Abstract
This is a focused clinical vignette and review of the literature in MDS to discuss the application of molecular sequencing for risk stratification in MDS. The authors utilize an exemplar patient case and explain the advantages and disadvantages, based on available data, of routine use of this testing for MDS patients.
Learning Objectives
Review the prognostic significance of mutational profiles in MDS
Identify appropriate approaches to use molecular profiling for risk stratification in MDS
CLINICAL CASE
A 67-year-old woman sought treatment for progressive fatigue initially attributed to caring for her 18-month-old grandson. She was found to have pancytopenia (hemoglobin of 10.2 g/dL, mean cell volume of 104 fL, platelet count of 77 × 109/L, and white blood cell count of 2.1 × 109/L with absolute neutrophil count of 0.7 × 109/L). Bone marrow biopsy specimen demonstrated trilineage dysplasia with 1% blasts. Cytogenetics were 46,XX [20]. International Prognostic Scoring System - Revised (IPSS-R) risk category was low. Mutational testing demonstrated mutations in ASXL1 (variant allele fraction [VAF] 34%), SRSF2 (VAF 42%), TET2 (VAF 18%), and SETBP1 (VAF 12%). Does this molecular profile modify risk stratification or management decisions in this patient?
Introduction
Myelodysplastic syndromes (MDS) are a group of related hematologic neoplasms that cause dysplasia and ineffective hematopoiesis and have a propensity to progress to acute myeloid leukemia (AML). The diagnosis of MDS requires morphologic dysplasia in 1 or more cell lines and/or characteristic cytogenetic abnormalities. Over the past decade, the development of next-generation sequencing (NGS) assays has allowed for the identification of more than 50 different recurrent driver gene mutations that are associated with MDS.1,2 Most patients with MDS will have at least 1 identified somatic mutation, whereas a typical patient will harbor a median of 2 or 3 driver mutations.3 NGS assays are increasingly used in the diagnostic evaluation of patients with cytopenias.4 Numerous studies have also evaluated the prognostic significance of such mutations. Best practices for integrating molecular testing into existing risk prediction modeling have yet to be established, and substantial clinical variability exists among practicing hematologists.5 Here we review the current evidence for use of molecular profiling to guide risk stratification in clinical practice.
Molecular precision
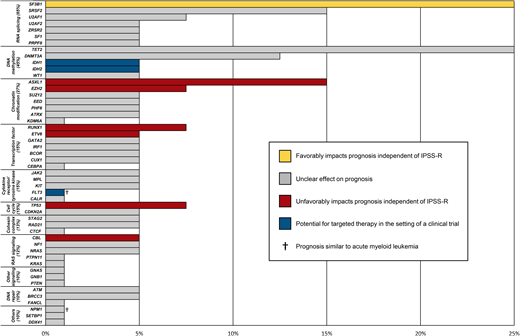
Several notable studies using NGS and high-throughput sequencing have demonstrated the independent prognostic significance of recurrent molecular mutations in patients with MDS. Consistently identified driver mutant genes include mutations involved in RNA splicing (SF3B1, SRSF2, U2AF1, and ZRSR2), DNA methylation (TET2, DNMT3A, IDH1, and IDH2), chromatin modification (ASXL1 and EZH2), transcription regulation (RUNX1), DNA repair (TP53), and signal transduction (CBL, NRAS, and KRAS).6
Papaemmanuil et al1 sequenced 111 genes across 738 patients with MDS, chronic myelomonocytic leukemia, and MDS/myeloproliferative neoplasms. Mutations in SF3B1 (24%), TET2 (22%), and SFSF2 (14%) were most common, followed by ASXL1, DNMT3A, RUNX1, U2AF1, TP53, and EZH2. Mutations in TP53, U2AF1, RUNX1, SRSF2, IDH2, CUX1, ASXL1, and BCOR were negatively associated with overall survival (OS), whereas mutations in SF3B1 were associated with improved OS. Leukemia-free survival was negatively associated with increased number of driver mutations and cytogenetic abnormalities.
Bejar et al7 in a study using NGS and mass spectrometry–based genotyping of 439 patients with MDS demonstrated that mutations in 10 genes were associated with OS (TET2, ASXL1, RUNX1, TP53, EZH2, NRAS, JAK2, ETV6, CBL, and IDH2). Mutations in 6 genes (TP53, EZH2, ETV6, RUNX1, CBL, and ASXL1) negatively affected OS after adjusting for IPSS risk group and age. The presence of a TP53 mutation had the largest independent association with survival among mutations (hazard ratio, 2.48).
Haferlach et al3 used high-throughput deep sequencing of 104 genes to analyze the genomic and clinical data of more than 900 patients with MDS. Twenty-five genes were identified to be associated with survival outcomes on univariate analysis. Only mutations in SF3B1 were associated with an improved clinical outcome. Other recent analyses confirm the importance of mutations identified in these studies, highlighting the prognostic value of specific mutations independent of IPSS-R.5,8
Variant allele frequency is the percentage of variant reads in the total number of reads (variant plus reference reads) and is used to approximate the proportion of DNA molecules in the original specimen that carry the specific variant. Traditionally, mutations with a VAF of 5% or less are not thought to be clinically significant. More data are emerging that prognostic outcomes associated with individual mutations may be dependent on the VAF of mutations, although this effect may be limited to certain mutations (such as TP53, TET2, and SF3B1).9-12 In TP53-mutated MDS, for example, increasing VAF was associated with worse prognosis, with an increase in hazard ratio of 1.02% per 1% VAF increase.13 Patients with a low TP53-mutational burden (VAF <10%) and without a complex karyotype may have outcomes better than expected. Those patients with a high VAF are less likely to respond to hypomethylating agents.13
Molecular profiling is also essential in estimating risk for patients with clonal hematopoiesis of indeterminate potential (CHIP) and clonal cytopenia of undetermined significance (CCUS), precursor states to MDS. For example, in patients with CCUS, mutational status is predictive of risk of progression: mutations in U2AF1, ZRSR2, SRSF2, JAK2, or RUNX1 are associated with a high risk of progression to MDS (as high as 80%-90% at 5 years), whereas isolated mutations in TET2, ASXL1, and DNMT3A are associated with a lower risk of progression (~50% at 5 years).14 Similar to findings in MDS, emerging data have demonstrated that different mutational patterns and VAF values are likely important in predicting overall risk in CHIP and CCUS.15
Although identification of somatic mutations by NGS is an important step forward in risk stratification for patients with MDS, individual mutations are only a part of a more complex landscape of genomic abnormalities that drive pathology and determine outcomes. Using the same cohort of 944 patients mentioned above, Haferlach et al3 proposed novel prognostic models incorporating genetic data that stratify patients into 4 prognostically distinct subgroups. These models consistently outperformed IPSS-R, demonstrating the feasibility and importance of incorporating molecular data into prognostic models. By applying computational approaches to large international databases, Bersanelli et al16 explored the complexity of multiple coexisting mutations and identified 8 prognostically distinct “genomic subtypes” of MDS such as MDS with TP53 mutations and/or complex karyotype, MDS with AML-like mutational patterns, and SRSF2-related MDS. Furthermore, by integrating 63 clinical and genomic variables, the authors were able to develop a model to generate an estimated personalized probability of survival, which also significantly improved upon IPSS-R prognostication. Such approaches likely better represent the disease biology in MDS, but further work needs to be done to demonstrate the utility of such complex risk stratification systems for clinical decision making.
Clinical uncertainty
Despite the remarkable technological progress that has enabled rapid molecular profiling of patients with MDS and precursor states, substantial clinical uncertainty remains about how to apply molecular data to individual patients. Numerous prognostic models have already been validated for use in MDS and are in widespread use, including the IPSS, MDS WHO Classification-based Prognostic Scoring System (WPSS), Lower-Risk Prognostic Scoring System (LR-PSS), Global MD Anderson Prognostic Scoring System (MDAPSS), French Prognostic Scoring System (FPSS), and IPSS-R, among others. Multiple novel models have been proposed that seek to combine existing prognostic scoring systems with mutational data from emerging studies.1,3,16 Clinical use of these advanced models incorporating genetic data is currently limited due to the complexity of the models and the lack of further validation studies. A standard scoring system incorporating molecular data and clinicopathologic data remains to be established.
The lack of an accepted prognostic scoring system incorporating molecular data makes prognostication for individual patients particularly challenging. Hematologists already face the challenge of determining which existing risk prediction model best applies to each patient; the addition of molecular profiling adds yet another layer of complexity and clinical uncertainty. Multiple questions remain: Are the adverse effects of mutations on outcomes uniform across standardized risk models? Are they uniform across risk categories? Is there a ceiling effect to adverse prognostic factors? For patients with multiple mutations identified, how should risk be estimated? Multiple studies have demonstrated the adverse effect of having multiple coexisting mutations.1,3,7 Should this “comutation” effect be thought of in parallel or in sequence to the effect of individual mutations? These questions, along with many others, remain to be addressed to improve risk stratification for patients with MDS.
Implications for clinical practice
Although the use of molecular profiling adds complexity to prognostication and obtaining NGS is often hindered by the lack of insurance coverage, we suggest completing molecular profiling on all patients suspected or confirmed to have MDS. The reason for this is straightforward: in some patients, molecular profiling will substantially change management. For the patient mentioned above, although IPSS-R risk is low, several features of the molecular profile are important. The ASXL1 mutation, assuming it is a canonical mutation resulting in a reading frameshift, has been shown to be associated with worse outcomes independent of IPSS-R.7 Furthermore, the fact that 4 oncogenic mutations were identified also portends worse outcomes. The median leukemia-free survival for patients with 4 identified mutations was only 18 months in the study by Papaemmanuil et al.1 So, although by IPSS-R, this patient is low risk (estimated OS of 5.3 years and leukemia-free survival of 10.8 years), the molecular profile should prompt more frequent clinical monitoring and make consideration of early therapy reasonable, including discussions of an allogeneic stem cell transplant candidacy. Several additional scenarios require mentioning.
Upstaging lower-risk disease
Patients with lower-risk MDS often experience long-term survival without the need for aggressive therapy such as allogeneic hematopoietic cell transplant. The identification of patients who are higher risk for disease complications is important to guide therapeutic decisions. In a large analysis of patients predicted to have lower-risk MDS by MDS-LR, the identification of a mutation in EZH2 predicted worse-than-expected outcomes after adjusting for multiple relevant covariates.17 Similarly, the finding of a mutation with an independent poor prognostic significance, including ASXL1, SRSF2, ETV6, RUNX1, and TP53, in patients should prompt consideration of earlier initiation of disease-modifying therapy and/or closer clinical monitoring as in the case above. Furthermore, the identification of a mutation in NPM1 (~4% of cases) has been associated with an aggressive disease course and relatively rapid progression to AML often within 12 months of diagnosis.18 Treating patients with NPM1 mutations similar to patients with AML with intensive chemotherapy and allogeneic stem cell transplant has been associated with improved outcomes.19 Similarly, FLT3 mutations, which are less frequent in MDS compared with AML (~2% vs 35%), are associated with a complex karyotype and a more rapid progression to AML, although the data are mixed.20-22 The identification of a new FLT3-ITD mutation at the time of progression from MDS to AML is associated with dismal outcomes (1 month median OS).23
SF3B1-mutated MDS
SF3B1-muated MDS is often considered a distinct subtype of MDS with an indolent course.24 SF3B1 mutations have a positive prognostic value on OS and risk of progression. This favorable effect on prognosis is independent of IPSS-R for very low and low IPSS-R categories but is not retained for high- or very high-risk groups.24 Comutations mediate this effect. Mutations in epigenetic regulators, including TET2, DNMT3A, and ASXL1, do not appear to affect survival of patients with an SF3B1 mutation, whereas RUNX1 and EZH2 mutations have a significant association with increased risk of disease progression and decreased OS independent of IPSS-R.24,25
The presence or absence of a TP53 mutation
The adverse prognostic effect of TP53 mutations in MDS has long been recognized. In patients with an isolated deletion in 5q, 20% of patients harbor a TP53 mutation that confers a higher risk to AML progression, worse OS, and early progression in lenalidomide-treated patients.26 TP53 mutation status also appears critical to mediate the adverse effect of a complex karyotype. Patients with a complex karyotype without a TP53 mutation have significantly better survival than would be suggested from prognostication based on karyotyping alone.27 In both cases, the presence or absence of a TP53 mutation could substantially alter clinical management. Specifically, we would highly consider enrollment in a clinical trial for patients with a complex karyotype and a TP53 mutation due to recently emerging encouraging results of small molecules that induce apoptosis in TP53-mutated cells such as APR-246. Response rates of more than 70% with a 50% complete remission rate were shown in 29 patients with MDS receiving APR-246 on the phase 1b/2 trial.28
Targetable mutations
Although there are currently no therapies approved by the US Food and Drug Administration that target individual mutations in MDS, the identification of specific mutations may make a patient eligible for AML-style treatments in which targeted agents are approved or for a clinical trial. Current therapeutic clinical trials include patients with identified mutations in TP53 (ClinicalTrials.gov Identifier: NCT04638309), IDH1 (numerous studies including NCT03173248, NCT03503409, NCT03839771), IDH2 (NCT04522895, NCT03839771, NCT03383575), RUNX1 (NCT04874194), TET2 (NCT03397173), FLT3 (NCT04493138, NCT04027309), CBL (NCT04493138), and multiple mutations (NCT02670525).
Existing challenges
Obtaining quality molecular profiling on some patients remains a challenge. Many insurance companies deny coverage for NGS assays or require prior authorization that may be difficult to obtain. We encourage clear coding as MDS to help with billing coverage. A letter of medical necessity citing the National Comprehensive Cancer Network guidelines may also be of use.
Some reference laboratories are not routinely reporting VAF, which substantially limits the interpretation of data, and/or are not clearly delineating whether individual mutations are pathogenic. A consensus panel by the Association for Molecular Pathology with liaison representation from the American College of Medical Genetics and Genomics, American Society of Clinical Oncology, and College of American Pathologists recommends a 4-tiered reporting approach: tier I, variants with strong clinical significance; tier II, variants with potential clinical significance; tier III, variants of unknown clinical significance; and tier IV, variants deemed benign or likely benign.29 Importantly, according to the American College of Medical Genetics and Genomics guidelines, a variant of uncertain significance should not influence clinical decision making. NGS may also identify a germline variant (eg, biallelic mutation in CEBPA, RUNX1, or other genes often evidenced by a VAF of around 50%), which may have immediate practical implications for donor selection if the patient is a transplant candidate, and influence family members.30 Referral to a genetic counselor is reasonable when germline mutations are a consideration.
Conclusion
In summary, we recommend the use of NGS to provide clinicians with additional information for risk stratification for patients with MDS. Conclusive recommendations of how to integrate current risk prognostication systems and molecular profiles cannot be made based on the variability in data quality and heterogenous effects of mutations on patients. Treatment decisions must be made on a case-by-case basis with therapy aligned with patient preferences. Increasingly, we are seeing the demonstration of the association between molecular profiles and clinical features that can predict prognosis independent of clinical scoring systems. The development of validated prognostic models, inducing molecular data, will bring great value to the field. Hopefully, we are not too far away from this being a reality. The International Working Group for the Prognosis of MDS and the MDS Foundation are progressing in the development of an integrated clinical-molecular database that should support the development of “IPSSR-Molecular.”
Recommendations
The recommendations are labeled as either “strong” or “conditional” according to the GRADE approach.
- (1)
For all patients suspected of having or confirmed to have MDS, the authors recommend molecular profiling with NGS to identify relevant mutations (strong recommendation based on moderate certainty in the evidence of effects).
- (2)
For patientpdfs found to have canonical mutations in genes known to contribute to survival outcomes (eg, SF3B1, ASXL1, SRSF2, ETV6, RUNX1, and TP53), the authors suggest clinicians incorporate the potential additional risk into existing prognostic scoring systems (conditional recommendation based on low certainty in the evidence of effects).
- (3)
For patients who are eligible based on molecular profiles, the authors suggest clinicians should offer enrollment in a clinical trial to patients (conditional recommendation based on low certainty in the evidence of effects).
- (4)
For all patients with MDS, the authors recommend assessing patient preferences to align treatment recommendations with patients' willingness to tolerate risks for benefits (strong recommendation based on moderate certainty in the evidence of effects).
Conflict-of-interest disclosure
Daniel R. Richardson: no conflicts to disclose.
Amy E. DeZern has received consultancy fees from BMS, Abbvie, Novartis, and Taiho.
Off-label drug use
Daniel R. Richardson: nothing to disclose.
Amy E. DeZern: nothing to disclose.