In this issue of Blood Advances, Chirande et al describe an international partnership designed to build capacity and improve the care of children with hematologic disorders in sub-Saharan Africa through education and training.1 The article highlights the East African Pediatric Hematology-Oncology Program, developed in 2016 as a partnership between the Texas Children’s Global Hematology-Oncology-Pediatric-Excellence program in the United States and Makerere University and Mulago National Referral Hospital in Kampala, Uganda.2 The 2-year fellowship includes training and assessment of competency in evidence-based care, clinical and procedural skills, communication and professionalism, leadership, advocacy, and research. The program has trained 24 fellows from 7 African countries, who are now practicing as pediatric hematology/oncology subspecialists in Kenya, Tanzania, Malawi, Botswana, and South Sudan. Importantly, 87% of trainees have returned to their home countries to practice. The program also included the development of a specialized nursing program and training of primary health care workers to further support the development of clinical programs.
Global disparities in pediatric hematology are vast and unacceptable. Over the past several decades, there have been tremendous advances that have led to improvements in both survival and quality of life for children with hematologic malignancies and nonmalignant conditions such as sickle cell disease (SCD). Unfortunately, the geographic location of where a child lives when diagnosed is literally a matter of life and death. In the United States and Europe, the prognosis for most malignant and nonmalignant hematologic ailments in children is excellent due to access to early diagnosis and comprehensive care from well-trained hematology subspecialists. In sub-Saharan Africa, most children born with SCD or diagnosed with hematologic malignancies are likely to die, often before a diagnosis can be made and without access to highly effective disease-modifying therapies.
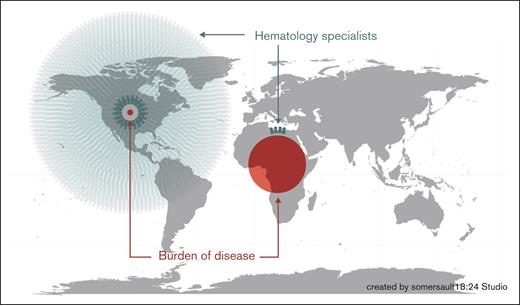
In the United States, there are 5500 children and adolescents diagnosed with hematologic malignancies and 2000 infants diagnosed with SCD by newborn screening per year, with >90% chance of survival to adulthood for both groups.3,4 According to the American Society of Pediatric Hematology/Oncology, there are ∼3000 board-certified and practicing pediatric hematology/oncology subspecialists and 78 active training programs that enroll ∼175 new fellows per year.3 In sub-Saharan Africa, >400 000 infants are born with SCD per year, most of whom die in the first years of life due to lack of newborn screening and associated treatment.5 Although data for hematologic malignancies are not available, the overall incidence is likely similar. In the United States, there are ∼73 million children aged <18 years and >500 million in sub-Saharan Africa. This suggests that there are likely 37 000 children and adolescents who could be diagnosed with hematologic malignancies in sub-Saharan Africa per year. Compared with the robust pediatric hematology workforce in the United States, the number of subspecialty-trained pediatric hematologists in sub-Saharan Africa can be counted on one hand in most countries and is drastically out of proportion to the burden of disease (see figure). Historically, this has resulted in African physicians seeking hematology training in other countries, with many not returning to their home countries to practice. This “brain drain” is not reflective of a lack of commitment to the home countries but rather due to lack of opportunities and infrastructure to function as a subspecialist in most African settings. There is a critical and desperate need to establish sustainable pediatric hematology training programs in sub-Saharan Africa.
Geospatial map of the burden of disease and number of hematology specialists. This figure depicts the geographical disparities of hematologic conditions vs hematology specialists in the United States compared with sub-Saharan Africa, highlighting the need for many more trained subspecialists to provide care for the greater burden of hematology disease among children in Africa.
Geospatial map of the burden of disease and number of hematology specialists. This figure depicts the geographical disparities of hematologic conditions vs hematology specialists in the United States compared with sub-Saharan Africa, highlighting the need for many more trained subspecialists to provide care for the greater burden of hematology disease among children in Africa.
The fellowship described by Chirande and colleagues in this issue of Blood Advances is an important step to build capacity for pediatric hematology care in sub-Saharan Africa, but there are a number of important challenges and potential barriers to expansion and sustainability. The majority of programs are entirely dependent on external funding, with estimated costs of as much as $20 000 per trainee.6 To build, expand, and retain subspecialists in African countries where there is such an overwhelming burden of disease, there must be buy-in and true investment from national governments, Ministries of Health, and academic institutions to develop and maintain these programs without reliance upon external funding, which can be tenuous and lead to immediate collapse of established programs. Additionally, it is essential to link these subspecialty training programs to build capacity for health care professionals of all disciplines to provide comprehensive care for children and adolescents with hematologic conditions.
We suggest taking a step back and reimagining hematology training in the context of sub-Saharan Africa. Although trained subspecialists in Africa likely provide care for both malignant and nonmalignant conditions, it is likely that the pull toward doing more oncology than hematology is strong given the high degree of specialization that is needed to diagnose malignancies and to administer chemotherapy. Given the overwhelmingly high burden of SCD alone, we suggest the consideration of a model in which hematology and oncology trainings are separated, as they are in many US adult training programs. In this way, committed trainees could pursue hematology or oncology alone, removing barriers of extended training and additional costs, which may prevent some from specializing at all. In fact, in adult hematology, this is already being implemented: the first adult hematology fellowship in East Africa was launched in 2023 at Aga Khan University in Kenya.7 Another consideration is to remove the distinction between pediatric and adult training programs. As capacity to provide pediatric hematology care improves, particularly for children with SCD, survival to adulthood will improve, creating a significant gap in providers trained to provide hematology care for surviving adults. This is a lesson we have learned the hard way in the United States and only now are ideating nonmalignant hematology training to consider a life span approach. As new training programs are developed, we suggest the consideration of life span training approaches that are not age specific. This “outside the box” thinking to create focused and streamlined training specifically in pediatric oncology or pediatric and adult hematology may result in a more robust workforce and improved outcomes across the life span. We applaud this important work and look forward to seeing the graduates of these newly developed training programs, including coauthors Lulu Chirande and Ruth Namazzi, to become leaders in the field to improve outcomes for children with hematologic conditions across sub-Saharan Africa.
Conflict-of-interest disclosure: The authors declare no competing financial interests.