Abstract
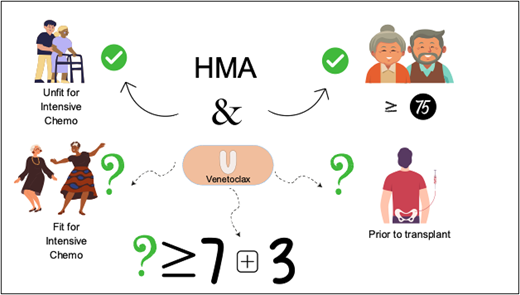
Treatment options for acute myeloid leukemia (AML) have expanded over the last 5 years. New regimens are increasing the options for patients who previously may not have been offered any antineoplastic therapy. The use of the hypomethylating agent (HMA) decitabine or azacitidine combined with the BCL2 inhibitor venetoclax (HMA-VEN) has improved overall survival in an older and unfit population compared to HMA therapy alone. Delivering these regimens outside academic centers allows more patients with AML to be treated, though support and collaboration with allogeneic stem cell transplant (SCT) centers should still be considered to determine eligibility and promptly initiate a donor search for potential transplant candidates. Expanding the use of HMA-VEN to younger and fit patients who are also candidates for intensive chemotherapy (IC) is being studied prospectively and is not recommended at this time outside of a clinical trial. Retrospective studies suggest populations that may benefit from HMA-VEN over IC, but this is not yet confirmed prospectively. Utilizing HMA-VEN prior to allogeneic SCT is also under investigation, and some retrospective data show feasibility and the ability to achieve measurable residual disease negativity pretransplant. Upcoming prospective randomized clinical trials aim to answer the comparability or superiority of HMA-VEN vs IC in fit populations and its potential use as a standard pretransplant induction regimen.
Learning Objectives
Describe the role of HMAs plus VEN in the treatment of older patients with AML
Review data from the use of HMAs plus VEN in younger, fit patients with AML
CLINICAL CASE
A 61-year-old presents with a 4-week history of fatigue and dyspnea. Progressing symptoms over the last 3 days are unexplained bruising on the arms and legs and gingival tenderness. The patient's past medical history is pertinent for diffuse large B-cell lymphoma diagnosed 3 years ago and treated with six 21-day cycles of rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone chemotherapy. The postchemotherapy treatment course was complicated by symptomatic lower-extremity edema and orthopnea 2 months after completion of chemotherapy, and subsequently the patient was found to have a decrease in cardiac ejection fraction from 65% prechemotherapy to 40%. The patient was evaluated and treated by oncocardiology with guideline-directed medical therapy. The patient's Eastern Cooperative Oncology Group (ECOG) performance status (PS) upon evaluation is 3, but history provided by the patient demonstrates an ECOG of 0 a few months ago. Mobility is severely limited, with dyspnea on exertion when arising from the chair or bed and significant fatigue, including sleeping 20 hours per day and being unable to perform some activities of daily living without assistance. The patient's complete blood count with differential 3 months ago was normal but now demonstrates a white blood cell count of 24 000 k/µL with 50% blasts, a hemoglobin level of 7.2 g/dL, and a platelet count of 65 000 k/µL. The physical examination is pertinent for normal jugular venous pressure, no peripheral edema, normal pulmonary function, mild splenomegaly, and ecchymoses. Peripheral blood flow cytometry demonstrates acute myeloid leukemia (AML). A repeat ejection fraction is 55%. Imaging demonstrates nodularity in the lung parenchyma and splenomegaly at 16 cm, both concerning for leukemic involvement. The patient is screened for available clinical trials but is excluded from open trials at the practice location due to an ECOG PS of 3. A bone marrow aspirate and biopsy confirm acute myelomonocytic leukemia without myelodysplastic changes. Rapid TP53 and FLT3 assays and fluorescence in situ hybridization studies for −5,−7,−17p,inv16,t(8;21), and MLL rearrangement are all negative. Next-generation sequencing is pending. Therapeutic options are reviewed with the patient, who opts to pursue treatment. Following the American Society of Hematology (ASH) AML guidelines, the patient is started on azacitidine (AZA) at 75 mg/m2 on days 1 through 7 and venetoclax (VEN) on days 1 through 28 per a standard dose ramp-up for days 1 through 3. The dose is then adjusted for antifungal prophylaxis with a plan for disease assessment bone marrow biopsy between days 21 and 28.1
Introduction
AML treatment remains a challenge given its significant mortality despite the approval of new therapeutic options. In 2022 the American Cancer Society reported over 20 000 new index cases, with 11 310 deaths due to AML reported.2 Of patients diagnosed with AML, only 28% of those aged 20 and older will be alive in 5 years.3 Therapy for unfit or older adults presents a challenge as some will not tolerate intensive chemotherapy (IC).
Standard therapy for younger, fit patients has been IC since the 1970s, with anthracycline given for 3 days and cytarabine infusion for 7 days (commonly referred to as 7 + 3). Therapy for unfit patients was limited, with low-dose cytarabine (LDAC) data emerging in the 1980s. In the 2000s, drug approvals for myelodysplastic syndrome (MDS) included the hypomethylating agents (HMAs) AZA and decitabine. These agents began to be used off-label shortly thereafter for the treatment of AML in patients unfit for IC based on data from cooperative group trials in the 1980s that included patients with MDS and AML.
Fitness for IC is difficult to determine in some cases and is often subjective despite the increased use of geriatric assessment tools. In a disease such as AML, fitness can be rapidly affected by the disease itself, taking a patient who was “fit” a few weeks prior to presentation to a poor PS, as in our patient. Historically, many unfit patients older than 60 may have only been offered best supportive care. In our practice, when determining initial therapy, we consider both recent performance status and performance status at time of diagnosis. Consideration of prior anthracycline-induced heart failure and presenting performance status led against recommending treatment with liposomal daunorubicin and cytarabine (CPX-351) in this patient. However, CPX-351 is approved by the US Food and Drug Administration (FDA) and demonstrated superior overall survival (OS) compared to 7 plus 3 in a randomized phase 3 trial for newly diagnosed patients aged 60 to 75 years with therapy-related AML, AML with prior MDS or chronic myelomonocytic leukemia, or de novo AML with MDS-related cytogenetic abnormalities per 2008 World Health Organization criteria.4
Historical studies have shown that older patients given IC have inferior survival compared to younger patients. A study in 2020 reported that patients aged 60 and older had a 2-year OS of 15.8% compared to 78.6% in patients aged 40 or younger.5 This location where patients receive their care also has an impact. In a 2016 retrospective study of a large community oncology practice analyzing newly diagnosed AML patients 60 years and older, only 5 of 922 patients received IC, and 43% received no antileukemic therapy.6 The majority of patients treated received single-agent HMA therapy with decitabine or AZA.6 Outcomes with single-agent HMAs were better than LDAC or best supportive care but lagged behind IC in rates of complete remission (CR), time to response, and OS, similar to reports in multiple other studies.5,7-10 Community settings face challenges in providing intensive AML chemotherapy regimens, which often require weeks in the hospital and rigorous inpatient support and experience. A retrospective study evaluating outcomes in patients treated with IC in high-volume hospitals had lower mortality compared to low-volume hospitals (odds ratio, 0.8; 95% CI, 0.67-0.95; P = .01).11
Where HMA-VEN started
The inhibition of B cell lymphoma 2 (BCL2) protein has become an intriguing target in hematologic malignancies. Inhibiting BCL2 leads to the induction of apoptosis in blood cancer cells.12 Multiple clinical trials were developed in the early 2010s utilizing VEN for treatment as a single agent or in combination therapy for a variety of hematologic malignancies. The first FDA approval came as a breakthrough designation in 2016 based on phase 2 data in chronic lymphocytic leukemia (NCT01889186) presented at the 2015 ASH annual meeting as a late breaking abstract.13 Despite all AML cells not overexpressing BCL2, leukemia stem cells have dysregulated apopotosis.14 VEN is a BCL homology domain (BH)-3 mimetic that is potent and highly selective for BCL2 (and not BCLXL, which is expressed on platelets) and able to inhibit BCL2, therefore increasing other proapoptotic factors to induce apoptosis in AML cells.15 VEN was explored in a phase 2 study by Konopleva et al, where it was used as a single agent for patients unfit for IC and for relapsed/refractory patients.16 This led to the exploration of combining it with other drugs, including HMAs. Preclinical work evaluating the synergism of VEN and HMAs ex vivo was described by Bogenberger et al in 2015.17 Azacitidine reduces the antiapoptotic gene MCL-1 and when combined with BCL2 inhibition was suggested to be moved into clinical studies. The phase 1b combination study of HMA-VEN in the frontline setting was published in 2018 by DiNardo et al and demonstrated safety, tolerability, and 60% CR and incomplete count recovery (CRi); therefore, it was the basis for future VIALE-A studies.18 When combined with AZA, data have shown that leukemia stem cells can be targeted, leading to deeper remissions and achievement of measurable residual disease (MRD) negativity.15,19
How HMA-VEN is going
The treatment landscape for this older or unfit population changed in 2018 when the FDA granted accelerated approval to decitabine, AZA, or LDAC in combination with VEN. The pivotal phase 3 VIALE-A study of AZA plus or minus VEN and the VIALE-C study of LDAC plus or minus VEN led to regular FDA approval in 2020.20
VIALE-A included newly diagnosed AML in patients unfit for IC, defining unfit as aged 74 or over or aged 18 to 74 with comorbidities ineligible for IC.21 Unfit for IC in this study was defined by a reduced cardiac ejection fraction of 50% or less, chronic angina, a pulmonary diffusion capacity of 65% or less or a forced expiratory volume of 65% or less, and a performance status of ECOG 2 or 3.21 The majority of patients were over 75 (61% in the AZA-VEN group and 61% in the AZA-placebo group).21 Patients were randomized 2:1 to receive AZA plus or minus VEN or placebo and met the primary end point of OS benefit at initial publication.19 On long-term follow up reported in 2022, OS was 14.7 (95% CI, 12.1-18.7) months in the AZA-VEN arm vs 9.6 (95% CI, 7.4-12.7) months in the AZA-placebo arm.21,22
Updated data from community settings are not yet published, but with the rise of HMA-VEN combination therapy, AML treatment in a community setting has become more feasible. The availability of transfusion support, including weekend infusion and blood product availability, remains a challenge in many places. Partnership between community and academic settings is critical for optimal outcomes of this complex patient population, with benefits including increased clinical trial options, prompt allogeneic transplant eligibility determination, and shorter time to transplant.23-25
HMA-VEN use in relapsed or refractory AML has emerged within clinical practice and been explored within several retrospective studies and a few early phase prospective studies, but use in this setting remains an off-label indication. A 2022 article by Brancati S. et al highlighted the available prospective and retrospective data of use for HMA-VEN in relapsed/refractory patients with an ORR ranging from 38% to 62%, though it pointed to a much lower ORR in patients with prior HMA exposure.26 Use as a salvage regimen requires further prospective studies.
CLINICAL CASE (continued)
Our patient, at age 61 with an ECOG PS of 3, would have met inclusion criteria in VIALE-A but would not have met inclusion criteria for liposomal CPX-351, and thus a less intensive regimen was chosen for the patient on the basis of performance status. Performance status impacted by disease burden is also a factor when determining treatment options, and IC could have been considered for this patient if the treating physician believed the symptoms to be reversible.
What is next for younger and fit patients?
The question of utilizing HMA-VEN combination for fit and/or younger patients or a direct comparator to IC has yet to be answered prospectively, but a large retrospective analysis by Cherry et al was performed on 143 patients who received AZA-VEN and 149 who received IC (Table 1).27 The CR rate was 62.2% vs 64.4% in AZA-VEN vs IC, respectively.27 Less than 25% of AZA-VEN patients went on to receive an allogeneic stem cell transplant (SCT) compared to 74.8% of those treated with IC.27 After five years, OS favored IC over AZA-VEN (884 days vs 483 days).27 Favorable survival in this case was likely largely impacted by who was offered and received allogeneic SCT, and when propensity matched controlling for age, European LeukemiaNet (ELN) risk group and transplant status, OS and progression-free survival were similar.27 (Table 1).
VEN and AZA compared with induction chemotherapy for newly diagnosed patients with acute myeloid leukemia
| . | Median OS (days) . | P . | ORR (%) . | P . | CR/CRi favored . | OS favored . |
|---|---|---|---|---|---|---|
| Entire cohort | ||||||
| HMA-VEN (n = 143) | 483 | .002 | 76.9 | .2109 | • Age >64 • RUNXI mutated • sAML | • Age >64 andRUNX1 mutated |
| IC (n = 149) | 884 | 70.5 | • Monocytic subtype | • Undifferentiated or minimal maturation subtypes • ELN intermediate risk • FLT3-ITD mutated • RAS mutated | ||
| Propensity matched for age, biological risk | ||||||
| HMA-VEN | NR | .0667 | ||||
| IC | 705 | |||||
| . | Median OS (days) . | P . | ORR (%) . | P . | CR/CRi favored . | OS favored . |
|---|---|---|---|---|---|---|
| Entire cohort | ||||||
| HMA-VEN (n = 143) | 483 | .002 | 76.9 | .2109 | • Age >64 • RUNXI mutated • sAML | • Age >64 andRUNX1 mutated |
| IC (n = 149) | 884 | 70.5 | • Monocytic subtype | • Undifferentiated or minimal maturation subtypes • ELN intermediate risk • FLT3-ITD mutated • RAS mutated | ||
| Propensity matched for age, biological risk | ||||||
| HMA-VEN | NR | .0667 | ||||
| IC | 705 | |||||
NR, not reached; ORR, overall response rate; sAML, secondary AML.
Reproduced from Cherry et al.27
CPX-351 was also retrospectively compared to AZA-VEN and included 217 patients who received CPX-351 and 439 who received AZA-VEN with a median OS of 13 months and 11 months, respectively (hazard ratio [HR] 0.88; 95% CI, 0.71-1.08; P = .22).28 Of the 217 who received CPX-351, 61 (28%) went on to allogeneic SCT, and 44 (10%) underwent allogeneic SCT in the AZA-VEN group, with SCT in both groups improving OS (HR, 0.33; P ≤ .0005) regardless of the choice of therapy (HR, 0.97; P = .78).28 The COVID-19 pandemic prompted the United Kingdom to expand the use of VEN to favorable-risk patients over 16 years of age with NPM1 mutations (FLT3-ITD negative), patients under 50 with NPM1 or IDH1/2 mutations, and patients under 60 without favorable-risk cytogenetics.29 Of the 301 patients registered, 85% received the AZA-VEN combination and 15% the LDAC and VEN, with a median age range that still skewed older at 72 (range, 34-90).29 The composite CR rate was 70%, with higher rates seen in de novo, NPM1-mutated, IDH1/2-mutated, and ELN-favorable risk patients. Median OS in all patients was 12.8 months, with 71% of those who achieved CR with CRi alive at 1 year.29
IC has been the backbone of AML treatment for decades, with HMA-VEN thus far being the closest to having some equivalency to standard 7 plus 3 induction. The applicability of HMA-VEN to all patients is unlikely, but vigorous and thoughtful clinical trial design will hopefully lead to IC alternatives to reduce toxicity and hospitalization while retaining similar or superior efficacy.
Is HMA-VEN or IC better in certain populations?
In older populations, HMA-based induction has had some traction in favorable-risk AML patients excluded from the VIALE-A study population. A retrospective study presented at the 2021 ASH annual meeting reviewed ELN 2017 favorable-risk patients aged 70 and older. Ball et al found a 97% CR plus CRi rate, vs 66% in IC-treated patients (P = .0002).30 Similar findings with NPM1-mutated patients have been seen retrospectively when compared with IC.31 The CR rate was 89% in the HMA-VEN group and 85% in the IC group (P = .778; with median age significantly younger in the IC group, at 72 years vs 55 years, respectively).31 Most notably, there was reduced risk of death in this older population compared to IC (HR, 0.31; 95% CI, 0.12-0.83; P = .038).31
Genomic subgroups are emerging that may also impact the choice of induction therapy between IC and HMA-VEN. Cherry et al identified RUNX1 mutations favoring HMA-VEN (Table 1).27 IDH1/2 mutations were analyzed in the VIALE-A patient population and demonstrated composite CR rates of 79% and OS of 24.5 months.32 When split out, IDH2 mutations had a composite CR rate of 86% compared with 66.7% in the IDH1-mutant patients, and both maintained an advantage despite the cytogenetic risk group.32 TP53 mutations were also analyzed in the VIALE-A population, with OS of 5.2 months in the AZA-VEN group vs 4.9 months in the AZA monotherapy group, demonstrating no meaningful improvement in survival with the addition of VEN to AZA.33 There was statistically significant improvement in the composite CR of AZA-VEN over AZA (41% vs 17%).33 However, without improvement in OS the added toxicity of VEN calls its benefits into question in this population. A monocytic subtype was identified by Cherry et al (Table 1) as conferring an advantage to IC over HMA-VEN.27 Pei et al also identified a loss of BCL2 target and heavy dependence of MCL-1 in monocytic AML and suggested using flow cytometry to distinguish monocytic AML as a more mature entity and a potential future target to overcome resistance.34
The use of HMA-VEN instead of IC in younger, fit patients is the subject of current prospectively enrolling trials (Table 2). One is NCT03573024, a single-arm study enrolling fit patients aged 18 to 59, all receiving the AZA-VEN combination. Another phase 2 randomized, multicenter study comparing AZA-VEN to IC (7 + 3 or CPX-351) in fit, newly diagnosed patients is also currently enrolling (NCT04801797). The soon to launch National Cancer Institute–sponsored collaborative MyeloMATCH studies will enroll intermediate-risk (NCT05554393) and high-risk (NCT05554406) patients aged 18 to 59 to answer the question of IC plus or minus VEN vs HMA-VEN. Patients in the high-risk study will be randomized to 1 of 5 arms: cytarabine and daunorubicin (7 + 3); cytarabine, daunorubicin, and VEN (7 + 3 + VEN); AZA-VEN; CPX-351; CPX-351 and VEN. It is hoped that these trials will help determine outcomes for fit patients utilizing regimens other than the traditional 7 plus 3.
Prospective studies evaluating younger, fit patients eligible for IC compared to AZA-VEN
| Study . | Phase . | Type . | Therapy . | Key inclusion . | Key exclusion . |
|---|---|---|---|---|---|
| NCT04801797 | II | Randomized | • IC • AZA-VEN | • Age 18+ • ECOG ≤2 | • FLT3 • Age <60 with NPM1 mutated • Favorable risk |
| NCT03573024 | II | Single arm | • AZA-VEN | • Age 18-59 • ECOG ≤2 • Adverse risk | • Willing to receive IC |
| NCT05554393 (MyeloMATCH) | II | Randomized | • 7 + 3 • 7 + 3 + VEN • AZA-VEN | • Age 18-59 • ECOG 0-3 | • Favorable and adverse risk by ELN 2017 criteria • FLT3-ITD/TKD • Secondary or therapy-related AML |
| NCT05554406 (MyeloMATCH) | II | Randomized | • CPX-351 • 7 + 3 • AZA-VEN • 7 + 3+ VEN • CPX-351 + VEN | • Age 18-59 • ECOG 0-3 • Adverse risk per ELN 2017 criteria | • Favorable or intermediate risk • FLT3- ITD/TKD |
| Study . | Phase . | Type . | Therapy . | Key inclusion . | Key exclusion . |
|---|---|---|---|---|---|
| NCT04801797 | II | Randomized | • IC • AZA-VEN | • Age 18+ • ECOG ≤2 | • FLT3 • Age <60 with NPM1 mutated • Favorable risk |
| NCT03573024 | II | Single arm | • AZA-VEN | • Age 18-59 • ECOG ≤2 • Adverse risk | • Willing to receive IC |
| NCT05554393 (MyeloMATCH) | II | Randomized | • 7 + 3 • 7 + 3 + VEN • AZA-VEN | • Age 18-59 • ECOG 0-3 | • Favorable and adverse risk by ELN 2017 criteria • FLT3-ITD/TKD • Secondary or therapy-related AML |
| NCT05554406 (MyeloMATCH) | II | Randomized | • CPX-351 • 7 + 3 • AZA-VEN • 7 + 3+ VEN • CPX-351 + VEN | • Age 18-59 • ECOG 0-3 • Adverse risk per ELN 2017 criteria | • Favorable or intermediate risk • FLT3- ITD/TKD |
CLINICAL CASE (continued)
Returning to the clinical case, our patient clinically improved during treatment with VEN and AZA. By treatment day 5, the patient had improved dyspnea, and ECOG PS had improved to 2. Diagnostic testing demonstrated an NRAS mutation using next-generation sequencing and trisomy 8 using cytogenetics. The patient underwent evaluation by an allogeneic SCT physician, and a donor search was initiated. On day 21, a bone marrow biopsy was performed, which was 5% cellular with 1% blasts. VEN was held at this time, and upon absolute neutrophil count and platelet recovery 10 days later, the patient began cycle 2 of VEN-AZA, with an improved ECOG performance status of 1. Bone marrow aspiration/biopsy upon count recovery after cycle 2 demonstrated a normocellular marrow and 2% blasts (immunophenotypically normal). Multiparameter flow cytometry was negative along with normalization of cytogenetics, and NRAS mutation was not detected.
When does allogeneic SCT fit in with non-IC induction therapy?
One might think that if patient factors lead to the choice of a non-IC strategy such as HMA-VEN, then allogenic SCT is unlikely. Patients on HMA-VEN can show improvement in leukemia symptoms and therefore improved fitness and proceed to allogenic SCT. Several retrospective studies utilizing AZA-VEN as a path to allogeneic SCT demonstrated the feasibility of obtaining favorable outcomes and MRD negativity (Table 3). This is highlighted in a study showing that for patients who achieved a CR, CRi, or morphologic leukemia-free state, 70% of patients achieved MRD negativity by multiparameter flow cytometry in the AZA-VEN group compared to 64% in the IC arm (1 patient in the IC arm had refractory disease prior to allogeneic SCT).35 Another study showed that those achieving a CR and MRD negativity with AZA-VEN, either in the frontline or relapsed settings, and then proceeding to SCT demonstrated a 1-year OS of 90% and 78%, respectively, and that those who proceeded to up-front allogeneic SCT lived longer than those who delayed allogeneic SCT.36,37
Currently reported studies utilizing HMA-VEN for remission induction prior to allogeneic SCT
| Study . | Type . | Participating sites . | Number of patients . | 12-month NRM (%) . | 12-month CIR . | 12-month RFS (%) . | 12-month OS (%) . | Relapse (%)/median LFS (month) . | OS (months) . |
|---|---|---|---|---|---|---|---|---|---|
| Pasvolsky et al35 | Retrospective | Multicenter | 24 | 19.1 | 58 | 63 | |||
| Winters et al36 | Retrospective | Single center | 29 | 66.1 | 74.5 | ||||
| Pollyea et al37,38 | Retrospective | Single center | 21 | 11 | 80 | NR | |||
| Kennedy et al39,40 | Retrospective | Multicenter | 88 | 17 | 18 | 73 | |||
| Nizamuddin et al41 | Retrospective | Single center | 36 | 39/11.2 | 25.4 | ||||
| Rautenberg et al42 | Retrospective | Single center | 26 | 67 | 81 | NR |
| Study . | Type . | Participating sites . | Number of patients . | 12-month NRM (%) . | 12-month CIR . | 12-month RFS (%) . | 12-month OS (%) . | Relapse (%)/median LFS (month) . | OS (months) . |
|---|---|---|---|---|---|---|---|---|---|
| Pasvolsky et al35 | Retrospective | Multicenter | 24 | 19.1 | 58 | 63 | |||
| Winters et al36 | Retrospective | Single center | 29 | 66.1 | 74.5 | ||||
| Pollyea et al37,38 | Retrospective | Single center | 21 | 11 | 80 | NR | |||
| Kennedy et al39,40 | Retrospective | Multicenter | 88 | 17 | 18 | 73 | |||
| Nizamuddin et al41 | Retrospective | Single center | 36 | 39/11.2 | 25.4 | ||||
| Rautenberg et al42 | Retrospective | Single center | 26 | 67 | 81 | NR |
CIR, cumulative index of relapse; NR, not reached; NRM, onrelapse mortality; RFS, relapse free survival; LFS, leukemia free survival.
Prospective studies remain a need in this space. Gruppo Italiano Trapianto di Midollo Osseo recently completed a prospective multicenter study exploring HMA-VEN as a cytotoxic chemotherapy-free bridge to allogeneic SCT and enrolled newly diagnosed AML patients aged 60 to 75. Patients were treated with decitabine and VEN, and those who achieved CR, CRi, or morphologic leukemia-free state after 2 cycles proceeded to allogeneic SCT (NCT04476199). We eagerly await the results.
Conclusion
Our patient had a matched unrelated donor and proceeded to allogeneic SCT after achieving an MRD-negative CR after 2 cycles. The use of a nonintensive remission-induction strategy in this patient highlights the ability to improve initial performance status with disease control and shows that early evaluation for allogeneic SCT can improve outcomes for patients previously excluded from any antileukemic therapy. The use of HMA-VEN in a younger, fit population is best studied in the context of clinical trials, as its benefit over IC is yet to be demonstrated prospectively. HMA-VEN combinations expand options for antileukemia treatment beyond academic centers and large cities, and collaboration with leukemia centers is recommended for optimal long-term treatment planning for this complex patient population.
Conflict-of-interest disclosure
Heather J. Male: research funding: Takeda, Chimerix, Jazz Pharmaceuticals.
Tara L. Lin: research funding: Bio-path Holdings, Astellas Pharma, Celyad, Aptevo Therapeutics, Cardiff Oncology, Cleave Biosciences, Ciclomed, Jazz Pharmaceuticals.
Off-label drug use
Heather J. Male: Nothing to disclose.
Tara L. Lin: Nothing to disclose.