Abstract
In this last decade, one of the major advances in the management of multiple myeloma has been the introduction of the novel agents thalidomide, bortezomib, and lenalidomide as part of frontline treatment in young patients eligible for high-dose therapy (HDT) and autologous stem cell transplantation (ASCT). These drugs have markedly improved the rate of complete remission both before and after ASCT without substantially increasing toxicity. The implementation of an “optimal strategy” consisting of novel-agent-based induction, HDT, and the use of novel agents in consolidation and maintenance may result in a 5-year survival rate of 80% and cure might be considered in a subset of patients who present with good prognostic features at the time of diagnosis. Nevertheless, the high efficacy of the novel agents has led some groups to test these agents upfront without ASCT. At the end of 2014, preliminary randomized data favor early ASCT plus novel agents over novel agents alone. Therefore, the optimal approach to the treatment of multiple myeloma is still to propose the most effective treatment that should involve the use of frontline ASCT in young patients eligible for HDT.
Learning Objective
To understand that, in the era of novel agents, frontline ASCT remains the standard of care in young patients with MM eligible for HDT
Introduction
When considering high-dose therapy (HDT) and autologous stem cell transplantation (ASCT) for the treatment of young patients with symptomatic multiple myeloma (MM), we have to consider 2 distinct time periods, the first one before and the second one after the introduction of novel agents. The former period, which corresponds to the 1990s, provided the proof-of-concept regarding the benefit of early ASCT and resulted in the procedure becoming the standard of care,1,2 whereas the introduction of the novel agents has led to the questioning of the role of this technique as part of frontline treatment.3 Indeed, some physicians hold the view that MM can be managed in some cases with novel drugs only and can be converted to a chronic disease in selected patients. This comes at the very time when important advances in the understanding of the biology of the disease may lead some physicians to believe that a risk-adapted strategy should be used routinely, with biological parameters guiding treatment decisions in daily practice. Nevertheless, many arguments are strongly supporting the continued integral role of ASCT as part of systematic treatment of MM.
Frontline ASCT before the era of novel agents
Considering first the 1990s, a literature search reveals that 7 randomized trials investigated the use of conventional chemotherapy (CCT) versus HDT and ASCT in younger patients with de novo MM (for review, see Moreau et al4 ). In all of them, the response rate was in favor of ASCT, in 6/7 event-free survival was in favor of ASCT and in 3/7 there was an overall survival (OS) benefit associated with HDT and ASCT. Among the studies comparing CCT with ASCT, only one was specifically designed to address the question of early versus late ASCT.5 On an intent-to-treat basis, the estimated median OS was 64.6 months in the early ASCT group and 64 months in the late group (P = .92), but the average time without symptoms, treatment, and treatment toxicity was longer in the group of patients undergoing early HDT, indicating that the quality of life was improved in this group. With the exception of this single trial, none of the randomized studies mentioned above evaluated the differences observed in quality of life between the 2 therapeutic options. Overall, the conclusions of the studies conducted in the 1990s were that ASCT results in improved response rates and better event-free survival with an OS benefit observed in some trials. As a result, frontline ASCT became the standard treatment, which has since then been systematically offered to the majority of young eligible patients.1,2,4
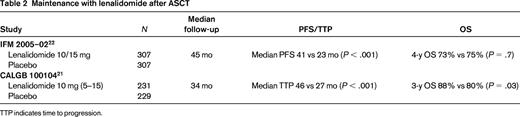
Frontline ASCT over the last decade: incorporation of novel agents into the ASCT scenario (Tables 1, 2).
Phase 3 trials incorporating novel agents in the ASCT setting: induction
Mel200 indicates melphalan 200 mg/m2; Dm, dexamethasone maintenance; ORR, overall response rate; VGPR, very good partial response; PR, partial response; IFNm, IFN maintenance; Tm, thalidomide maintenance; VTm, bortezomib-thalidomide maintenance; VBMCP, vincristine, BCNU, melphalan, cyclophosphamide, prednisone; VBAD, vincristine, BCNU, doxorubicin, dexamethasone; V, bortezomib; NR, not reported; Vm, bortezomib maintenance; and TTP, time to progression.
In this last decade, the major advance in the management of MM has been the introduction of the novel agents thalidomide, bortezomib, and lenalidomide into the therapeutic armamentarium. The novel agents have markedly improved the rate of complete remission (CR) both before and after ASCT without substantially increasing toxicity, which has important implications because the achievement of high-quality responses is a significant prognostic factor for outcome.6 The rate of very good partial responses increased from 15% after induction with the VAD (vincristine, doxorubicin, dexamethasone) regimen, the standard in the 1990s, up to 70% using triplet drug bortezomib-dexamethasone–based combinations, which are further upgraded with melphalan 200 mg/m2 as the conditioning regimen before ASCT.4,6 Regarding induction therapy, the addition of a third agent to bortezomib-dexamethasone [eg, thalidomide (VTD), doxorubicin (PAD), lenalidomide (RVD), or cyclophosphamide (VCD)] has shown higher response rates in phase 2 trials.4,6 Three prospective studies have already shown that VTD is superior to TD or bortezomib-dexamethasone.7-9 No data from phase 3 trials are yet available to assess the superiority of one combination, VTD, RVD, VCD, PAD, etc, over another. Nevertheless, the recent phase 2 EVOLUTION study suggests that RVD and VCD yield similar results.10 Based on response rates, depth of response, and progression-free survival (PFS) as surrogate markers for outcome, 3-drug combinations including at least bortezomib and dexamethasone are in 2014 the standard of care before ASCT.11-13 Three to 4 courses are recommended before proceeding to stem cell collection.11,12
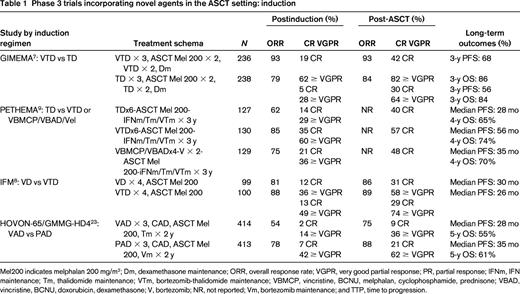
In addition, novel-agent-based consolidation therapy after ASCT14-16 has resulted in the achievement of deep molecular- or flow-cytometry-defined complete responses, with some patients remaining alive and free of disease with a minimal residual disease (MRD) negativity, which are vital prerequisites for extended disease-free survival.17-19 These unprecedented results were previously only achieved in the context of allogeneic transplantation, the routine use of which is not recommended outside of clinical trials in MM because of excessive transplantation-related mortality.20 Recent data also show that maintenance after HDT may dramatically increase PFS by almost 2 years.21-23 Indeed, the implementation of an “optimal strategy” consisting of novel-agent-based induction, HDT, and the use of novel agents in consolidation and maintenance may result in a 5-year survival rate of 80%, which is unprecedented, and cure might be considered in a subset of patients who present with good prognostic features at the time of diagnosis.24,25 The long-term results of the nonrandomized Total Therapy III (TT3) study best exemplify what is achievable by combining novel agents with ASCT in a comprehensive treatment program.24 With a median follow-up of 5.5 years, the 5-year estimates of OS and PFS are 73% and 62%, respectively. Patients enrolled in this study had near-normal, interval-specific relative survival ratios (a ratio equal to 1 suggests the mortality rate has normalized or matches the mortality of the general population) almost from the outset of therapy. This reduction in mortality to the level of the general U.S. population in TT3 speaks to the efficacy of this treatment approach. Similarly, the recent phase 2 Intergroupe Francophone du Myelome (IFM) 2008-01 trial combining triplet VRD induction, ASCT prepared by melphalan 200 mg/m2, short consolidation with VRD, and 1-year maintenance with lenalidomide in 31 patients yielded impressive 3-year PFS and OS rates of 77% and 100%, respectively.25 Overall, 58% of patients achieved CR and 68% were MRD negative by flow cytometry (CMF) at the completion of therapy. With a median follow-up of 39 months, none of the MRD-negative patients had relapsed. This regimen is being further evaluated in the ongoing IFM/Dana-Farber Cancer Institute (DFCI) 2009 phase 3 study.
Novel agents alone are questioning the role of frontline ASCT
The high efficacy of the novel agents has led some groups to test these agents upfront without ASCT and interesting results have recently been reported. Lenalidomide plus low-dose dexamethasone (len/dex) as part of frontline therapy without ASCT yielded similar survival rates at 2 years compared with len/dex followed by ASCT in a nonrandomized trial conducted by the Eastern Cooperative Oncology Group (ECOG).26 Furthermore, in a nonrandomized phase 2 trial of RVD (lenalidomide, bortezomib, dexamethasone) in the upfront setting, in which the choice of proceeding to HDT or not was based on physician or patient preference, no difference in outcome was seen for the 2 approaches.27 More recently, Jakubowiak et al reported the results of a phase 1/2 study of carfilzomib in combination with lenalidomide and low-dose dexamethasone (CRd) as frontline therapy in 53 patients with newly diagnosed MM.28 In this trial, without the incorporation of ASCT, 42% of patients reached stringent CR (sCR), defined by CMF after a median of 12 cycles, with an impressive 24-month PFS estimate of 92%. Another recent phase 2 study applied 8 cycles of the same CRd combination without upfront ASCT, followed by lenalidomide maintenance in 36 patients with newly diagnosed MM.29 Sixty-three percent of patients achieved sCR/CR/or near-CR (nCR) and a further 26% very good partial response status. Among nCR/sCR patients assessed by 8-color CMF, all tested negative for MRD. These early results of CRd appear to be superior to what has been achieved with other novel drug combinations in terms of (s)CR rates. The Mayo Clinic group also studied, in a retrospective analysis, the outcome of 290 patients with untreated MM who received immunomodulatory drug-based initial therapy, thalidomide-dexamethasone, or lenalidomide-dexamethasone, followed by either frontline/early (HDT performed within 12 months of diagnosis) or delayed (HDT >12 months after diagnosis) ASCT.30 Their retrospective results do not favor early ASCT, because the 4-year OS rate from diagnosis was identical, 73%, in both groups and there was no difference in terms of time to progression between the early and delayed SCT groups. Similar data and survival outcomes comparing early versus late ASCT have been published by Dunevin et al in a retrospective analysis involving 167 patients treated with thalidomide-, lenalidomide-, or bortezomib-based induction therapy at Ohio State University.31 Based on these results, many investigators have begun to consider the use of such novel agent-based therapies without the upfront application of ASCT as an alternative to early transplantation and the role of ASCT itself has become a matter of debate: should it be used upfront or as a salvage treatment at the time of progression for patients initially treated with novel agents? More drastically, some physicians are even floating the idea of the death of ASCT based on the results of the CRd regimen without intensive therapy despite the studies not being randomized.
Preliminary randomized data favor early ASCT plus novel agents over novel agents alone
At the end of 2014, only few data from prospective and retrospective trials are available to solve the outstanding issue of early versus late ASCT. At the 2010 ASH annual meeting, Siegel et al reported important results of the outcome of len/dex followed by early ASCT in the ECOG E4A03 study.32 In this trial, patients with newly diagnosed MM were randomized to lenalidomide with high-dose dexamethasone (LD) or lenalidomide with low-dose dexamethasone (Ld). Upon completing 4 cycles of therapy, patients had the option of proceeding to ASCT or continuing on the assigned therapy. In this post hoc, retrospective analysis of patients younger than 65 years and including only those surviving the first 4 cycles of therapy, OS at 3 years was 94% with early ASCT and 78% in patients continuing protocol therapy. Although a direct comparison between patients undergoing early ASCT and those who did not was not possible because the assignment to early ASCT versus no early ASCT was not randomized, the survival with ASCT at 3 years appeared to be higher. The investigators concluded that the strategy of lenalidomide plus dexamethasone induction followed by early ASCT had a remarkably good outcome in terms of OS and supported the continued role of early consolidative ASCT in newly diagnosed patients. Gay et al reported in abstract form at the 2013 ASH annual meeting the results of the first prospective randomized study comparing CCT plus novel agents with tandem high-dose melphalan and ASCT in newly diagnosed MM patients.33 A total of 402 patients received 4 cycles of len/dex as induction and were then randomized to MPR (melphalan, prednisone, lenalidomide) or tandem ASCT. After a median follow-up of 48 months, the median PFS was 24.2 months in the MPR arm and 38.8 months in the tandem ASCT arm (P < .0001), while the 5-year OS rate was 62% in the MPR arm versus 71% in the early intensive therapy arm (P = .27). Although preliminary, these results favor the early and systematic use of frontline HDT. At ASH 2013, the same Italian group also reported the preliminary results of a prospective randomized trial of lenalidomide-dexamethasone induction therapy (4 courses) followed by either CyRD (cyclophosphamide, lenalidomide, dexamethasone; 6 courses) or tandem ASCT in 389 patients with de novo symptomatic MM.34 At a short median follow-up of 3 years, PFS results strongly favor the intensive arm of the trial (median 27 months in the CyRD arm vs not reached, P = .01), without any OS difference yet (3-year OS 81% in the CyRD arm vs 84 in the ASCT arm, P = .89). Nevertheless, these 2 Italian trials have to be analyzed cautiously. In both of them, induction therapy was based on a combination of lenalidomide and dexamethasone, which is suboptimal compared with triplet bortezomib-based therapy, which is currently considered the most effective regimen before ASCT.6,11,12 Moreover, after initial treatment, patients underwent a second randomization step to receive lenalidomide maintenance or not, and 4 groups of ∼100 patients only will finally be compared: CCT ± lenalidomide, and HDT ± maintenance. This design could compromise the message of the optimal strategy in this population of patients. Two other ongoing trials, one conducted by the European Myeloma Network (EMN02 study; www.ClinicalTrials.gov identifier #NCT01208766) and one by the IFM plus a U.S. consortium (IFM/DFCI 2009 study; www.ClinicalTrials.gov identifier #NCT01208662) are investigating the same question and have already enrolled 1500 and 1000 patients, respectively. Although variability in consolidation and maintenance may affect PFS when comparing early ASCT versus late approaches, these 2 studies will solve many issues regarding the role of systematic frontline ASCT in the treatment of young patients eligible for HDT; however, results are not expected before the end of 2015.
In the future, biology might help in the treatment decision
Our understanding of the biology of MM has increased markedly over the last years. Systematic cytogenetic evaluations in clinical trials have revealed critical adverse prognostic factors, including 17p deletion, as being one of the most important,35 whereas the application of genomics has enabled the segregation of patients into risk groups according to different gene signatures.36,37 Although we are progressing toward a consensus regarding the definition of high-risk disease,35,38 few cooperative groups are currently able to propose a risk-adapted strategy incorporating frontline ASCT based on well-defined initial biological and/or clinical characteristics. This is particularly true outside of clinical trials, when patients are treated on a routine basis in the “real-life” setting. Additional correlative studies including genomic and cytogenetic analyses are being performed in the 2 ongoing prospective EMN2 and IFM/DFCI 2009 trials comparing upfront versus delayed ASCT mentioned, with the specific goal of defining subgroups of patients who may benefit from the different therapeutic approaches to develop a valuable risk-adapted strategy. In the United States, 2 groups are currently applying risk-adapted therapy. The Little Rock group in Arkansas proposes the application of different therapeutic options depending on the results obtained with gene-expression profiling.36 This strategy relies on their very extensive and impressive single-center experience. However, treatments are not randomized. The second group, at the Mayo Clinic in Rochester, Minnesota, is proposing the mSMART (Mayo Stratification for Myeloma and Risk-adapted Therapy) algorithm, a single-center consensus opinion taking into account genetically defined risk status, including cytogenetics, gene-expression profiling, and plasma-cell-labeling index.39 This classification allows for the definition of 3 risk groups, high, intermediate, and standard, which determine the treatment approaches. The high- and intermediate-risk groups are routinely offered ASCT, whereas in the standard-risk group, the collection of stem cells after 4 cycles of induction is proposed, but ASCT is not performed in patients harboring trisomies only. In following these approaches, the 2 groups are proposing what they consider as the best possible options to patients, but this will not solve the issue of early versus late ASCT. Their idea of implementing a tailored approach for all patients based on individual risk factors is strongly supported by the whole myeloma community. Nevertheless, at the current time, such a tailored approach based on the results of large phase 3 studies and aimed at adapting strategies to initial clinical and biological feature, as well as taking into account the “dynamic” prognostic factor that is the response to initial therapy,6 is not available.
ASCT in real life
Unlike the case with acute leukemia, in 2014, we have not yet reached the point of a risk-adapted strategy in MM. Moreover, the conclusions of the 2 most important prospective clinical trials aimed at comparing frontline versus late ASCT in the context of novel-agent-based therapy, the EMN2 and IFM/DFCI 2009 trials, are not yet available. Therefore, the optimal approach to the treatment of MM is still to propose the most effective treatment for all patients, regardless of risk status and including the so-called ”good risk” patients, and that this most effective treatment should involve the use of ASCT. This procedure is safe and is associated with a mortality rate of less than 2%, which is lower than that reported by physicians favoring continuous upfront therapy without ASCT, based for example on the lenalidomide-dexamethasone combination. Similarly, the argument of cost does not support the use of continuous novel agent-based therapy upfront in comparison to early ASCT, which is less expensive than 2 years of therapy including for example lenalidomide and carfilzomib. It was recently suggested that early ASCT could potentially be a relatively cost-effective treatment option compared with a delayed approach.40 Recent numbers from both the EBMT41 and Center for International Blood and Marrow Transplant Research (CIBMTR)42 registries clearly indicate that MM remains by far the principal indication for ASCT in the United States and Europe and that an increasing number of intensive therapy is performed year after year (almost 7000 ASCT sfor MM in the United States and 8500 in Europe in 2011), illustrating the profound importance of the technique for the treatment of young patients.
Disclosures
Conflict-of-interest disclosures: P.M. has received honoraria from Celgene, Millenium, and Janssen. M.A. is on the board of directors or an advisory committee and has consulted for Celgene and Janssen. Off-label drug use: Induction with novel agents for the treatment of frontline multiple myeloma.
Correspondence
Philippe Moreau, MD, Department of Hematology, University Hospital Hôtel-Dieu, Place Ricordeau, 44093 Nantes, France; Phone: +33-240-083271; Fax: +33-240-083250; e-mail: philippe.moreau@chu-nantes.fr.