Key Points
Addition of nivolumab to R-CHOP, using a priming approach, offers improved outcomes without unexpected toxicities even in high-risk disease.
Evaluation of immune cell subsets offers insights into the mechanisms of efficacy and toxicity with the combination regimen.
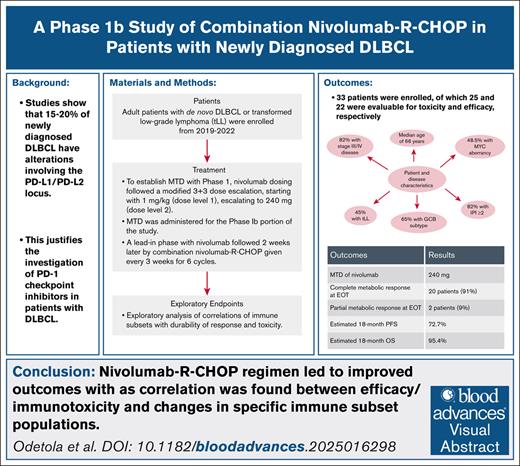
Visual Abstract
Approximately 20% of diffuse large B-cell lymphoma have aberrations involving the programmed death ligands 1 and 2 (PD-L1/PD-L2) locus. This justifies the investigation of PD-1 checkpoint inhibitors in the frontline therapy setting in a bid to improve outcomes, especially in patients with high-risk disease (antecedent low-grade lymphoma, MYC aberrancy, advanced staged disease, and intermediate/high-risk International Prognostic Index score). This phase 1b study evaluated the safety and preliminary efficacy of a combination of nivolumab and R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone) using a priming approach. Upon establishing the maximum tolerated dose of nivolumab, treatment consisted of a lead-in phase with nivolumab 240 mg × 1 followed 2 weeks later by combination nivolumab–R-CHOP given every 3 weeks for 6 cycles. A total of 33 patients were enrolled, of which 25 and 22 patients were evaluable for toxicity and efficacy, respectively. Estimated 18-month overall survival and progression-free survival rates were 95.4% and 72.7%, respectively. The observed therapy-related adverse events were not significantly different from previous reports on nivolumab and R-CHOP, respectively. Patient-reported outcomes did not suggest that the addition of nivolumab to R-CHOP led to worse quality of life measures. Exploratory analysis of biologic correlates showed an exhausted T-cell immunophenotype to be a predictor of progression and immunotoxicity, while also suggesting the effectiveness of a priming approach. This trial was registered at www.clinicaltrials.gov as #NCT03704714.
Introduction
Diffuse large B-cell lymphoma (DLBCL) is the most common subtype of non-Hodgkin lymphoma (NHL), accounting for about one-third of all NHL cases in the United States.1,2 At present, chemoimmunotherapy with R-CHOP (rituximab, cyclophosphamide, doxorubicin, vincristine, and prednisone), administered in 4 to 6 cycles, is an established standard of care for DLBCL.3 However, this regimen is not curative in all patients, with only ∼60% to 70% achieving durable remission; ∼20% experiencing primary disease refractoriness, and 30% suffer a relapse.4 Therefore, there have been several efforts to improve upon R-CHOP (the so-called R-CHOP + X approach), with no generalizable results.5-8 This is likely due to the heterogeneity of the disease.9-11
There has been growing recognition that a proportion (20%-30%) of DLBCL will have aberrations involving the programmed death ligands 1 and 2 (PD-L1/PD-L2) locus, with consequent T-cell exhaustion, and evasion of the immune system by cancer cells.12-14 Increased expression of PD-L1/PD-L2 in a subset of DLBCL is characterized by the finding of recurrent copy number alterations at the chromosome 9p24.1 locus.15,16 This is more commonly associated with the activated B-cell (nongerminal center) subtype, typically associated with poorer survival with R-CHOP, in addition to other high-risk features, such as increased serum lactate dehydrogenase (LDH), and International Prognostic Index (IPI) that correlates with higher risk.17-19 However, these PD-L1/PD-L2 alterations have been associated with a T-cell–inflamed phenotype, and have been shown to correlate with improved response to immune checkpoint inhibitors (ICIs) with potential for reversal of the T-cell exhaustion.19
The addition of ICIs to standard chemoimmunotherapy has been evaluated in patients with untreated DLBCL. The combination of atezolizumab, a PD-L1 inhibitor, with R-CHOP demonstrated a complete remission (CR) rate higher than historical control; additionally, the additive immunotoxicity did not hinder dose administration of R-CHOP.20 The use of immune priming with an ICI prior to administering R-CHOP has also been considered, given the evidence for increased efficacy of chemotherapy in patients with NHL with prior exposure to immunotherapy.21 Priming with immunotherapy prior to chemotherapy was first described in solid tumors, and subsequently demonstrated in NHL.22-24
We investigated the frontline use of combination nivolumab and R-CHOP based on a significant proportion of untreated cases of DLBCL expected to have PD-L1/PD-L2 aberrations, and the suggestion of synergism between immunotherapy and chemotherapy. Additionally, we deployed the principle of immune priming (treatment with nivolumab weeks before initiation of the combination regimen), and evaluated biologic correlates of efficacy and toxicity with this approach.
This phase 1b study was conducted to determine the maximum tolerated dose (MTD) for nivolumab in combination with R-CHOP in patients with DLBCL, and to evaluate the preliminary efficacy of the combined regimen.
Materials and methods
Study participants
The phase 1b nonrandomized study (ClinicalTrials.gov identifier #NCT03704714) was conducted at 2 academic medical centers and their community affiliates in the United States from 2019 to 2022.
Of note, the unforeseen COVID-19 pandemic significantly affected patient enrollment, leading to a prolonged study period. Patients aged ≥18 years with previously untreated de novo DLBCL or large cell transformation of a low-grade lymphoma were eligible for the study following histologic confirmation of their diagnosis, and identification of at least 1 measurable lesion on positron emission tomography-computed tomography scan.25 Patients with prior exposure to PD-1/PD-L1 inhibitors, known autoimmune disease, concurrent use of immunomodulatory agents, or solid organ transplant were excluded from the study.
Study design and treatment
To establish the MTD with phase 1, nivolumab dosing followed a modified 3+3 dose escalation, with a starting dose of 1 mg/kg (dose level 1), escalating to 240 mg (dose level 2). A dose-limiting toxicity was defined by the occurrence of prespecified toxicities with the first 2 cycles of combination therapy deemed as a possibly, probably, or definitely related to both nivolumab and R-CHOP. This included grade ≥3 nonhematologic and hematologic toxicities (including one that caused a delay of >14 days in initiating cycle 2 or 3).
The MTD, once established, was administered for the phase 1b portion of the study. Treatment consisted of a lead-in dose of nivolumab followed 2 weeks later by combination therapy with nivolumab and R-CHOP. Nivolumab–R-CHOP was then given on day 1 of each 3-week cycle for a total of 6 cycles. For combination therapy, nivolumab was administered on day 1 followed by R-CHOP on days 1 to 5 (days 2-6 for cycle 1, and days 1-5 for subsequent cycles). R-CHOP comprised IV rituximab 375 mg/m2, cyclophosphamide 750 mg/m2, doxorubicin 50 mg/m2, and vincristine 1.4 mg/m2 (capped at 2 mg) on day 1, and prednisone 100 mg orally (or equivalent), once daily, on days 1 to 5. Patients were allowed palliative steroids for symptom management prior to study treatment, with a 7-day washout prior to dosing lead-in nivolumab. Patients previously treated for their indolent lymphoma were eligible if they had not received prior anthracycline.
Disease staging and burden assessment was conducted using positron emission tomography-computed tomography scan prior to initiation of therapy. Response assessments were conducted using the Lugano Criteria for Assessment of Lymphoma at mid-treatment (after cycle 3), and end-of-treatment (after cycle 6) time points. For patients who achieved CR, surveillance with periodic history and physical exam was conducted every 3 months for ≤18 months from the start of treatment, until recurrent lymphoma or death. Imaging during the follow-up period was performed at 12 and 18 months from the start of study treatment.
Adverse effects were assessed using the Common Terminology Criteria for Adverse Events (CTCAE) version 5. Immunotoxicity with nivolumab was evaluated and managed using the National Comprehensive Cancer Network’s guidelines.
Primary prophylaxis against neutropenic fever with the aid of granulocyte colony-stimulating factor, including its pegylated formulation, was administered per physician discretion/institutional guidelines. Secondary prophylaxis with granulocyte colony-stimulating factor was deployed in patients who had neutropenic fever with no primary prophylaxis.
For biologic correlative studies, peripheral blood samples were collected at 4 time points: prior to lead-in visit (LIV) predose, C1D1 predose, end of treatment, and at relapse. These samples were analyzed for immune cell subsets using a high-dimensional spectral flow cytometry (CyTEK) panel that incorporated hallmark surface markers for all major immune populations and serum cytokines/chemokines. We also performed analysis for PD-1/PDL-1 expression by immunohistochemistry (IHC). The IHC for PD-1 and PD-L1 was done on tissue biopsy samples, with efforts to score staining and intensity in neoplastic B cells. Positive staining for PD-1 and PD-L1 was defined as clear membranous staining.
Study objectives
The primary objective of this study was to determine the MTD for the combination treatment of nivolumab and R-CHOP in patients with DLBCL for the phase 1 portion. The primary objective of the phase 1b portion was to assess the impact of the combination therapy on CR rates.
Secondary objectives were to determine safety, with a particular focus on immunotoxicity. Adverse effects were assessed using the CTCAE version 5. We also assessed the impact of the regimen on the quality of life using patient-reported outcomes–CTCAE (PRO-CTCAE). Geriatric Prognostic Index (GPI) for assessment of frailty was performed in all patients, irrespective of age, to look for changes associated with treatment and disease course. This assessment tool was administered to patients at the LIV, C1D1, end of treatment, and progression. Adverse events were assessed from the time of informed consent until 42 days (± 4 weeks) after treatment discontinuation. The PRO-CTCAE data were collected on C1D1 and C6D1. We assessed the impact of the combination therapy on overall response rate (ORR) and survival outcomes, including progression-free survival (PFS), overall survival (OS), and event-free-survival.
For exploratory objectives, changes in immune cell subsets and the cytokine/chemokine milieu associated with treatment with nivolumab were evaluated as predictive biomarkers of response and toxicity.
Statistical design
This was a phase 1b dose escalation with a dose expansion cohort design. Dose escalation was completed and recommended phase II dose was determined. Sample size for the dose expansion cohort was based on estimation of CR rate among patients treated at the MTD/recommended phase II dose. Assuming the true CR rate of 80%, a sample size of n = 22 evaluable patients would provide a 1-sided exact Clopper-Pearson 95% confidence interval with a lower limit of 61.0%, which excludes the unacceptably low (as previously determined) 60% CR rate. Patients treated at the MTD during dose escalation and dose expansion phases were included in the analysis for CR.
Primary objectives were reported descriptively in tabular format for both objectives. Kaplan-Meier curves were generated for PFS and OS as secondary end points.
Descriptive statistics were summarized for GPI scores, the Functional Assessment of Anorexia/Cachexia Therapy (FAACT) scores, and the symptomatic toxicities assessed by the National Cancer Institute PRO-CTCAE.
Exploratory analyses for changes in immune cell subsets were conducted using edgeR analysis and a 2-tailed t-test with multiple-comparison correction using the Benjamini-Hochberg adjustment. To correlate changes in these markers with either PFS, OS, or event-free-survival, proportional hazards regression with time-dependent covariates (serum markers) were used. Fisher’s exact test was used to test significant correlations of serum markers with CR rate. Descriptive statistics were generated for response rates.
The study was approved by the institutional review boards at the participating sites, and conformed to the principles of the Declaration of Helsinki and the International Council for Harmonization Good Clinical Practice guidelines. All patients enrolled in the study provided written informed consent prior to registration in the study.
Results
A total of 33 patients were enrolled in the study from 2019 to 2022. The majority of the patients were men (64%); 79% of the patients were White. Sixty-four percent of the patients were aged >60 years (Table 1). The predominant Eastern Cooperative Oncology Group performance status was 0 to 1 (91%). Most patients had stage III or IV disease (82%), with the IPI in the intermediate-to-risk category in 87% (35% had IPI 4-5). Cell-of-origin analysis revealed that 60.6% had GCB subtype. MYC aberrancy (10 with double-expressor disease, 6 with double-hit lymphoma, and 3 with triple-hit lymphoma) was documented in 39.4% of patients, while 45.5% of patients had transformed low-grade lymphoma. Among patients with transformed low-grade lymphoma, 2 had received therapy with regimens including rituximab, obinutuzumab, and lenalidomide prior to transformation. About one-third (34.5%) of the patients had an elevated LDH at diagnosis, with a median LDH of 208 mg/dL for the entire cohort (range, 146-731).
Patient and disease characteristics observed in the study
| Characteristic . | All patients . | Evaluable for toxicity . | Evaluable for efficacy . |
|---|---|---|---|
| N = 33 . | n = 25 . | n = 22 . | |
| Sex, n (%) | |||
| Female | 12 (36.4) | 8 (32) | 6 (27.3) |
| Male | 21 (63.6) | 17 (68) | 16 (72.7) |
| Age, n (%) | |||
| ≤60 y | 12 (36.4) | 7 (28) | 7 (31.8) |
| >60 y | 21 (63.6) | 18 (72) | 15 (68.2) |
| Race, n (%) | |||
| Asian | 2 (6.1) | 2 (8.0) | 2 (9.1) |
| Black | 1 (3.0) | 1 (4.0) | 1 (4.5) |
| White | 26 (79) | 19 (76) | 16 (73) |
| Unknown | 4 (12) | 3 (12) | 3 (14) |
| ECOG PS, n (%) | |||
| 0-1 | 30 (90.9) | 23 (92) | 21 (95.5) |
| ≥2 | 3 (9.1) | 2 (8.0) | 1 (4.5) |
| Stage, n (%) | |||
| I-II | 6 (18) | 6 (24) | 6 (27) |
| III-IV | 27 (82) | 19 (76) | 16 (73) |
| IPI, n (%) | |||
| 0-1 | 4 (12.1) | 4 (16) | 4 (18.2) |
| 2-3 | 16 (48.5) | 10 (40) | 10 (45.5) |
| 4-5 | 11 (33.3) | 10 (40) | 7 (31.8) |
| Unknown | 2 (6.1) | 1 (4) | 1 (4.5) |
| Disease subtype, n (%) | |||
| ABC | 11 (33.3) | 8 (32) | 7 (31.8) |
| GCB | 20 (60.6) | 16 (64) | 14 (63.6) |
| Unknown | 2 (6.1) | 1 (4) | 1 (4.5) |
| De novo DLBCL, n (%) | 18 (54.5) | 13 (52) | 11 (50) |
| Transformed LL, n (%) | 15 (45.5) | 12 (48) | 11 (50) |
| MYC aberrancy, n (%) | 13 (39.4) | 13 (52.0) | 13 (52.0) |
| DEL | 10 (30.3) | 10 (40.0) | 10 (40.0) |
| DHL | 6 (18.2) | 6 (24.0) | 6 (24.0) |
| THL | 3 (9.1) | 3 (12.0) | 3 (12.0) |
| Characteristic . | All patients . | Evaluable for toxicity . | Evaluable for efficacy . |
|---|---|---|---|
| N = 33 . | n = 25 . | n = 22 . | |
| Sex, n (%) | |||
| Female | 12 (36.4) | 8 (32) | 6 (27.3) |
| Male | 21 (63.6) | 17 (68) | 16 (72.7) |
| Age, n (%) | |||
| ≤60 y | 12 (36.4) | 7 (28) | 7 (31.8) |
| >60 y | 21 (63.6) | 18 (72) | 15 (68.2) |
| Race, n (%) | |||
| Asian | 2 (6.1) | 2 (8.0) | 2 (9.1) |
| Black | 1 (3.0) | 1 (4.0) | 1 (4.5) |
| White | 26 (79) | 19 (76) | 16 (73) |
| Unknown | 4 (12) | 3 (12) | 3 (14) |
| ECOG PS, n (%) | |||
| 0-1 | 30 (90.9) | 23 (92) | 21 (95.5) |
| ≥2 | 3 (9.1) | 2 (8.0) | 1 (4.5) |
| Stage, n (%) | |||
| I-II | 6 (18) | 6 (24) | 6 (27) |
| III-IV | 27 (82) | 19 (76) | 16 (73) |
| IPI, n (%) | |||
| 0-1 | 4 (12.1) | 4 (16) | 4 (18.2) |
| 2-3 | 16 (48.5) | 10 (40) | 10 (45.5) |
| 4-5 | 11 (33.3) | 10 (40) | 7 (31.8) |
| Unknown | 2 (6.1) | 1 (4) | 1 (4.5) |
| Disease subtype, n (%) | |||
| ABC | 11 (33.3) | 8 (32) | 7 (31.8) |
| GCB | 20 (60.6) | 16 (64) | 14 (63.6) |
| Unknown | 2 (6.1) | 1 (4) | 1 (4.5) |
| De novo DLBCL, n (%) | 18 (54.5) | 13 (52) | 11 (50) |
| Transformed LL, n (%) | 15 (45.5) | 12 (48) | 11 (50) |
| MYC aberrancy, n (%) | 13 (39.4) | 13 (52.0) | 13 (52.0) |
| DEL | 10 (30.3) | 10 (40.0) | 10 (40.0) |
| DHL | 6 (18.2) | 6 (24.0) | 6 (24.0) |
| THL | 3 (9.1) | 3 (12.0) | 3 (12.0) |
ABC, activated B cell; DEL, double-expressor lymphoma; DHL, double-hit lymphoma; ECOG PS, Eastern Cooperative Oncology Group Performance Status; GCB, germinal center B-cell; LL, low-grade lymphoma; THL, triple-hit lymphoma.
Efficacy
Of the 32 enrolled patients (7 in phase 1, and 25 in phase 1b), 3 did not start any therapy (hence not evaluable for efficacy or toxicity), 2 patients (1 patient transitioned to mini-R-CHOP alone for immediate control of disease, and the other developed infectious complications with treatment discontinued) did not complete the minimum 2 doses of nivolumab to meet study definition for evaluable, and were deemed ineligible for efficacy assessment but evaluable for toxicity, 1 patient was assigned to dose level 1 but was treated for dose level 2 (deemed evaluable for toxicity but not efficacy), 1 did not complete the dose-limiting toxicity (deemed ineligible for MTD assessment but evaluable for toxicity). There was no reported clinical disease progression prior to C1D1 of R-CHOP. However, patients were allowed prednisone after the initiation of lead-in nivolumab.
A total of 22 patients were evaluable for efficacy at the MTD. A dose of 240 mg of nivolumab was established as MTD. Twenty of 22 (91%) achieved complete metabolic response (CMR), and 2 achieved partial metabolic response by end of treatment, with ORR of 100% (2 of the 3 evaluable patients who received nivolumab at 1 mg/kg achieved a CMR). One patient died from COVID-19 after 4 cycles, but was in CMR on interim imaging. With a median follow-up of 11.6 months (range, 2.6-24.5), 4 patients had progression. Both patients with partial metabolic response by end of treatment have not relapsed. Estimated 18-month OS and PFS rates were 95.4% and 72.7%, respectively. The median PFS and OS were not reached (Figures 1 and 2). When the MYC aberrancy status was put into consideration, the 2 patients with partial response had double-hit lymphoma, while all 4 patients with progression had MYC aberrancy: all had double-expressor disease with 1 each having double-hit lymphoma and triple-hit lymphoma, respectively.
Kaplan-Meier plot of the PFS estimate. CI, confidence interval; N, number; NR, not reached.
Kaplan-Meier plot of the PFS estimate. CI, confidence interval; N, number; NR, not reached.
Kaplan-Meier plot of the OS estimate. CI, confidence interval; N, number; NR, not reached.
Kaplan-Meier plot of the OS estimate. CI, confidence interval; N, number; NR, not reached.
Analysis of the correlation between PFS and PD-1 and/or PDL-1 expression was undertaken (Table 2). Of the patients with PD-L1 positivity by IHC, 76.5% had percentage scores ≥10%, while 66.7% met this score threshold for PD-1 staining. The median PD-1 and PD-L1 percentage scores for the cohort were 8% and 15%, respectively. The majority of patients with PD-L1 positive tumors had a lower intensity score, while most of those with PD-1 positivity had higher intensity scores. However, there was no statistically significant differences in PFS based on PD-1 or PDL-1 status or intensity scores.
Results of analysis of PD-1 and PD-L1 expression by IHC
| Characteristic . | Overall N = 22∗ . | No progression n = 17 . | Progression n = 5 . | P value† . |
|---|---|---|---|---|
| PD-L1 percentage score | 15 (10-35) | 10 (10-20) | 35 (25-45) | .2 |
| Unknown | 7 | 6 | 1 | |
| PD-L1 intensity | >.9 | |||
| 1-2.0 | 9 (60) | 7 (64) | 2 (50) | |
| >2.0 to 3 | 6 (40) | 4 (36) | 2 (50) | |
| Unknown | 7 | 6 | 1 | |
| PD-1 percentage score | 8 (2-30) | 5 (1-30) | 20 (9-35) | .4 |
| Unknown | 6 | 5 | 1 | |
| PD-1 intensity | >.9 | |||
| 0-1.0 | 1 (7) | 1 (10) | 0 (0) | |
| >1.0 to 2 | 13 (93) | 9 (90) | 4 (100) | |
| Unknown | 8 | 7 | 1 |
| Characteristic . | Overall N = 22∗ . | No progression n = 17 . | Progression n = 5 . | P value† . |
|---|---|---|---|---|
| PD-L1 percentage score | 15 (10-35) | 10 (10-20) | 35 (25-45) | .2 |
| Unknown | 7 | 6 | 1 | |
| PD-L1 intensity | >.9 | |||
| 1-2.0 | 9 (60) | 7 (64) | 2 (50) | |
| >2.0 to 3 | 6 (40) | 4 (36) | 2 (50) | |
| Unknown | 7 | 6 | 1 | |
| PD-1 percentage score | 8 (2-30) | 5 (1-30) | 20 (9-35) | .4 |
| Unknown | 6 | 5 | 1 | |
| PD-1 intensity | >.9 | |||
| 0-1.0 | 1 (7) | 1 (10) | 0 (0) | |
| >1.0 to 2 | 13 (93) | 9 (90) | 4 (100) | |
| Unknown | 8 | 7 | 1 |
Median (interquartile range); n (%).
Wilcoxon rank-sum test; Fisher’s exact test.
Safety
A total of 25 patients was evaluable for toxicity as described above. All 25 patients had at least 1 therapy-related adverse event (TRAE). Grade ≥3 adverse events were seen in 88% of the patients, as presented in Table 3. The majority of the TRAEs were grades 1 to 2 (242/310, 78.1%). The most common nonhematologic TRAEs attributed to nivolumab–R-CHOP were fatigue in 22 patients (88%), hypertension in 21 patients (84%), and musculoskeletal disorders in 16 patients (64%). Sixteen (60%) patients had infections with a total of 25 events, 32% of which were grades 3 to 4. The most encountered infections were urinary tract infection (6 of 25, 24%) and respiratory tract infection (6 of 25, 24%). COVID-19 was diagnosed in 3 patients (12%), with 1 being the only grade 5 event in the study.
Adverse events, including IrAEs, observed in the study
| Events . | All grades (N = 25) . | Grade 3 . | Grade 4 . | Grade 5 . |
|---|---|---|---|---|
| Non-IrAEs (general toxicities), n (%) | ||||
| Hypertension | 21 (84) | 3 (12) | 1 (4) | 0 (0) |
| Cardiac arrhythmia | 13 (52) | 0 (0) | 0 (0) | 0 (0) |
| Hyperglycemia | 15 (60) | 2 (8) | 1 (4) | 0 (0) |
| Anemia | 22 (88) | 1 (4) | 0 (0) | 0 (0) |
| Leukopenia | 17 (68) | 13 (52) | 3 (12) | 0 (0) |
| Neutropenia | 18 (72) | 11 (46) | 4 (16) | 0 (0) |
| Lymphopenia | 21 (84) | 13 (52) | 4 (16) | 0 (0) |
| Thrombocytopenia | 16 (64) | 1 (4) | 0 (0) | 0 (0) |
| Febrile neutropenia | 3 (12) | 3 (12) | 0 (0) | 0 (0) |
| Infections | 15 (60) | 6 (24) | 0 (0) | 1 (4) |
| Fatigue | 22 (88) | 0 (0) | 0 (0) | 0 (0) |
| Mood disorder | 13 (52) | 2 (8) | 0 (0) | 0 (0) |
| Nausea/vomiting | 13 (52) | 0 (0) | 0 (0) | 0 (0) |
| Abdominal pain/acid reflux | 13 (52) | 0 (0) | 0 (0) | 0 (0) |
| Anorexia | 15 (60) | 0 (0) | 0 (0) | 0 (0) |
| Diarrhea | 12 (48) | 1 (4) | 0 (0) | 0 (0) |
| Constipation | 15 (60) | 0 (0) | 0 (0) | 0 (0) |
| MSK pain (arthralgia and myalgia) | 16 (64) | 0 (0) | 0 (0) | 0 (0) |
| Alopecia | 6 (24) | 0 (0) | 0 (0) | 0 (0) |
| Pleural/pericardial effusion | 4 (16) | 0 (0) | 0 (0) | 0 (0) |
| Acute kidney injury | 4 (16) | 1 (4) | 0 (0) | 0 (0) |
| Peripheral neuropathy | 14 (56) | 0 (0) | 0 (0) | 0 (0) |
| Immunotoxicity/IrAEs, n (%) | ||||
| Infusion reaction | 3 (12) | 0 (0) | 0 (0) | 0 (0) |
| Dermatitis | 4 (16) | 1 (4) | 0 (0) | 0 (0) |
| Conjunctivitis | 1 (4) | 0 (0) | 1 (4) | 0 (0) |
| Hypothyroidism | 3 (12) | 0 (0) | 0 (0) | 0 (0) |
| Hyperthyroidism | 1 (4) | 0 (0) | 0 (0) | 0 (0) |
| Hepatitis | 3 (12) | 1 (4) | 0 (0) | 0 (0) |
| Pneumonitis | 2 (8) | 0 (0) | 0 (0) | 0 (0) |
| Colitis | 1 (4) | 1 (4) | 0 (0) | 0 (0) |
| Myocarditis | 1 (4) | 0 (0) | 1 (4) | 0 (0) |
| Events . | All grades (N = 25) . | Grade 3 . | Grade 4 . | Grade 5 . |
|---|---|---|---|---|
| Non-IrAEs (general toxicities), n (%) | ||||
| Hypertension | 21 (84) | 3 (12) | 1 (4) | 0 (0) |
| Cardiac arrhythmia | 13 (52) | 0 (0) | 0 (0) | 0 (0) |
| Hyperglycemia | 15 (60) | 2 (8) | 1 (4) | 0 (0) |
| Anemia | 22 (88) | 1 (4) | 0 (0) | 0 (0) |
| Leukopenia | 17 (68) | 13 (52) | 3 (12) | 0 (0) |
| Neutropenia | 18 (72) | 11 (46) | 4 (16) | 0 (0) |
| Lymphopenia | 21 (84) | 13 (52) | 4 (16) | 0 (0) |
| Thrombocytopenia | 16 (64) | 1 (4) | 0 (0) | 0 (0) |
| Febrile neutropenia | 3 (12) | 3 (12) | 0 (0) | 0 (0) |
| Infections | 15 (60) | 6 (24) | 0 (0) | 1 (4) |
| Fatigue | 22 (88) | 0 (0) | 0 (0) | 0 (0) |
| Mood disorder | 13 (52) | 2 (8) | 0 (0) | 0 (0) |
| Nausea/vomiting | 13 (52) | 0 (0) | 0 (0) | 0 (0) |
| Abdominal pain/acid reflux | 13 (52) | 0 (0) | 0 (0) | 0 (0) |
| Anorexia | 15 (60) | 0 (0) | 0 (0) | 0 (0) |
| Diarrhea | 12 (48) | 1 (4) | 0 (0) | 0 (0) |
| Constipation | 15 (60) | 0 (0) | 0 (0) | 0 (0) |
| MSK pain (arthralgia and myalgia) | 16 (64) | 0 (0) | 0 (0) | 0 (0) |
| Alopecia | 6 (24) | 0 (0) | 0 (0) | 0 (0) |
| Pleural/pericardial effusion | 4 (16) | 0 (0) | 0 (0) | 0 (0) |
| Acute kidney injury | 4 (16) | 1 (4) | 0 (0) | 0 (0) |
| Peripheral neuropathy | 14 (56) | 0 (0) | 0 (0) | 0 (0) |
| Immunotoxicity/IrAEs, n (%) | ||||
| Infusion reaction | 3 (12) | 0 (0) | 0 (0) | 0 (0) |
| Dermatitis | 4 (16) | 1 (4) | 0 (0) | 0 (0) |
| Conjunctivitis | 1 (4) | 0 (0) | 1 (4) | 0 (0) |
| Hypothyroidism | 3 (12) | 0 (0) | 0 (0) | 0 (0) |
| Hyperthyroidism | 1 (4) | 0 (0) | 0 (0) | 0 (0) |
| Hepatitis | 3 (12) | 1 (4) | 0 (0) | 0 (0) |
| Pneumonitis | 2 (8) | 0 (0) | 0 (0) | 0 (0) |
| Colitis | 1 (4) | 1 (4) | 0 (0) | 0 (0) |
| Myocarditis | 1 (4) | 0 (0) | 1 (4) | 0 (0) |
MSK, musculoskeletal.
The observed hematologic TRAEs included anemia in 22 patients (88%), neutropenia in 18 patients (72%), and thrombocytopenia in 16 patients (64%), as summarized in Table 2. Neutropenic fever was reported in 4 patients (16%), with 75% being grades 3 to 4.
Immune-related adverse events (IrAEs) were the most common TRAEs specifically attributed to nivolumab, and occurred in 17 patients (68%). The most common IrAEs included thyroiditis (n = 4, 16%), dermatitis (n = 4, 16%), hepatitis (n = 3, 12%), and infusion reactions (n = 3, 12%). Most common high-grade IrAEs were: 1 case each of colitis (grade 3), hepatitis (grade 3), myocarditis (grade 4), conjunctivitis (grade 4), and dermatitis (grade 3). Treatment discontinuation due to IrAEs occurred in 2 patients (8%): 1 each for myocarditis and dermatitis. The timing of IrAE onset typically ranged from initial exposure with the lead-in dose of nivolumab to 3 months after initiation of therapy. Infusions reactions were seen early with the lead-in/cycle 1, while dermatitis was seen from initial exposure with the lead-in and for ≤3 months later on treatment. Thyroid disorders were seen across the entirety of the treatment period. The only case of myocarditis occurred after cycle 1. Pneumonitis cases were more delayed, typically observed after several months of nivolumab exposure.
There was 1 death in the study, related to COVID-19, after 4 cycles.
Patient-reported outcomes
Fourteen patients responded to the GPI measure at baseline, with a median score of 10.75, and an interquartile range of 9.62 to 13.50. Among the 22 patients evaluable for efficacy at the MTD, patients reported a quality of life on average comparable to that of the general population on the FAACT measure (where higher FAACT scores would indicate better quality of life). The average total functional assessment of cancer therapy-general score was 85 (standard deviation [SD] 12), compared with 80.1 (SD 18.1) in normative data.26 Subscale scores included Physical Well-being at 23.3 (SD 5.4) vs 22.7 (SD 5.4) in the general population, Social/Family Well-being at 24.0 (SD 5.3) vs 19.1 (SD 6.8), Emotional Well-being at 18.9 (SD 3.5) vs 19.9 (SD 4.8), and Functional Well-being at 18.4 (SD 5.6) vs 18.5 (SD 6.8).
Most patients reported no treatment-related symptoms on the National Cancer Institute PRO-CTCAE, which in general evaluated cardiovascular, pulmonary, gastrointestinal, genitourinary, dermatologic, musculoskeletal, nervous system, gynecologic, memory, psychological, and pain-related symptoms. Over 70% of patients reported no symptoms in most domains, while ∼30% or fewer reported issues like dry mouth, hoarseness, decreased appetite, heartburn, constipation, diarrhea, abdominal pain, shortness of breath, coughing, itching, numbness, or tingling.
Common side-effects included mild to severe pain (reported by 67%), though <30% noted pain interference. Headache, muscle pain, or joint pain was reported by 30% to 50%, with <30% experiencing interference due to these pains. Insomnia affected 81% of patients, and 62% reported mild to very severe fatigue. Psychological symptoms such as anxiety or sadness were noted by ∼60%. Urinary emergency of some extent was reported by 62%, excessive sweating by 33%, and body odor by 38%. These findings reflect a range of mild to moderate side-effects, with most patients experiencing minimal impact on their overall quality of life during therapy.
Exploratory analysis of biologic correlates
Through edgeR analysis and a 2-tailed t-test with multiple-comparison correction using the Benjamini-Hochberg adjustment, we found that there were increased frequencies of circulating myeloid-derived suppressor cells, exhausted-like CD4+PD-1+CD39+ T cells, and CD4+CD39+IFN-γ– (or perforin-) T cells having less effector function at both LIV and C1D1 in progressors (Pro) compared with nonprogressors (NP) with P < .05. Notably, there was a lower frequency of fragile-like IFN-γ producing CD4+Foxp3+ Treg at LIV in NP than Pro (Figure 3) with P < .05. Furthermore, there was a significant reduction in exhausted-like CD4+PD-1+CD39+ T-cell levels at C1D1 in comparison to LIV in NP but not Pro (P < .05). In addition, at LIV but not C1D1, there were increased frequencies of circulating B cells (especially naïve B cells), and less exhausted-like CD4+PD-1–IFN-γ+ effector T cells with decreased frequencies of CD4+ naive (CD197+CD45RA+) T cells (CD4 N) and CD4+ central memory (CM; CD197+CD45RA−) T cells (CD4 CM) in patients with immunotoxicity (grade 1-4) compared with patients without immunotoxicity (grade 0), as depicted in Figure 4. There was also a significant increase in CD4 N and CD4 CM cell levels, with a decrease in less exhausted-like CD4+PD-1–IFN-γ+ T-cell levels at C1D1 in comparison to LIV in patients experiencing immunotoxicity as compared with those without such toxicity (P < .05).
Exhausted immunophenotype correlates with disease progression in patients treated with nivolumab–R-CHOP.
Exhausted immunophenotype correlates with disease progression in patients treated with nivolumab–R-CHOP.
Less exhausted-like effector T-cell immunophenotype is associated with greater immunotoxicity in patients treated with nivolumab–R-CHOP.
Less exhausted-like effector T-cell immunophenotype is associated with greater immunotoxicity in patients treated with nivolumab–R-CHOP.
Discussion
This phase 1b study evaluated a novel combination of nivolumab–R-CHOP preceded by a “priming” lead-in dose of nivolumab. The results show preliminary efficacy of the regimen. The study did have patients with disease skewed towards germinal center origin; however, the study was enriched with patients with high-risk disease profiles, such as transformed low-grade lymphoma, high-risk IPI, and MYC aberrancy. Therefore, the achievement of ORR, PFS, and OS rates higher than historic controls with R-CHOP is encouraging, with the caveat that this is a phase 1b study.
In landmark trials including LNH 98.5 trial and the phase 3 CALGB 50303 study trial, CR/unconfirmed CR rates for R-CHOP/dose-adjusted etoposide, prednisone, vincristine, cyclophosphamide, doxorubicin with rituximab ranged from ∼60% to 75%, with 24-month PFS rates of 57% to 79%, and OS rates of 70% to 78%.27,28 For trials evaluating adjunctive therapy to R-CHOP such as the POLARIX trial, there have been measurable gains over R-CHOP alone with CR, 24-month PFS, and OS rate of 78%, 77%, and 89%, respectively, in the polatuzumab vedotin, rituximab, cyclophosphamide, doxorucibin, and prednisone arm.29 In comparison to POLARIX, our study included a higher proportion of patients with MYC aberrancies, an adverse prognostic marker even in the absence of a translocation.30 Despite a higher proportion of patients with MYC aberrancy, the addition of nivolumab to R-CHOP in our study provided reasonable outcomes, recognizing the heterogeneity of our population as a limitation. Currently, bispecific antibodies are also being evaluated as adjuncts to chemotherapy in frontline. However, these trials are very selective, much like the POLARIX trial, typically excluding transformed follicular lymphoma.31 This is a subset population where nivolumab–R-CHOP demonstrates encouraging activity, and should be an area of focus for future ICI-based studies.
A recent study (avelumab, rituximab, cyclophosphamide, doxorubicin, vincristine, prednisone) combined another ICI, avelumab, with R-CHOP.32 In the phase 2 trial involving 28 patients, treatment consisted of a priming phase with avelumab-rituximab followed by 6 cycles of R-CHOP, and lastly a consolidation phase with 6 cycles of avelumab. Like our study, impressive ORR and CR rate of 89% and 89%, respectively, were reported after the priming and R-CHOP phases. Progression during the avelumab-rituximab predicted for chemotherapy refractoriness. This priming approach is supported by biologic correlates analyzed in our study. There were demonstrable changes in immune cell subsets at the C1D1 visit compared with the LIV. Patients who did not experience disease progression or relapse had a significant decrease in T cells with an exhausted-like phenotype, an immune cell subset known to be important in tumoral response. The occurrence of toxicity was also predicted by changes in relevant immune cell subsets between the LIV and CID1, suggesting that patients with a “toxicity-leaning” immune profile can be identified prior to onset of toxicity.
The correlation between PD-1/PDL-1 expression and response remains unresolved with our results. In our study, improved response rates with nivolumab–R-CHOP were independent of PD-1/PD-L1 expression, seen with no or low-level expression of the proteins. Several other studies evaluating ICI-chemoimmunotherapy in treatment-naïve DLBCL using a variety of tools to determine protein expression had similar findings. In contrast, a study with pembrolizumab–R-CHOP showed that the PD-L1 expression (by IHC) was a predictor of relapse and PFS with reproducibility across various expression cut-offs (≥5% and ≥30%).33 This reflects the challenges of utilizing PD-1/PDL-1 expression as a predictive biomarker for clinical outcomes with ICI-based therapy. However, we do not believe that ICI should be limited to patients with tumors expressing PD-1/PD-L1.
Adverse effects including hematologic toxicities in our study were not significantly different from those recorded in other studies using nivolumab or R-CHOP. Most were low grade (grades 1-2), and discontinuation due to adverse effects was rarely seen; most patients were able to complete the study regimen.3,27 There was only 1 death in the study, and it was attributable to severe COVID-19. Immunotoxicity was not aggravated by concurrent use of chemotherapy, and most IrAEs were low grade in severity. Of note, the rate of IrAEs was higher than that reported with other large randomized clinical trials with nivolumab. Our biologic correlates provide some insights regarding the immunologic drivers of the observed phenomenon, which probably supersede the immunosuppressive effect of concurrent chemotherapy and steroids.
With future investigation of ICI-based treatments in lymphoma, there needs to be fine-tuning of patient selection: our exploration of correlations between immune subsets and toxicities could help with selection of patients who have a higher chance of improved outcomes with ICI-based regimens but lower risk of toxicity. The variability of results identified with ICI–R-CHOP regimens suggests a need for improved biomarker-driven patient selection. Pretreatment assessment of T-cell fragility, immunophenotype, and stemness, circulating B cells, and myeloid-derived suppressor cells, as demonstrated in our study, could help optimize patient selection for these regimens.
Finally, with our unique incorporation of patient-reported outcome assessment in DLBCL, quality of life during therapy indicated that most patients were minimally affected by side-effects, and maintained a quality of life comparable to that of the general population. As the quest to improve outcomes continues, the incorporation of patient-reported outcomes is important to identify therapies that are not only effective at treating the lymphoma but also tolerable for patients.
Conclusions
The addition of nivolumab to R-CHOP for the treatment of newly diagnosed aggressive B-cell lymphoma has promising efficacy with complete response rates. There was no signal for increased general toxicities stemming from the addition of nivolumab, though immunotoxicity was common. However, patient-reported outcomes data did not suggest an impact of quality of life. Immune cell subsets may inform patients’ selection to optimize efficacy and toxicity for future ICI-based treatments in B-cell lymphoma.
Acknowledgments
This study, an investigator-initiated trial, was funded by Bristol Myers Squibb, the manufacturer of nivolumab.
The manuscript was solely prepared and reviewed by the named authors.
Authorship
Contribution: Q.C. performed and interpreted the PD-1/PDL-1 immunohistochemical studies; O.O. was responsible for clinical trial data review, extracting and analyzing data, interpreting results, and preparation of the manuscript; I.R. contributed to the collection and analysis of data; P.X. and B.Z. analyzed samples for biologic correlates and contributed to the preparation of the manuscript; G.P.K. coordinated the study and provided data support; X.M., R.C., and Y.M. provided statistical support to the study; X.T. facilitated analysis of the patient-reported outcome data; R.B., R.E., V.N., H.S., D.T., F.S., P.V., L.I.G., S.M., J.W., and B.P. were study investigators, and contributed revisions to the final manuscript; and R.K. conceptualized the study, wrote the protocol, served as principal investigator, and supervised the preparation of the manuscript.
Conflict-of-interest disclosure: S.M. reports membership of advisory committee with Juno/Bristol Myers Squibb; and research funding from Juno/Bristol Myers Squibb. L.I.G. reports honoraria from Bristol Myers Squibb. R.K. reports advisory board roles with BeiGene, Bristol Myers Squibb, Gilead/Kite, Genmab, and AbbVie; and speakers’ bureau roles with BeiGene, AstraZeneca, and Bristol Myers Squibb. The remaining authors declare no competing financial interests.
Correspondence: Reem Karmali, Robert H. Lurie Comprehensive Cancer Center, Northwestern University, Suite 805, 676 North Saint Clair St, Chicago, IL 60611; email: reem.karmali@northwestern.edu.
References
Author notes
All relevant data generated or analyzed during this study are included in this submitted manuscript.