.17,23,24 However, it is unclear whether an elevated FVIII:C has an impact on the risk of recurrent VTE. In a recent systematic review, 9 of 16 studies failed to identify FVIII:C as an independent risk factor for recurrence.25 Thus, it is not our practice to obtain FVIII:C in patients who undergo testing for thrombophilia.
When FVIII:C is obtained as part of thrombophilia testing, there are additional challenges with respect to its interpretation. FVIII:C is generally measured using a one-stage clot-based assay; elevated FVIII:C measured by chromogenic assay and ELISA have also been associated with thrombosis.26,27 There is potential for interference in one-stage FVIII:C assays by heparins and lupus anticoagulants.28 Elevated FVIII:C is often defined as above the 90th percentile of the population.25 However, there is uncertainty regarding what cutoff values should be considered “elevated,” since cutoffs were >150% in the Leiden Study and >234% in the Vienna study.16,29 Standardization of such values with the applicable population is needed.16,29
CLINICAL CASE (continued)
Based on the provoked nature of the PE, this patient was continued on apixaban for 3 months. In this case, FVIII:C was found to be elevated 2 weeks after she was diagnosed with PE. Even if persistently elevated, its role in predicting recurrent VTE is uncertain. Thus the elevated FVIII:C should not affect the duration of anticoagulation.
Don’ts: testing for 4G/5G variants in the promoter of the gene encoding PAI-1 (SERPINE1) and other polymorphisms
CLINICAL CASE
A 42-year-old woman sustained ischemic strokes at ages 17 and 41. CT and magnetic resonance imaging showed old infarcts, but there was no evidence of vascular disease. Echocardiography (both transthoracic and transesophageal) did not show a patent foramen ovale, and cardiac telemetry was negative. She had no cardiovascular risk factors but developed PE following delivery at age 28 that was treated with 6 months of warfarin. There was no family history of thrombosis, and she did not have hereditary thrombophilia or markers of APS. Analysis of the PAI-1 gene showed heterozygosity for 4G/5G in the promoter. Her current therapy includes aspirin and a statin. Hematology is consulted regarding the significance of the 4G/5G variant and the role of anticoagulation for preventing recurrent stroke.
This case highlights one of several tests that are ordered by some practitioners to evaluate patients with arterial and/or venous thrombosis as well as women with recurrent adverse fetal outcomes: these include SERPINE1 4G/5G, MTHFR polymorphisms, homocysteine levels, and a common F13A gene polymorphism resulting in Factor XIII Val34Leu. However, the association of these laboratory abnormalities with an increased or decreased risk of thrombosis is minimal or relatively small.
The 4G/5G polymorphism in the SERPINE1 is associated with an increased plasma level of PAI-1.30 As compared with the 5G allele, carriers of the 4G allele had marginally increased risks of VTE and myocardial infarction (odds ratio, ∼1.2).31-33 However, there is no evidence of an increased risk of stroke.31,34 Some studies have shown a reduced risk in individuals carrying the 4G/4G genotype.35 The MTHFR polymorphisms, C677T and A1298C, are common, with heterozygosity and homozygosity in 40% to 60% and 16% of the population, respectively.36,37 These polymorphisms decrease function of the MTHFR enzyme, leading to elevated homocysteine levels; this effect is only relevant in folate-depleted states, which are rare in countries where folate-fortified food is mandated.38 Randomized trials have shown that lowering homocysteine levels with vitamin B6, B12, and folic acid supplementation does not prevent arterial thrombosis, VTE, or mortality.39-43 MTHFR polymorphisms are not associated with an increased risk of VTE or arterial thrombosis; testing for them or measuring homocysteine levels should not be done to evaluate for thrombophilia.37,44
CLINICAL CASE (continued)
The patient's history of PE was provoked as it occurred in the postpartum period; there is no evidence that anticoagulation will prevent recurrent stroke in this patient as a consequence of carrying the SERPINE1 4G allele. The situation would be no different if she had 1 of the 5 hereditary thrombophilias (Table 1).
Nuances: Testing for protein C deficiency and protein S deficiency
CLINICAL CASE
A 31-year-old woman is referred with a history of 2 first-trimester miscarriages but no history of thrombosis. Her mother had multiple venous thrombotic events following an initial DVT during pregnancy; her maternal grandmother and great-grandmother also had VTE during pregnancy. The patient's protein C activity and antigen levels were 55% (reference range, 70%-180%) and 111%, respectively. At her consultation with you regarding potential risks during a future pregnancy, protein C activity was 97%.
This patient had discrepant protein C activity levels measured by different laboratories. There are several potential explanations besides laboratory error or preanalytic factors. Protein C activity levels can be measured using either amidolytic (chromogenic) or clot-based assays (Table 3). Generally, amidolytic tests are preferred due to lower variability.45,46 Clot-based assays for protein C are subject to interference by lupus anticoagulants or anticoagulants. The levels of protein C can also be affected by several conditions (Tables 3 and 4).47 Another possibility is that the patient may have a rare type 2B variant of protein C deficiency with abnormalities in calcium, phospholipid, or cofactor binding.48 This type of protein C deficiency is only detected using the clot-based activity assay.
Diagnostic considerations in protein C deficiency and protein S deficiency
| . | Protein C deficiency . | Protein S deficiency . |
|---|---|---|
| Genetic mutation | PROC gene | PROS1 gene |
| Types of deficiency | Type 1 quantitative defect, low PC antigen and activity Type 2 qualitative defect, normal PC antigen but low activity • Type 2A • Type 2B—not detected by amidolytic assays | Type 1 quantitative defect; low total and free PS antigen, low activity Type 2 qualitative defect; normal total and free PS, low activity Type 3 selective quantitative defect; normal total PS, low free PS antigen, low activity |
| Activity assays | PC activity: • Clotting end point • Amidolytic end point (uses a chromogenic substrate) | PS activity: • Clotting end point |
| Antigen assays | PC antigen: immunoassays • Helps distinguish deficiency type, not required for diagnosis | PS antigen: immunoassays Free PS antigen—ELISA, latex immunoassays; initial test for diagnosis Total PS antigen—helps distinguish deficiency type, not required for diagnosis |
| Diagnostic threshold | PC activity <65%-70% | Free PS antigen <33% (in general population) <40%-50% (with patients with prior VTE or strong family history) |
| Laboratory interference | Clot-based assays: lupus anticoagulants, heparins, direct thrombin inhibitor, oral factor Xa inhibitors, elevated FVIII:C, FVL mutation, and hyperlipidemia | Clot-based assays: lupus anticoagulants, heparins, direct thrombin inhibitor, oral factor Xa inhibitors, elevated FVIII, FVL mutation, and PC deficiency |
| Conditions with acquired deficiency | Liver disease, DIC, vitamin K antagonist, vitamin K deficiency, recent surgery or trauma, acute inflammatory illnesses, oral contraceptive pills, or acquired antibodies | Liver disease, DIC, vitamin K antagonist, vitamin K deficiency, nephrotic syndrome, L-asparaginase therapy, oral contraceptive pills, pregnancy, or acquired antibodies |
| . | Protein C deficiency . | Protein S deficiency . |
|---|---|---|
| Genetic mutation | PROC gene | PROS1 gene |
| Types of deficiency | Type 1 quantitative defect, low PC antigen and activity Type 2 qualitative defect, normal PC antigen but low activity • Type 2A • Type 2B—not detected by amidolytic assays | Type 1 quantitative defect; low total and free PS antigen, low activity Type 2 qualitative defect; normal total and free PS, low activity Type 3 selective quantitative defect; normal total PS, low free PS antigen, low activity |
| Activity assays | PC activity: • Clotting end point • Amidolytic end point (uses a chromogenic substrate) | PS activity: • Clotting end point |
| Antigen assays | PC antigen: immunoassays • Helps distinguish deficiency type, not required for diagnosis | PS antigen: immunoassays Free PS antigen—ELISA, latex immunoassays; initial test for diagnosis Total PS antigen—helps distinguish deficiency type, not required for diagnosis |
| Diagnostic threshold | PC activity <65%-70% | Free PS antigen <33% (in general population) <40%-50% (with patients with prior VTE or strong family history) |
| Laboratory interference | Clot-based assays: lupus anticoagulants, heparins, direct thrombin inhibitor, oral factor Xa inhibitors, elevated FVIII:C, FVL mutation, and hyperlipidemia | Clot-based assays: lupus anticoagulants, heparins, direct thrombin inhibitor, oral factor Xa inhibitors, elevated FVIII, FVL mutation, and PC deficiency |
| Conditions with acquired deficiency | Liver disease, DIC, vitamin K antagonist, vitamin K deficiency, recent surgery or trauma, acute inflammatory illnesses, oral contraceptive pills, or acquired antibodies | Liver disease, DIC, vitamin K antagonist, vitamin K deficiency, nephrotic syndrome, L-asparaginase therapy, oral contraceptive pills, pregnancy, or acquired antibodies |
DIC, disseminated intravascular coagulation; PC, protein C; PS, protein S.
The effects of oral factor Xa inhibitors and oral thrombin inhibitors on tests for hereditary thrombophilia
| Thrombophilia . | Tests . | Effect on test . |
|---|---|---|
| Factor V Leiden mutation | PCR | Not affected |
| Prothrombin G20210A mutation | PCR | Not affected |
| Protein C deficiency | Protein C activity: clot-based assays | Interference by oral factor Xa inhibitors and dabigatran |
| Protein C activity: amidolytic assays | Not affected | |
| Protein C antigen assays | Not affected | |
| Protein S deficiency | Protein S activity: clot-based assays | Interference by oral factor Xa inhibitors and dabigatran |
| Protein S antigen assays | Not affected | |
| Antithrombin deficiency | Antithrombin activity: anti-Xa–based assays | Interference by oral factor Xa inhibitors |
| Antithrombin activity: anti-IIa–based assays | Interference by dabigatran | |
| Antithrombin antigen assays | Not affected |
| Thrombophilia . | Tests . | Effect on test . |
|---|---|---|
| Factor V Leiden mutation | PCR | Not affected |
| Prothrombin G20210A mutation | PCR | Not affected |
| Protein C deficiency | Protein C activity: clot-based assays | Interference by oral factor Xa inhibitors and dabigatran |
| Protein C activity: amidolytic assays | Not affected | |
| Protein C antigen assays | Not affected | |
| Protein S deficiency | Protein S activity: clot-based assays | Interference by oral factor Xa inhibitors and dabigatran |
| Protein S antigen assays | Not affected | |
| Antithrombin deficiency | Antithrombin activity: anti-Xa–based assays | Interference by oral factor Xa inhibitors |
| Antithrombin activity: anti-IIa–based assays | Interference by dabigatran | |
| Antithrombin antigen assays | Not affected |
PCR, polymerase chain reaction.
CLINICAL CASE (continued)
The low functional protein C level was done by a commercial laboratory that uses a clotting end point, while the normal level obtained by our laboratory used an amidolytic assay. Repeat testing using an assay with a clotting end point returned low at 62%; the patient is therefore likely to have heterozygous protein C deficiency. Arrangements were made to have sequencing done to determine the mutation in the protein C gene. Regarding the implications of protein C deficiency on recurrent miscarriage, an association has not been established,49,50 nor is there evidence for a higher live birth rate in women treated with antepartum low-molecular-weight heparin.51 However, based on her having protein C deficiency and a family history of VTE, postpartum thromboprophylaxis is recommended per the ASH Guidelines.52 This, however, is an individualized decision that the patient and her physicians need to make based on her thrombotic and bleeding risk following delivery.
Nuances: diagnosing protein S deficiency
CLINICAL CASE
A 34-year-old G3P0 woman was referred with a history of 2 first-trimester miscarriages but no personal or family history of thrombosis. As part of the evaluation for in vitro fertilization, protein S activity was 57% (reference range, >64%). She was started on enoxaparin 40 mg subcutaneously daily on the day following embryo transfer. Protein S activity at 4 months' gestation was lower at 31%. She is seen regarding the need for continued prophylaxis with low-molecular-weight heparin.
This case highlights the challenge encountered in accurately diagnosing clinically relevant protein S deficiency (ie, associated with an increased risk for VTE). Protein S circulates in the blood in 2 forms, 60% bound to C4b-binding protein and 40% free.53 Tests for protein S deficiency include activity assays as well as free and total protein S antigen (Table 3). Free protein S antigen is the preferred method due to its lower variability and correlation with risk of VTE.54 In a case-control study, levels of free protein S had to be <33% (<0.10th percentile) to indicate an increased risk of venous thrombosis. No association was observed with total protein S antigen, even at levels <53% (<0.20th percentile).54 As with protein C, protein S levels are influenced by many factors that must be considered in interpreting results (Table 3).
CLINICAL CASE (continued)
This patient's mild reduction in protein S activity at baseline has no clinical significance, and the level of 31% was due to being 4 months pregnant. Hence it was recommended that prophylactic anticoagulation be discontinued; the patient and her obstetrician agreed with this plan.
Conflict-of-interest disclosure
Thita Chiasakul has nothing to declare.
Kenneth A. Bauer has served as a consultant to Abbott and Sanofi.
Off-label drug use
Thita Chiasakul: nothing to disclose.
Kenneth A. Bauer: nothing to disclose.