TO THE EDITOR:
Approximately 100 000 adults in the United States are affected by sickle cell disease (SCD).1 Individuals with SCD seek acute care services for vaso-occlusive pain episodes (VOEs). Emergency department (ED) treatment of VOEs can be expensive, inefficient, and frustrating.2 Infusion center (IC)-based management of acute SCD pain has proven to be more timely and is associated with higher provider and patent satisfaction than ED care.2-4 IC-based care has resulted in shortened time to first dose of parenteral analgesia, a key metric for high-quality SCD care per national guidelines,5,6 along with decreased ED use and decreased system-wide healthcare costs.7-10 Standalone IC programs have emerged as a solution but require resources and personnel, which were unavailable at our institution. We sought to offer acute pain management services for VOEs in the outpatient setting and hypothesized that a telemedicine-guided same-day IC model would lead to lower ED use on a population level.
Our SCD clinic is embedded within cancer care services. The clinic comprises of a hematologist, an advanced practice provider (APP), a registered nurse/case manager, and a social worker. The clinic establishes ED and home pain plans for each patient; initiates disease-modifying therapy; and offers outpatient pain management, pain psychiatry, and social work referral, when appropriate. We are part of an academic hospital and care for ∼150 adults. All staff also care for patients with other hematologic diseases. Our hospitals are located on 2 campuses, and we have 4 IC locations.
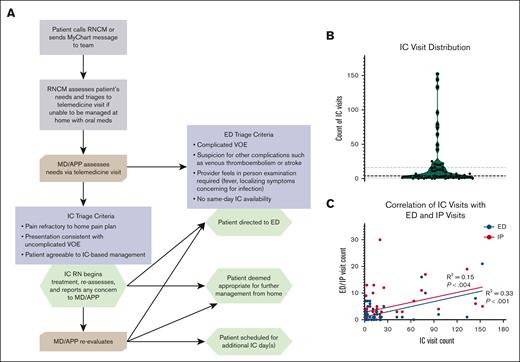
Our SCD IC workflow is summarized in Figure 1A. Patients were educated to contact the SCD team via phone call or secure message via our electronic medical record (EMR). This triggered a triage phone call by the registered nurse/case manager. A same-day telemedicine appointment was created with the hematologist or APP, who placed orders for day infusion as part of an IC treatment plan. Existing IC staff and the SCD team were pooled, and a real-time messaging thread was created once the patient was recommended for IC-based management. Clinic and IC staff coordinated same-day IC appointments. Registered nurses executed the treatment plan and communicated with the SCD team.
IC workflow, visit distribution, and correlation with ED and IP utilization. (A) Workflow outlining pathway from initial contact from patient to IC, ED, or home-based VOE management. Triage criteria for ED and IC are outlined. RNCM arranged telemedicine visit if the patient was unable to manage pain at home. (B) A violin plot depicting the distribution of IC visits over the study period. Dashed lines represent median and quartiles. (C) Linear regression demonstrates a direct correlation of IC visits with ED discharges and IP admissions per patient. MD/APP, hematologist or advanced practice provider; RNCM, registered nurse/case manager.
IC workflow, visit distribution, and correlation with ED and IP utilization. (A) Workflow outlining pathway from initial contact from patient to IC, ED, or home-based VOE management. Triage criteria for ED and IC are outlined. RNCM arranged telemedicine visit if the patient was unable to manage pain at home. (B) A violin plot depicting the distribution of IC visits over the study period. Dashed lines represent median and quartiles. (C) Linear regression demonstrates a direct correlation of IC visits with ED discharges and IP admissions per patient. MD/APP, hematologist or advanced practice provider; RNCM, registered nurse/case manager.
Retrospective data collection and review was approved by University of California San Diego human research protection program (institutional review board: #210705). Epic EMR was used to generate visit lists by type. Any patient with a visit within our health system at these locations during the study period (2017, 2018, 2021, and 2022) with an International Classification of Diseases 10 code specific for SCD (excluding trait) was included. Diagnosis of SCD was confirmed by chart review and patients without SCD and visits unrelated to acute VOE were removed. IC visits without pain medications administered were removed. For patients with IC visits, manual chart review was performed for age, sex, genotype, and disease modifying therapies. The IC model was implemented at our institution mid-year in 2019 and the COVID-19 pandemic in 2020 affected IC staffing and in-person availability. For this reason, we compared the 2-year periods from 2017 to 2018 (before IC) and 2021 to 2022 (after IC). There was no option for direct admission at our hospital; all ED visits resulted in ED discharge or inpatient (IP) admission. For IP admissions, we collected 30-day readmission counts. Pre-IC and post-IC means were analyzed using 1-tailed Welch t testing. Time to first dose of parenteral opioid pain medication (TFD) in our IC and ED was collected; median times were compared via Mann-Whitney U test.
Implementation of the IC program was successful and there were 1110 IC visits in the 2-year postimplementation period among 51 IC users, corresponding to 10.5 IC visits per patient per year. There were 129 patients in the pre-IC period and 134 patients in the post-IC period who had a visit of any type (ED, IP, or IC). Among patients with any visit type, mean ED discharges per patient per year decreased from 1.4 to 1.0 (P = .031) and mean IP admissions per patient per year remained the same at 1.1 (P = .49). Total ED visits were 372 in the pre- and 241 in the post-IC periods. Visit data per year for each type are shown in supplemental Table 1. Mean 30-day IP readmissions per patient with IP admissions per year decreased from 0.48 to 0.39 (P = .66). Thirty IC visits resulted in presentation to the ED within 6 hours; 28 resulted in IP admission, and 2 resulted in ED discharge. Using this metric, admission rate from the IC was 2.8%, and the ED admission rate was 52% in the post-IC period. Demographic characteristics are displayed in Table 1, and utilization patterns of IC users are shown in Figure 1B. Among 51 patients who used the IC, 8 patients exclusively used the IC and had no ED visits. The median IC visit count was 4 (interquartile range [IQR], 1-16). Eighty-two percent of patients had ≤25 IC visits in the post-IC period, and the remaining 9 patients had visit counts ranging from 42 to 153. There was a positive correlation between IC visits and ED/IP usage (Figure 1C). There were no complications or safety issues noted at the IC in the post-IC period. During the post-IC period, the median TFD was shorter across our ICs at 26.2 minutes (IQR, 18.7-39.0), than 82.8 minutes (IQR, 44.6-151.5) in the ED (P < .0001).
Demographics, genotypes, and disease modifying therapy for IC user population
| IC population characteristics . | IC users, n = 51 . |
|---|---|
| Age, median (range), y | 37 (20-64) |
| Sex, count (%) | |
| Female | 34 (67) |
| Male | 17 (33) |
| Genotype, count (%) | |
| SS | 32 (61) |
| SC | 12 (24) |
| Sβ0 thalassemia | 2 (4) |
| Sβ+ thalassemia | 5 (10) |
| Disease modifying therapy, count (%) | |
| Hydroxyurea | 31 (61) |
| Red cell exchange | 18 (35) |
| IC population characteristics . | IC users, n = 51 . |
|---|---|
| Age, median (range), y | 37 (20-64) |
| Sex, count (%) | |
| Female | 34 (67) |
| Male | 17 (33) |
| Genotype, count (%) | |
| SS | 32 (61) |
| SC | 12 (24) |
| Sβ0 thalassemia | 2 (4) |
| Sβ+ thalassemia | 5 (10) |
| Disease modifying therapy, count (%) | |
| Hydroxyurea | 31 (61) |
| Red cell exchange | 18 (35) |
SC, sickle cell-hemoglobin C disease; SS, sickle cell-hemoglobin S disease.
We successfully established and implemented a same-day infusion program for patients with SCD using a telemedicine platform and available IC resources. The use of telemedicine and existing EMR tools facilitated triage and communication between team members. Median TFD in our IC was 26.2 minutes, well within the established guideline of 60 minutes5 and faster than what was available in our ED. We observed a decrease in overall ED visits after implementation. There was a population of IC users who also had high ED and IP visits, possibly because of a high burden of chronic pain that was unmet by comprehensive outpatient resources.11 This model may be particularly useful for small- to mid-sized SCD programs and those using the embedded clinic model for care delivery.
Limitations of our study include small sample size and retrospective nature of analysis. Pre- and post-IC data sets included different individuals, and some of the differences in ED use may be explained by differences in usage patterns between individuals. There was a small group of patients who spent most of the study period admitted to the hospital. However, we believe that this was not different between the pre- and post-IC periods. We did not have a reliable way to capture visits at outside hospitals. However, upon review of the EMR, which has the capacity to capture visits at some other local institutions, and there being no other SCD centers in our county, we believe these numbers are small. We did not observe a significant decrease in IP admissions or readmissions, possibly because patients who required admission for VOE required more complex pain control regimens or had complicated VOEs. Future work will examine cost savings under this model and describe quality improvement centered around caring for severe VOEs within the IC.
In summary, we developed a telemedicine-guided same-day IC model for management of acute SCD VOE. The implementation of this program led to decreased ED use. This model may be replicated by SCD centers without dedicated IC services.
Acknowledgments: Grant support was received from the Health Resources and Service Administration (award number 2 U1EMC27862-08-00) and the National Institutes of Health (NIH), National Center for Advancing Translational Sciences (award number UL1 TR001442).
The content of this article is solely the responsibility of the authors and does not necessarily represent the official views of the NIH.
Contribution: J.B. contributed to conceptualization, data collection, and writing; A.Y. contributed to data collection and writing; J.G., S.S., and S.B. contributed to conceptualization and writing; and S.G. contributed to conceptualization, design and implementation of the infusion center model, data collection, and writing.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Srila Gopal, University of California San Diego, 3855 Health Sciences Dr, La Jolla, CA 92037; email: srgopal@health.ucsd.edu.
References
Author notes
Presented in abstract form at the 65th annual meeting of the American Society of Hematology, San Diego, CA, 9 December 2023.
Original data are available on request from the corresponding author, Srila Gopal (srgopal@health.ucsd.edu).
The full-text version of this article contains a data supplement.