Key Points
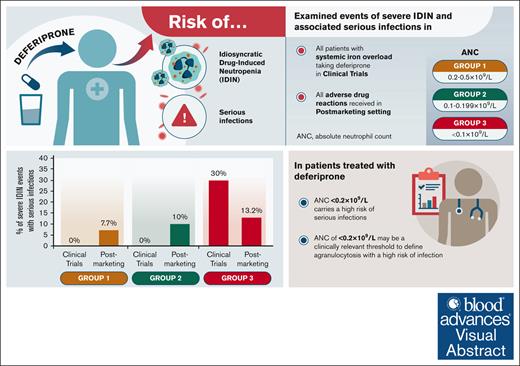
In patients treated with deferiprone, ANC levels <0.2 × 109/L conferred the highest risk of serious infections.
An ANC of <0.2 × 109/L may be a clinically relevant threshold to define agranulocytosis with a high risk of infection.
Visual Abstract
Patients treated with deferiprone for transfusional iron overload may experience idiosyncratic drug–induced neutropenia (IDIN) that may increase risk of infection. This analysis examined the rates of severe IDIN and risk of serious infections at different absolute neutrophil count (ANC) levels during deferiprone treatment. Events of severe IDIN (ANC <0.5 × 109/L) and associated serious infections from clinical trials and postmarketing setting were analyzed by discrete ANC levels: group 1, 0.2 × 109/L to 0.5 × 109/L; group 2, 0.1 × 109/L to 0.199 × 109/L; group 3, <0.1 × 109/L. In clinical trials, 22 events of severe IDIN occurred (group 1, n = 9; group 2, n = 3; group 3, n = 10), and rates of severe IDIN per 100 patient-years were 0.45 in group 1; 0.15 in group 2; and 0.50 in group 3 (1990.26 patient-years deferiprone exposure). All serious infections were in group 3 (3/10 [30.0%]). In the postmarketing setting, 176 events of severe IDIN were reported (group 1, n = 65; group 2, n = 20; group 3, n = 91) and rates of severe IDIN per 100 patient-years were 0.06 in group 1; 0.02 in group 2; and 0.08 in group 3 (111 570.24 patient-years deferiprone exposure). Rates of serious infection were 7.7% (5/65) in group 1; 10% (2/20) in group 2; and 13.2% (12/91) in group 3. Our findings suggest a high risk of serious infections with ANC <0.2 × 109/L during deferiprone treatment, a level consistent with the recent neutropenia guidelines.
Introduction
Acute, unforeseeable, and transient declines in absolute neutrophil counts (ANCs) can occur with the use of some medications, a condition referred to here as idiosyncratic drug–induced neutropenias (IDINs).1-5 Although rare, IDIN may put patients at a high risk of serious and sometimes fatal infections, in particular if IDIN is profound and long lasting.1,2,5-8 For example, it is estimated that as many as 60% of patients with severe IDIN develop septicemia if their infections are not treated aggresively.9 Because patients experiencing IDINs can progress rapidly from having no symptoms or fever to developing sepsis,4 early detection of IDINs and timely measures to increase ANCs are critical to prevent serious infections.2,5,8
Although the clinical characterization of neutropenias into strata of mild (ANC, 1 × 109/L to 1.5 × 109/L), moderate (ANC, 0.5 × 109/L to 1 × 109/L), and severe (ANC, <0.5 × 109/L) helps in predicting the risk of infections in patients with any type of neutropenia, there is a need to further characterize the risk of infections in patients with severe neutropenia with very low ANCs (ie, <0.5×109/L) to establish algorithms for rapid interventions adjusted to ANC levels and specific drugs.
In a study involving 203 patients with severe IDIN, with a median ANC of 0.08 × 109/L (range, 0 to 0.48 × 109/L) at the nadir, clinical features of sepsis with serious infections (eg, extensive pneumonia or septicemia) were observed in >38% of patients, and intensive care was required in 18% of patients.2 The main clinical presentations during hospitalization were isolated fever (26%), septicemia/septic shock (21%), pneumonia (13%), and sore throat/tonsillitis (9%).2 In addition, a systematic review that included data from 980 case reports of nonchemotherapy drug–induced neutropenia found that patients with ANCs <0.1 × 109/L had a significantly higher rate of localized infections, sepsis, and fatal complications than those with ANCs ≥0.1 × 109/L.1 The newly published consensus-based guidelines by the European Hematology Association and the European Network for Innovative Diagnosis and Treatment of Chronic Neutropenias (EHA/EuNet-INNOCHRON) within the European Cooperation in Science & Technology (COST) action state that the term agranulocytosis may be used for severe chronic neutropenias with ANC <0.2 × 109/L.10 Thus, clinical observations and evidence suggest that ANC values of <0.2 × 109/L or <0.1 × 109/L may better identify patients at the highest risk of serious infections compared with the broader range of ANC values of 0.2 × 109/L to 0.5 × 109/L. The risks of serious infections vary not only with the degree or depth of neutropenia but also with the drugs involved and the duration of neutropenia. Thus, certain drugs are associated with IDINs that are more severe and longer lasting (eg, metamizole and clozapine)1,3,11 than others (eg, trimethoprim sulphamethoxazole),12 probably relating to a drug-specific mechanism of interference with various stages of neutropoiesis.
Deferiprone (Ferriprox) is an oral iron chelator that can be associated with transient episodes of neutropenia or severe neutropenia.5,13-16 Deferiprone is indicated for the treatment of transfusional iron overload in adult and pediatric patients with thalassemia, sickle cell disease (SCD), or other anemias.17,18 Treatment with deferiprone is associated with favorable safety and efficacy outcomes, both as monotherapy19,20 or in combination with other chelators.19,21 As described previously by Tricta et al, based on the ANC cutoff of <0.5 × 109/L (termed as agranulocytosis in the deferiprone US prescribing information), the incidence of severe IDIN was 1.7% in pooled clinical trials of 642 patients with thalassemia syndromes and 1.5% in pooled clinical trials of 196 patients with SCD or other anemias.17,18,22 However, the risk of infection and rates of severe IDIN at ANCs of <0.2 × 109/L or <0.1 × 109/L in patients treated with deferiprone have not been described.
In this analysis, we extracted events of severe IDIN from company-sponsored clinical trials of deferiprone and the postmarketing setting. We then examined the rates of severe IDIN as well as the risk of serious infections at 3 discrete ANC levels.
Methods
Data source
Company-sponsored clinical trials
Events of severe IDIN from clinical trials were extracted from data associated with all patients with systemic iron overload (thalassemia syndromes, SCD, or other conditions) who received at least 1 dose of deferiprone across 15 company-sponsored clinical trials from 1993 to 31 August 2021. Patients treated in >1 clinical trial were counted once. For this analysis, severe IDIN was defined as any reported event of agranulocytosis, which was defined as ANC <0.5 × 109/L in the study protocols, investigator’s brochures, and deferiprone US prescribing information.
Postmarketing setting
Events of severe IDIN were identified from individual case safety reports (ICSRs) from the deferiprone postmarketing surveillance program since its approval on 25 August 1999 to 31 August 2021. Similar to the definition used in clinical trials, ICSRs with adverse drug reactions coded to the term agranulocytosis were extracted and defined as events of severe IDIN for this analysis. Some ICSRs coded to the term agranulocytosis did not have ANC values reported, and confirmatory ANC values were not always available in the postmarketing setting. Events of severe IDIN that did not have ANC values were excluded, and those with at least 1 ANC value were included for analysis.
Patient narratives in the ICSRs were compiled from reports that were solicited and/or spontaneously reported by patients, caregivers, pharmacists, and/or health care providers. Patient narratives could include demographics, medical history, suspected and concomitant medications, description of the case (eg, ANC measurements, relevant laboratory tests, time to onset, duration, severity, outcome, and rechallenge), and causality assessment. Additional information relevant to each event was also collected. All patient data were deidentified before being reported to the pharmacovigilance department at Chiesi.
Analysis of rates of severe IDIN
Rates of severe IDIN were normalized to estimated deferiprone exposure, which was expressed as the number of severe IDIN events per 100 patient-years. In the postmarketing setting, exposure to deferiprone was estimated from the cumulative worldwide sales and a defined daily dose of 75 mg/kg. For tablet formulations (500 and 1000 mg, both 3 times a day and twice a day formulation), 1 patient-year of exposure is considered equivalent to 1 643 625 mg of sales; at an average patient weight of 60 kg and the defined daily dose of 75 mg/kg, the daily dose requirement is 4500 mg, taken 365.25 days per year. For oral solution (100 mg/mL), 1 patient-year of exposure is considered equivalent to 1 095 750 mg of sales; because expected use of this formulation is mostly by pediatric patients, a lower average patient weight is used than that which is used for the tablet formulations; at an average patient weight of 40 kg and the defined daily dose of 75 mg/kg, the daily dose requirement is 3000 mg, taken 365.25 days per year.
Analysis of serious infections
Infections that led to hospitalizations and life-threatening complications, including death, were reported as serious and/or severe based on Common Terminology Criteria for Adverse Events criteria. Serious and/or severe infections that occurred within 2 weeks of onset of severe IDINs were of particular interest for the purpose of this analysis. Reported data associated with infections were coded using the Medical Dictionary for Regulatory Activities. When available, additional data on patient medical history, concomitant medications, and associated adverse events were used in the analysis of infection episodes.
Serious infectious events were defined as any event that resulted in death, was life-threatening, required or prolonged hospitalization, caused disability or permanent damage, resulted in a congenital anomaly or birth defect, required intervention to prevent permanent impairment or damage, or was classified as an important medical event. Life-threatening infectious events were defined as any event that placed the patient at immediate risk of death. Severe infections were defined as any event that was incapacitating and required medical intervention.
Regulatory obligations require the reporting of “serious” and “severe”; however, “serious” is not the same as “severe.” The term “serious” is based on patient/event outcome usually associated with events that pose a threat to a patient’s life or functioning. The term “severe” is often used to describe the intensity (severity) of a specific event (as in mild, moderate, or severe). For the purpose of this analysis, we are using the term “serious” to indicate infections that were reported as serious, severe, or life-threatening in clinical trials and postmarketing ICSRs.
Data analysis
Events of severe IDIN as well as the associated serious infections were analyzed by 3 discrete ANC groups based on the nadir ANC: group 1, ANC 0.2 × 109/L to 0.5 × 109/L; group 2, ANC 0.1 × 109/L to 0.199 × 109/L; or group 3, ANC <0.1 × 109/L. To examine any clinically significant trends, events of severe IDIN were additionally analyzed by 3 all-encompassing ANC thresholds: <0.5 × 109/L, <0.2 × 109/L, and <0.1 × 109/L.
The incidence of severe IDIN was analyzed in clinical trials but not in the postmarketing setting owing to the uncertainty in the actual number of patients who received deferiprone and missing patient information. This analysis focused primarily on the rates of severe IDIN normalized to exposure per 100 patient-years to achieve consistency in data reporting between clinical trials and the postmarketing setting.
Results
Company-sponsored clinical trials
Overall, 22 events of severe IDIN were reported in deferiprone-treated patients enrolled across 15 clinical trials. Severe IDINs occurred predominantly in females (61.9%) and in patients diagnosed with thalassemia major (57.1%) (Table 1). The mean time from initiation of deferiprone to onset of severe IDIN was 736.2 days (standard deviation [SD], 1461.3 days). Severe IDINs resolved, or patients recovered with permanent (15/22 [68.2%]) or temporary (4/22 [18.2%]) discontinuation of deferiprone; in the remaining events, 1 recovered with no action taken; 1 recovered, and the action was not applicable because the patient had already ended exposure with deferiprone; and 1 resulted in a fatal outcome. In 14 of 22 events (63.3%), granulocyte colony-stimulating factor (G-CSF) treatment was initiated at a mean of 3.1 (SD, 3.8) days after the onset of severe IDIN. The total deferiprone exposure was 1990.26 patient-years. The total deferiprone exposure in clinical trials is based on a total of 977 patients with systemic iron overload who received at least 1 dose of deferiprone.
Demographics in sponsored clinical trials
| Demographics . | Cases of severe IDIN, n (%) (n = 21∗) . |
|---|---|
| Sex | |
| Female | 13 (61.9) |
| Male | 8 (38.1) |
| Age category, y | |
| 0-5 | 3 (14.3) |
| 6-11 | 6 (28.6) |
| 12-16 | 1 (4.8) |
| 17-35 | 5 (23.8) |
| 36-64 | 6 (28.6) |
| Diagnosis | |
| Thalassemia major | 12 (57.1) |
| Thalassemia intermedia | 1 (4.8) |
| Hereditary hemochromatosis | 2 (9.5) |
| Hereditary spherocytosis | 2 (9.5) |
| Myelodysplasia | 2 (9.5) |
| Sickle cell anemia | 1 (4.8) |
| SCD | 1 (4.8) |
| Demographics . | Cases of severe IDIN, n (%) (n = 21∗) . |
|---|---|
| Sex | |
| Female | 13 (61.9) |
| Male | 8 (38.1) |
| Age category, y | |
| 0-5 | 3 (14.3) |
| 6-11 | 6 (28.6) |
| 12-16 | 1 (4.8) |
| 17-35 | 5 (23.8) |
| 36-64 | 6 (28.6) |
| Diagnosis | |
| Thalassemia major | 12 (57.1) |
| Thalassemia intermedia | 1 (4.8) |
| Hereditary hemochromatosis | 2 (9.5) |
| Hereditary spherocytosis | 2 (9.5) |
| Myelodysplasia | 2 (9.5) |
| Sickle cell anemia | 1 (4.8) |
| SCD | 1 (4.8) |
In 1 case, 1 patient had 2 events of severe IDIN.
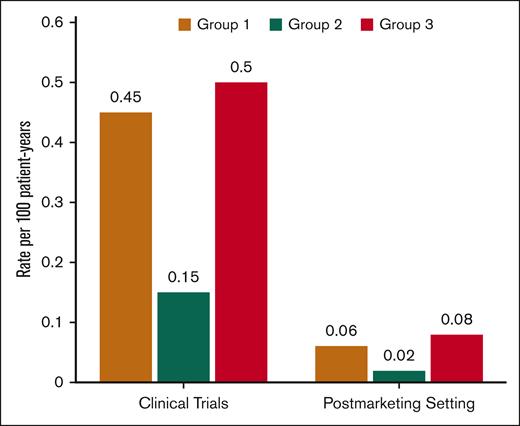
Stratification of severe IDIN events by discrete ANC groups demonstrated that 9 events were within group 1, a total of 3 events were within group 2, and 10 events were within group 3. Rates of severe IDIN per 100 patient-years were 0.45 for group 1; 0.15 for group 2; and 0.50 for group 3 (Table 2; Figure 1). The median durations of severe IDIN stratified by ANC groups were 16 days (range, 3-93) within group 1; 3 days (range, 2-5) within group 2; and 4 days (range, 3-13) within group 3. One event of severe IDIN in group 1 lasted 93 days; excluding this event resulted in a median duration of severe IDIN of 14 days (range, 3-21).
Summary of occurrence of events of severe IDIN in patients treated with deferiprone
| . | Severe IDIN . | |||||
|---|---|---|---|---|---|---|
| ANC thresholds, ×109/L . | ANC groups, ×109/L . | |||||
| <0.5 . | <0.2 . | <0.1 . | Group 1, 0.2-0.5 . | Group 2, 0.1-0.199 . | Group 3, <0.1 . | |
| Cumulative deferiprone exposure in clinical trials∗= 1990.26 patient-y | ||||||
| Events, n (rate/100 patient-y) | 22 (1.11) | 13 (0.65) | 10 (0.50) | 9 (0.45) | 3† (0.15) | 10† (0.50) |
| Cumulative deferiprone exposure in the postmarketing setting = 111 570.24 patient-y | ||||||
| Events‡, n (rate/100 patient-y) | 176 (0.16) | 111 (0.10) | 91 (0.08) | 65 (0.06) | 20 (0.02) | 91 (0.08) |
| . | Severe IDIN . | |||||
|---|---|---|---|---|---|---|
| ANC thresholds, ×109/L . | ANC groups, ×109/L . | |||||
| <0.5 . | <0.2 . | <0.1 . | Group 1, 0.2-0.5 . | Group 2, 0.1-0.199 . | Group 3, <0.1 . | |
| Cumulative deferiprone exposure in clinical trials∗= 1990.26 patient-y | ||||||
| Events, n (rate/100 patient-y) | 22 (1.11) | 13 (0.65) | 10 (0.50) | 9 (0.45) | 3† (0.15) | 10† (0.50) |
| Cumulative deferiprone exposure in the postmarketing setting = 111 570.24 patient-y | ||||||
| Events‡, n (rate/100 patient-y) | 176 (0.16) | 111 (0.10) | 91 (0.08) | 65 (0.06) | 20 (0.02) | 91 (0.08) |
ADR, adverse drug reaction.
Total of 977 patients with systemic iron overload were treated with deferiprone in clinical trials.
One patient had 2 events of severe IDIN, the event with ANC 0.18 × 109/L was counted in group 2, and the event with ANC 0 × 109/L was counted in group 3.
Events of severe IDIN in the postmarketing setting are defined as adverse drug reactions coded to agranulocytosis that had at least 1 ANC value.
Rates of severe IDIN in patients treated with deferiprone across the clinical-development program. Stratification of rates of severe IDIN from clinical trials or postmarketing setting by discrete ANC groups based on the nadir ANC: group 1, ANC 0.2 × 109/L to 0.5 × 109/L; group 2, ANC 0.1 × 109/L to 0.199 × 109/L; or group 3, ANC <0.1 × 109/L. Rates of severe IDIN were normalized to estimated deferiprone exposure and expressed as the number of severe IDIN events per 100 patient-years.
Rates of severe IDIN in patients treated with deferiprone across the clinical-development program. Stratification of rates of severe IDIN from clinical trials or postmarketing setting by discrete ANC groups based on the nadir ANC: group 1, ANC 0.2 × 109/L to 0.5 × 109/L; group 2, ANC 0.1 × 109/L to 0.199 × 109/L; or group 3, ANC <0.1 × 109/L. Rates of severe IDIN were normalized to estimated deferiprone exposure and expressed as the number of severe IDIN events per 100 patient-years.
The incidence of severe IDIN stratified by ANC levels ranged from 1.02% to 0.31% among the clinical trial cohort. Based on the ANC groups, 9 events of severe IDIN occurred in 9 patients in group 1 for an incidence of 0.92%; 3 events occurred in 3 patients in group 2 for an incidence of 0.31%; and 10 events occurred in 10 patients in group 3 for an incidence of 1.02%.
A summary of serious infections observed in the clinical trials is shown in Table 3. Of the 12 events of severe IDIN in groups 1 and 2, none were associated with any serious infections. Of the 10 events in group 3, a total of 3 (30%) were associated with serious infections. Brief descriptions of these 3 patient cases are presented below. Note that patient case descriptions below may include the term “agranulocytosis” per the terminology used for regulatory reporting in the deferiprone clinical-development program.
Summary of serious infections in patients treated with deferiprone in sponsored clinical trials
| Total patients (N = 977) . | |||||||
|---|---|---|---|---|---|---|---|
| ANC range, × 109/L . | Primary diagnosis . | Serious/severe infections, n . | Preferred term . | Nadir ANC, × 109/L . | Characteristics of infection . | ||
| Severity seriousness . | Causality to DFP . | Outcome . | |||||
| Group 1 (0.2-0.5) | — | 0 | — | — | — | — | — |
| Group 2 (0.1-0.199) | — | 0 | — | — | — | — | — |
| Group 3 (<0.1) | 3 | ||||||
| Hereditary spherocytosis | Parvovirus | 0 | Severe serious | Not related | Hospitalized, recovered | ||
| Hereditary hemochromatosis | Pseudomonal sepsis | 0.01 | NA serious | Related | Hospitalized, fatal | ||
| Hereditary hemochromatosis | RTI and esophageal candidiasis | 0.01 | Severe not serious | Related | Hospitalized, recovered with sequelae | ||
| Total patients (N = 977) . | |||||||
|---|---|---|---|---|---|---|---|
| ANC range, × 109/L . | Primary diagnosis . | Serious/severe infections, n . | Preferred term . | Nadir ANC, × 109/L . | Characteristics of infection . | ||
| Severity seriousness . | Causality to DFP . | Outcome . | |||||
| Group 1 (0.2-0.5) | — | 0 | — | — | — | — | — |
| Group 2 (0.1-0.199) | — | 0 | — | — | — | — | — |
| Group 3 (<0.1) | 3 | ||||||
| Hereditary spherocytosis | Parvovirus | 0 | Severe serious | Not related | Hospitalized, recovered | ||
| Hereditary hemochromatosis | Pseudomonal sepsis | 0.01 | NA serious | Related | Hospitalized, fatal | ||
| Hereditary hemochromatosis | RTI and esophageal candidiasis | 0.01 | Severe not serious | Related | Hospitalized, recovered with sequelae | ||
DFP, deferiprone; NA, not applicable; RTI, respiratory tract infection.
One patient with hereditary spherocytosis had a parvovirus infection with diarrhea, a maculopapular rash, and pyrexia resulting in hospitalization. During hospitalization, the patient had ANC values that decreased from 3.25 × 109/L to 0.56 × 109/L and reached a nadir of 0 × 109/L. Deferiprone was discontinued, and G-CSF treatment was initiated. After 3 days, the ANC increased to 1.56 × 109/L. This episode of agranulocytosis was reassessed as unlikely related to the use of deferiprone but rather associated with parvovirus infection, considering the manifestation of signs of infection before the onset of agranulocytosis. The parvovirus infection was deemed serious and not related to deferiprone.
A second patient with hereditary hemochromatosis was receiving deferiprone for severe cardiac iron overload and had a history of neutropenia before initiating deferiprone. The patient was hospitalized for 13 days with their ANCs ranging from 0.01 × 109/L to 0.06 × 109/L. Although there were no signs or symptoms of infections before noting agranulocytosis, the patient developed esophageal candidiasis and respiratory tract infection after developing agranulocytosis. Deferiprone was discontinued, G-CSF was initiated, and the patient recovered with mild sequelae. The infections were considered nonserious but severe and likely to be related to deferiprone-induced agranulocytosis.
A third patient also had hereditary hemochromatosis and a history of multiple comorbidities, including hypertension, chronic obstructive pulmonary disease, liver cirrhosis, and congestive heart failure. This patient developed agranulocytosis (ANC of 0.1 × 109/L) ∼3 months after the initiation of deferiprone therapy and was hospitalized with Pseudomonas sepsis. Deferiprone was discontinued. The patient had ANC values ranging from 0 × 109/L to 3.2 × 109/L during the 5-day hospitalization, developed complications of atrial fibrillation, experienced acute kidney failure, and died. The cause of death was multisystem organ failure secondary to Pseudomonas sepsis, hospital-acquired pneumonia, and deferiprone-induced agranulocytosis. The comorbidity of ischemic heart disease and a recent episode of congestive heart failure might have also contributed to the onset of atrial fibrillation, kidney failure, and subsequent death.
Postmarketing setting
To determine whether what we observed in sponsored clinical trials is consistent with real-world settings, we analyzed data from the deferiprone postmarketing surveillance program. We extracted a total of 238 events that were reported as agranulocytosis (ie, ICSRs that coded to the term “agranulocytosis,” with or without ANC values reported) and defined as events of severe IDIN for the purpose of this analysis. Severe IDIN occurred predominantly in females (56.8%) and those diagnosed with thalassemia syndromes (69.9%) in the postmarketing setting (Table 4). The mean time from the initiation of deferiprone to severe IDIN was 398.2 days (SD, 716.3 days) among 185 events with evaluable data. Most events of severe IDIN either resolved (171/238 [71.8%]), were resolving (14/238 [5.9%]), or resolved with sequelae (2/238 [0.8%]); other cases were associated with ongoing (4/238 [1.7%]), unknown (28/238 [11.8%]), or fatal (19/238 [8.0%]) outcomes. Cumulative deferiprone exposure was estimated to amount to 111 570.24 patient-years.
Demographics in the postmarketing setting
| Demographics . | Cases of severe IDIN, n (%) (n = 236) . |
|---|---|
| Sex | |
| Female | 134 (56.8) |
| Male | 99 (41.9) |
| Missing data | 3 (1.3) |
| Age category, y | |
| 0-5 | 11 (4.7) |
| 6-11 | 18 (7.6) |
| 12-16 | 31 (13.1) |
| 17-35 | 91 (38.6) |
| 36-64 | 42 (17.8) |
| ≥65 | 22 (9.3) |
| Missing data | 21 (8.9) |
| Diagnosis | |
| Thalassemia major | 165 (69.9) |
| Other | 71 (30.1) |
| Demographics . | Cases of severe IDIN, n (%) (n = 236) . |
|---|---|
| Sex | |
| Female | 134 (56.8) |
| Male | 99 (41.9) |
| Missing data | 3 (1.3) |
| Age category, y | |
| 0-5 | 11 (4.7) |
| 6-11 | 18 (7.6) |
| 12-16 | 31 (13.1) |
| 17-35 | 91 (38.6) |
| 36-64 | 42 (17.8) |
| ≥65 | 22 (9.3) |
| Missing data | 21 (8.9) |
| Diagnosis | |
| Thalassemia major | 165 (69.9) |
| Other | 71 (30.1) |
Of these 238 events, 176 had at least 1 ANC value reported and were analyzed. There were 65 events of severe IDIN in group 1; 20 events in group 2; and 91 events in group 3. Rates of severe IDIN stratified by ANC groups and all-encompassing ANC thresholds are summarized in Table 2 and Figure 1.
As with the clinical trial setting, in the postmarketing setting, the occurrence of serious infections was higher with lower ANC levels. A total of 19 serious infectious events were identified; all infectious events required hospitalization and resulted in either recovery (n = 6), death (n = 12), or unknown outcome (n = 1). A summary of these infectious events is shown in Table 5.
Summary of serious infections in patients treated with deferiprone in the postmarketing setting
| Total DFP exposure (111 570.24 patient-y) . | |||||||
|---|---|---|---|---|---|---|---|
| ANC range, ×109/L . | Primary diagnosis . | Infections, n . | Preferred term, Infection term . | Medical history . | Nadir ANC, ×109/L . | Outcome . | Reported cause of death . |
| Group 1 (0.2-0.5) | 5 | ||||||
| β-thalassemia major | Septic shock | Episode of mild leukopenia | 0.4 | Hospitalized, recovered | N/A | ||
| β-thalassemia major | Breast abscess | Severe cardiopathy | 0.4 | Hospitalized, recovered | N/A | ||
| Hereditary hemochromatosis | Fungal sepsis | Inborn hemochromatosis, micronodular cirrhosis, diabetes | 0.2 | Hospitalized, fatal | Septic shock | ||
| β-thalassemia major | Septic shock | No significant history | 0.48 | Hospitalized, fatal | Septic shock | ||
| Diamond Blackfan anemia | Sepsis | Hypothyroidism | 0.27 | Hospitalized, fatal | Sepsis | ||
| Group 2 (0.1-0.199) | 2 | ||||||
| β-thalassemia major | Infectious pleural effusion | No significant history | 0.1 | Hospitalized, recovered | N/A | ||
| β-thalassemia major | Sepsis | Positive serology for Hep C | 0.1 | Hospitalized, fatal | Agranulocytosis and sepsis | ||
| Group 3 (<0.1) | 12 | ||||||
| β-thalassemia major | Oropharyngeal pain | Cardiomyopathy, T1D | 0 | Hospitalized, recovered | N/A | ||
| Aplasia pure red cell | Neutropenic sepsis | Cardiac transplant, end-stage renal failure | 0 | Hospitalized, recovered | N/A | ||
| β-thalassemia major | Mucormycosis | Severe cardiac iron overload, amenorrhea, osteoporosis, extramedullary hematopoiesis | 0 | Hospitalized, recovered with sequelae | N/A | ||
| β-thalassemia major | Herpes simplex | Severe neutropenia on deferiprone therapy | <0.1 | Hospitalized, unknown | N/A | ||
| β-thalassemia major | Septic shock | Hypoparathyroidism | 0 | Hospitalized, fatal | Sepsis | ||
| β-thalassemia major | Rash pustular and septic shock | Regular transfusions | 0 | Hospitalized, fatal | Sepsis | ||
| β-thalassemia major | Sepsis | Hemosiderosis | 0.05 | Hospitalized, fatal | Not reported | ||
| α-thalassemia | Sepsis | Not reported | 0.01 | Hospitalized, fatal | Sepsis | ||
| Secondary hemochromatosis∗ | Furuncle | Lower UTI with right renal lithiasis, paroxysmal cardiac rhythm troubles, dyslipemia | 0.01 | Hospitalized, fatal | Infection | ||
| β-thalassemia major | Sepsis | Failed BMT | <0.1 | Hospitalized, fatal | Sepsis and cardiac arrest | ||
| β-thalassemia major | Sepsis and lymphadenitis | Cardiac hemosiderosis, splenectomy | 0.02 | Hospitalized, fatal | Febrile neutropenia, multiple organ dysfunction syndrome, pneumonia, sepsis | ||
| Congenital sideroblastic anemia | Septic shock and Streptococcal bacteremia | Severe RA, CHF, c.560G > A mutation in SLC25A38 | 0.05 | Hospitalized, fatal | Cardiogenic shock, congestive cardiomyopathy, iron overload, septic shock, agranulocytosis, Streptococcal bacteremia | ||
| Total DFP exposure (111 570.24 patient-y) . | |||||||
|---|---|---|---|---|---|---|---|
| ANC range, ×109/L . | Primary diagnosis . | Infections, n . | Preferred term, Infection term . | Medical history . | Nadir ANC, ×109/L . | Outcome . | Reported cause of death . |
| Group 1 (0.2-0.5) | 5 | ||||||
| β-thalassemia major | Septic shock | Episode of mild leukopenia | 0.4 | Hospitalized, recovered | N/A | ||
| β-thalassemia major | Breast abscess | Severe cardiopathy | 0.4 | Hospitalized, recovered | N/A | ||
| Hereditary hemochromatosis | Fungal sepsis | Inborn hemochromatosis, micronodular cirrhosis, diabetes | 0.2 | Hospitalized, fatal | Septic shock | ||
| β-thalassemia major | Septic shock | No significant history | 0.48 | Hospitalized, fatal | Septic shock | ||
| Diamond Blackfan anemia | Sepsis | Hypothyroidism | 0.27 | Hospitalized, fatal | Sepsis | ||
| Group 2 (0.1-0.199) | 2 | ||||||
| β-thalassemia major | Infectious pleural effusion | No significant history | 0.1 | Hospitalized, recovered | N/A | ||
| β-thalassemia major | Sepsis | Positive serology for Hep C | 0.1 | Hospitalized, fatal | Agranulocytosis and sepsis | ||
| Group 3 (<0.1) | 12 | ||||||
| β-thalassemia major | Oropharyngeal pain | Cardiomyopathy, T1D | 0 | Hospitalized, recovered | N/A | ||
| Aplasia pure red cell | Neutropenic sepsis | Cardiac transplant, end-stage renal failure | 0 | Hospitalized, recovered | N/A | ||
| β-thalassemia major | Mucormycosis | Severe cardiac iron overload, amenorrhea, osteoporosis, extramedullary hematopoiesis | 0 | Hospitalized, recovered with sequelae | N/A | ||
| β-thalassemia major | Herpes simplex | Severe neutropenia on deferiprone therapy | <0.1 | Hospitalized, unknown | N/A | ||
| β-thalassemia major | Septic shock | Hypoparathyroidism | 0 | Hospitalized, fatal | Sepsis | ||
| β-thalassemia major | Rash pustular and septic shock | Regular transfusions | 0 | Hospitalized, fatal | Sepsis | ||
| β-thalassemia major | Sepsis | Hemosiderosis | 0.05 | Hospitalized, fatal | Not reported | ||
| α-thalassemia | Sepsis | Not reported | 0.01 | Hospitalized, fatal | Sepsis | ||
| Secondary hemochromatosis∗ | Furuncle | Lower UTI with right renal lithiasis, paroxysmal cardiac rhythm troubles, dyslipemia | 0.01 | Hospitalized, fatal | Infection | ||
| β-thalassemia major | Sepsis | Failed BMT | <0.1 | Hospitalized, fatal | Sepsis and cardiac arrest | ||
| β-thalassemia major | Sepsis and lymphadenitis | Cardiac hemosiderosis, splenectomy | 0.02 | Hospitalized, fatal | Febrile neutropenia, multiple organ dysfunction syndrome, pneumonia, sepsis | ||
| Congenital sideroblastic anemia | Septic shock and Streptococcal bacteremia | Severe RA, CHF, c.560G > A mutation in SLC25A38 | 0.05 | Hospitalized, fatal | Cardiogenic shock, congestive cardiomyopathy, iron overload, septic shock, agranulocytosis, Streptococcal bacteremia | ||
BMT, bone marrow transplant; CHF, congestive heart failure; Hep C, hepatitis C virus; T1D, type 1 diabetes; N/A, not applicable; RA, rheumatoid arthritis; UTI, urinary tract infection.
The patient was diagnosed with secondary hemochromatosis about a year before the event of agranulocytosis at age 71 years; however, the patient narrative does not include the underlying cause of hemochromatosis.
In group 1, a total of 5 serious infectious events were reported in 5 patients among the 65 total severe IDIN events (7.7%). Of these 5 infectious events, 3 (4.6%) resulted in deaths, all due to sepsis.
In group 2, a total of 2 serious infectious events were reported in 2 patients among the 20 total severe IDIN events (10.0%). One patient with β-thalassemia major had a life-threatening infection with high-grade pyrexia and ANC of 0.1 × 109/L ∼3 months after initiating deferiprone. Deferiprone was discontinued, and ANC levels recovered in a week, but the patient developed pneumonia complicated by massive hemoptysis secondary to the rupture of pulmonary artery aneurism. Pneumonia was considered serious and related to deferiprone-induced severe IDIN. A second patient with β-thalassemia died 7 months after the start of deferiprone when they developed sore throat with progressive worsening. The lowest reported ANC was 0.1 × 109/L. The preliminary cause of death was septic shock, and autopsy report was not available for this patient.
In group 3, a total of 12 serious infectious events were reported by 12 patients among the 91 total severe IDIN events (13.2%). Of these, 8 (8.8%) were fatal, all due to sepsis. Among the nonfatal serious infectious events, 1 patient with transfusion-dependent red cell aplasia with a history of cardiac transplant and end-stage renal failure developed neutropenia and neutropenic sepsis within 3 months of starting deferiprone. The patient had a nadir ANC of 0 × 109/L, which resolved in ∼3 weeks. A second patient with β-thalassemia and diabetes developed pancytopenia after 1.5 months on deferiprone therapy. Deferiprone was discontinued when the patient became neutropenic (ANC of 1.1 × 109/L). However, the patient developed oropharyngeal pain, fever, and diarrhea with a nadir ANC of 0 × 109/L, requiring hospitalization and G-CSF, and eventually recovered within a week. A third patient with β-thalassemia and a history of severe cardiac iron overload developed severe neutropenia (ANC, 0 × 109/L) 3 weeks after starting deferiprone and was diagnosed with invasive mucormycosis. The infection was considered to be related to deferiprone-induced neutropenia but resolved with sequelae. A fourth patient with β-thalassemia developed lymphopenia and severe neutropenia on deferiprone with a nadir ANC of 0 × 109/L, ∼4 years after deferiprone initiation. The patient was hospitalized for sepsis and disseminated herpes simplex along with extensive mucositis. ANC levels recovered after 7 days with G-CSF treatment, and the event was considered to be associated with deferiprone.
Discussion
The most significant adverse drug reaction associated with deferiprone use is a decline in ANC to <0.5 × 109/L, defined as severe IDIN. Several studies have reported rates of severe IDIN ranging from 0.5% to 3.6% with deferiprone use.23-25 Although the incidence of severe IDIN decreases after the first year of therapy,22 its occurrence is associated with a high risk of infection.
Despite the risk of serious infections related to the degree and duration of neutropenia, most patients experiencing severe IDIN usually recover over time with supportive care and timely treatment.26 Without immediate medical intervention, patients with ANC <0.5×109/L can develop septicemia with clinical signs of pneumonia, anorectal, skin, or oropharyngeal infections and septic shock.2,26 With deferiprone-associated severe IDIN, most patients recover neutrophil counts with continued treatment and monitoring27 and rarely is permanent discontinuation required.
In this analysis of severe IDIN events in patients treated with deferiprone in clinical trials and the postmarketing setting, we found that ANC levels <0.1 × 109/L or <0.2 × 109/L are consistently associated with a higher risk of serious infection and/or mortality than ANC levels of 0.2 × 109/L to 0.5 × 109/L. In clinical trials, all serious infections (100%), including 1 fatality, occurred in patients with ANCs <0.1 × 109/L, and no serious infections occurred in patients with ANCs ranging from 0.1 × 109/L to 0.5 × 109/L. No serious infections or fatalities occurred in group 1 despite the generally longer duration of severe IDIN than groups 2 and 3 in clinical trials. In the postmarketing setting, serious infections were generally more common with ANCs of <0.2 × 109/L (10.0% in group 2 and 13.2% in group 3) than ANCs of 0.2 × 109/L to 0.5 × 109/L (7.7%), with fatal outcomes being more likely when ANCs dropped <0.2 × 109/L (9 deaths in groups 2 and 3 vs 3 deaths in group 1). Despite discontinuation of deferiprone at the first sign of infection or fever and treatment with G-CSF, in most of the fatal cases reported in the deferiprone clinical-development program, the patient progressed to developing septic shock or septicemia. In addition, we found that severe IDIN was generally more common in female patients than males, which is consistent with evidence that female sex is an independent risk factor for developing neutropenia.28 The findings that mean time to severe IDIN was ∼2 years in clinical trials and 1 year in the postmarketing setting highlight the importance of monitoring ANC and the signs and symptoms of infection during the first years of deferiprone treatment.
Our findings suggest that patients taking deferiprone are at the highest risk of serious infections at the lowest ANC levels. Several case studies on deferiprone-induced severe neutropenia have described life-threatening conditions, including 2 fatal cases, in which ANCs dropped below 0.1 × 109/L, with a complete lack of neutrophils reported in some patients.13,15,16,29-32 Two of these cases occurred in patients with Diamond Blackfan anemia, for whom deferiprone was associated with an abrupt drop in ANC to ≤0.1 × 109/L within 6 to 9 weeks of therapy initiation.13,31 Both patients presented with persistent high-grade fever and were treated with broad-spectrum antibiotics; 1 of them also received G-CSF but eventually died. To date, 4 incidents of deferiprone–induced severe neutropenia have been recorded in patients with thalassemia, and in all of those cases, ANC levels precipitously dropped to <0.1 × 109/L, with 1 patient dying due to multiorgan failure.15,16,29,32 In addition, Newburger and Dale33 observed that although ANCs of 0.2 × 109/L to 0.5 × 109/L is associated with an increased risk of infection in most patients, ANCs of ≤0.2 × 109/L carries a risk of severe, life-threatening infections with susceptibility to opportunistic organisms. In summary, our findings in this systematic and comprehensive analysis in a very large cohort of patients treated with deferiprone confirm anecdotal reports in the literature that the degree of ANC decline is a critical predictor of risk of infections.
The newly published consensus-based guidelines by the EHA/EuNet-INNOCHRON COST suggest that severe chronic neutropenias with ANCs <0.2 × 109/L might be termed “agranulocytosis” and are associated with a high risk of severe, life-threatening infections.10 In addition, some clinicians use an ANC threshold of <0.1 × 109/L to denote agranulocytosis with the highest risk for infection.5 Here, we have provided clinical evidence for supporting a lower ANC threshold than the previously used <0.5 × 109/L to define agranulocytosis. However, due to the diurnal variations in ANCs and other causes of ANC variability together with lack of precision in measuring very low ANC levels, it is less relevant to differentiate between sharp ANC cutoffs of 0.1 × 109/L or 0.2 × 109/L. Therefore, we suggest that the term agranulocytosis may be used for severe IDIN with ANCs <0.2 × 109/L,34 as suggested by the EHA/EuNet-INNOCHRON COST.10
According to the deferiprone product label, incidence of severe IDIN (termed as agranuclocytosis in deferiprone label) is 1.7% among patients with thalassemia syndromes.17 Additional studies have reported incidence of severe IDIN ranging from 0.5% to 3.6% with deferiprone use based on ANC cutoff of <0.5 × 109/L.23-25,35,36 In our clinical trial cohort of a total 977 patients, 22 events of severe IDIN (ANC < 0.5 × 109/L) occurred in 21 patients for an incidence of 2.15%; 13 events occurred in 12 patients with ANC <0.2 × 109/L for an incidence of 1.23%; and 10 events occurred in 10 patients with ANC <0.1 × 109/L for an incidence of 1.02%. Based on the EHA/EuNet-INNOCHRON COST guidelines10 as well as our analysis, using the clinically relevant ANC cutoff of <0.2 × 109/L reduces the incidence of agranulocytosis from 2.15% to 1.23%. Using the threshold of ANC <0.1 × 109/L, the incidence of agranulocytosis declined from 2.15% to 1.02%. Based on these trends, it appears that ANC cutoffs of <0.2 × 109/L or <0.1 × 109/L may be better thresholds to define deferiprone-induced agranulocytosis.
A limitation of this study is that individual case reports of severe IDIN in the postmarketing setting vary in quality, completeness, and accuracy despite attempts to collect all available relevant information. Due to missing or underreporting of unique patient identifiers, we were unable to perform an accurate analysis of the incidence of severe IDIN from the postmarking setting. In addition, the low number of severe IDIN cases in the clinical setting also precluded the ability to provide accurate and meaningful statistical correlation analyses between serious infections and various factors (eg, duration of neutropenia and presence of organ failure). Furthermore, external factors (eg, environmental or social factors) are difficult to account for but may also influence the rates of severe IDIN in the clinical trial and postmarketing settings. Nevertheless, this study represents, to our knowledge, the largest analysis of all severe IDIN cases in patients treated with deferiprone in clinical trials or postmarketing setting.
In conclusion, our analysis has demonstrated that lower ANC thresholds of <0.2 × 109/L or <0.1 × 109/L are clinically relevant to define deferiprone-induced agranulocytosis associated with a higher risk of serious infections. By using these lower thresholds, clinicians may be able to better assess the risk associated with deferiprone use. Although the idiosyncratic nature of deferiprone-induced agranulocytosis is not a reliable predictor of the ANC trend or the duration of the event, a proactive approach to detecting early signs of infection is recommended for all patients regardless of the severity of neutropenia. Furthermore, this potential change in risk stratification and definition of agranulocytosis may help to improve patients’ access to adequate chelation regimens, leading to lower iron overload and better clinical outcomes.
Acknowledgments
The authors thank all the patients, their families, and the investigators involved in the deferiprone clinical-development program. Medical writing support was provided by Sangeeta Chakraborty and Michael Dyle, contracted by Oxford PharmaGenesis Inc, with funding from Chiesi USA, Inc.
The study was sponsored by Chiesi Global Rare Diseases (formerly ApoPharma Inc).
Authorship
Contribution: F.T., N.T.T., C.F., L.L., and A.R. analyzed the results and created the figures, and S.M.B., J.P., F.T., N.T.T., C.F., L.L., A.R., and S.S. designed the research and wrote the manuscript.
Conflict-of-interest disclosure: S.M.B. received consultancy fees from Chiesi, bluebird bio, Vertex Pharmaceuticals, Forma Therapeutics, Novo Nordisk, Global Blood Therapeutics, Pfizer, Bristol Myers Squibb, and Editas Medicine. J.P. reports consultancy fees from Chiesi. F.T., N.T.T., C.F., L.L., and A.R. are full-time employees of Chiesi Canada Corp. S.S. reports consultancy fees from Chiesi, Agios, bluebird bio, Bristol Myers Squibb, and Forma Therapeutics, and serves on a clinical trial steering committee for CRISPR/Vertex CTX001.
Correspondence: Sujit Sheth, Division of Pediatric Hematology Oncology, Department of Pediatrics, Weill Cornell Medical College, 525 E 68th St, P695, New York, NY 10065; email: shethsu@med.cornell.edu.
References
Author notes
Data sharing requests from external parties will be approved or denied on a case-by-case basis. Chiesi reserves the right to deny requests for all legally appropriate reasons. Data requests that risk sharing participant-level data or proprietary information will not be approved.