Key Points
Systematically updating pedigrees of patients with hemophilia and contacting female relatives reduces underdiagnosis of hemophilia carriers.
Reaching all hemophilia carriers remains challenging and depends on awareness of patients with hemophilia and health care providers.
Visual Abstract
Despite numerous efforts to raise awareness, many hemophilia carriers and female persons with hemophilia (PWHs) remain undiagnosed. Between May 2021 and April 2023, we identified potential and obligate carriers of hemophilia A (HA) and hemophilia B (HB) by updating pedigrees of all PWHs followed at the Cliniques universitaires Saint-Luc, Brussels. Retrospective data on previously screened females were collected, including bleeding history, coagulation factor levels, and testing for the proband’s pathogenic variant. In addition, a proactive approach involved sending 125 invitation letters to unscreened or incompletely screened individuals, through related PWHs. In pedigrees of 287 male PWHs (226 HA and 61 HB) and 7 female index patients from 236 families (184 HA and 52 HB), a total of 900 female individuals were identified. Of those, 454 were obligate and/or genetically proven carriers, and 118 were noncarriers. Genetic testing was conducted in 133 obligate, 237 potential, and 4 sporadic carriers, with 190 obligate and 328 potential carriers remaining untested. Among carriers with known factor levels (261/454), 42 HA (23.0%) and 23 HB carriers (29.5%) had a factor level <40 IU/dL. Carriers with a factor deficiency were screened on average 6 years earlier than other females (P = .034). This study, to our knowledge, represents the first systematic effort to identify potential carriers among families of all PWHs within a single center, emphasizing the challenges in comprehensive screening for female individuals genetically linked to one or more PWHs. Such initiatives are vital for achieving equitable access to hemophilia care for all potentially affected individuals, irrespective of gender. This trial was registered at www.ClinicalTrials.gov as #NCT05217992.
Introduction
The first explicit report of female carriership of hemophilia dates back to 1803, by John Conrad Otto,1 who described a family lineage of several decades earlier, wherein only males were affected by an often fatal bleeding disorder, later named “hemophilia” by Hopff2 and Schoenlein,3 which we now know is marked by a deficiency of coagulation factor VIII (FVIII) (hemophilia A [HA]) or FIX (hemophilia B [HB]). The disease was passed down through generations by female ancestors who appeared to show no symptoms themselves. Thomas Hunt Morgan's discovery of X-linked recessive inheritance in 1910 further elucidated the inheritance pattern described by Otto.4 At the beginning of the 20th century, anecdotal reports of hemophilia carriers experiencing abnormal bleeding surfaced5 and gradually accumulated,6-12 yet research on carriers was mainly focused on the genetic transmission of the disease and not on the potential bleeding consequences. Bleeding symptoms in hemophilia carriers and, thanks to new biomolecular techniques, the diagnosis of carriers gained increasing interest by the end of the 20th century.13 However, it took until 2021, 218 years after Otto’s report, for the term “women and girls with hemophilia” (WGH) to be officially defined by the Scientific and Standardization Committee of the International Society on Thrombosis and Haemostasis.14 Several underlying mechanisms explaining why hemophilia carriers may exhibit low factor levels have been identified, with skewed X-chromosome inactivation being the most commonly described.15-17 Importantly, not only carriers with a factor deficiency may experience abnormal bleeding; it has been reported that a quarter of those with factor levels >50 IU/dL may also experience abnormal bleeding symptoms.14
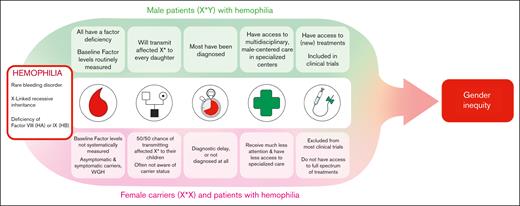
Research on hemophilia carriers and WGH has progressed slower than research focusing on male persons with hemophilia (PWHs) and gender inequities persist in the diagnosis, care, and treatment of hemophilia and bleeding disorders in general 18,19 (Figure 1). Many female relatives of PWHs remain unaware of their carrier status or experience diagnostic delay and their coagulation factor levels are not systematically measured.18-20 In contrast to male PWHs, WGH and carriers often do not benefit from specialized care.18,21 Care gaps for carriers and WGH are even bigger in countries with limited resources,22,23 but even in high-resource countries systemic barriers and political decisions may limit access to care for WGH.24 Despite advancements in hemophilia therapies, including gene therapy and nonreplacement therapies, access for WGH has been limited and they have been excluded from most clinical trials for these new therapeutic agents.14 In addition, the impact of caregiving for affected males on predominantly female caregivers has been largely overlooked.25
At the hemophilia treatment center (HTC) of the Cliniques universitaires Saint-Luc in Brussels, the screening of female relatives of PWHs and the care for WGH and symptomatic carriers have been integral parts of the clinical routine for the past 2 decades. However, before this study, we lacked precise information about the number of carriers and potential carriers within the families of PWHs followed at the center and the effectiveness of our approach. Moreover, despite the increasing interest in hemophilia carriers within the scientific community, concrete strategies for systematic hemophilia carrier screening have been lacking.
In this study, we present the outcomes of a proactive and systematic hemophilia carrier screening study, in which the primary objectives were to screen the highest possible number of potential and obligate hemophilia carriers within a single HTC and to assess the effectiveness of our approach. Furthermore, we aimed to compare carriers of HA and HB, examining circumstances of diagnosis, coagulation factor levels, bleeding symptoms, and hemostatic treatment requirements.
Methods
The study was conducted at the Cliniques universitaires Saint-Luc, Brussels, Belgium, from May 2021 to April 2023 and was approved by the local ethics committee. It was registered at ClinicalTrials.gov (identifier: NCT05217992). The study consisted of both a retrospective and a prospective arm.
While conducting a retrospective data analysis of electronic medical records, we used data acquired through routine carrier screening of female relatives of PWHs. These data included FVIII and FIX levels, genetic testing results, bleeding history, hemostatic treatment history, and family pedigrees. Only data from female individuals presumed to be alive at the start of the study were included in the analysis.
In addition to this retrospective analysis and to further enhance the screening of female relatives of PWHs, we adopted a proactive and systematic approach to reach out to previously unscreened or incompletely screened individuals. During personal contacts with PWHs regularly followed at the HTC (referred to as “probands” hereafter), either during clinical follow-up visits or telephone interviews, pedigrees of probands were analyzed and unscreened potential and obligate carriers of hemophilia were identified, complementing the pedigree information gathered during the retrospective part of the study. Probands were provided with a total of 125 invitation letters to our study, either in paper or electronic form, and were asked to forward these to the unscreened female individuals in their families.
Respondents to the invitation were seen at the clinic, in which their general medical and bleeding history were taken, individual bleeding risk was determined, and coagulation factor levels (FVIII, von Willebrand factor [VWF] Antigen [Ag] and VWF Ristocetin Cofactor activity [RCo] for HA; FIX for HB) were assessed. Coagulation factor levels were measured using a 1-stage assay, a chromogenic assay, or both. For the statistical analysis, the lowest level recorded for each patient was used, regardless of the assay method used. With the informed consent of the participant, genetic testing for the proband’s pathogenic variant was performed. The study was approved by the ethics committee of the Cliniques universitaires Saint-Luc (Comité d'éthique hospitalo-facultaire) in Brussels, Belgium.
Concurrently with both the retrospective and the prospective components of the study, family pedigrees of all PWHs followed at the HTC were updated and digitalized. Anonymized pedigrees were created using PhenoTips and later in Epic when this feature became available at the clinic. In the proactive recruitment arm of the study, only females aged >12 years and <75 years were included. No age limit was applied for retrospective data collection. Statistical analysis of the data was performed using SPSS version 27.
Results
Study population
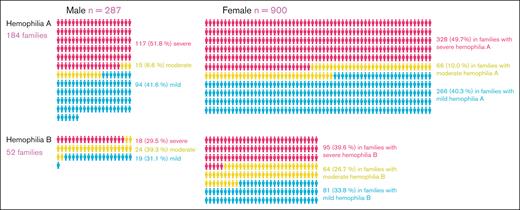
At the time of the analysis, 287 male PWHs (226 HA and 61 HB) were regularly followed at the HTC and causative genetic variants were known in all of them. In addition, 7 female PWHs were considered as probands (3 HA and 4 HB), meaning they were the first individuals to be diagnosed in their respective families. In total, 236 families (184 HA and 52 HB) were registered at the HTC. Twenty appointments at the bleeding disorders clinic were scheduled after the proactive outreach to unscreened potential and obligate carriers. Through retrospective and prospective data collection, 900 presumably alive female individuals could be identified.
An overview of the study population according to sex and hemophilia type and severity is shown in Figure 2. The mean age of male individuals was 39.9 years (range, 1-97) for HA and 40.2 years (range, 3-80) for HB, with 81.9% (n = 235) aged ≥18 years. The mean age of female individuals was 44.1 years (range, 1-99) for families with HA and 44.4 years (range, 5-101) for families with HB, with 90.2% (n = 450) aged ≥18 years. Date of birth was not known in 44.6% of female individuals (n = 401). At least 64 females (7.1%) were living abroad.
Overview of the study cohort, comprising 236 families. In these families, there were ∼3 times as many female individuals who were potential or obligate carriers of hemophilia, based on their position in the family pedigree, compared with male probands. The severities of hemophilia affecting the families are depicted in red (severe), green (moderate), and blue (mild).
Overview of the study cohort, comprising 236 families. In these families, there were ∼3 times as many female individuals who were potential or obligate carriers of hemophilia, based on their position in the family pedigree, compared with male probands. The severities of hemophilia affecting the families are depicted in red (severe), green (moderate), and blue (mild).
Female individuals were categorized into 4 priority groups based on their proximity to the nearest patient with hemophilia in the pedigree (Table 1). Group 1 comprised mothers, sisters, half-sisters (on the mother’s side), daughters, and sporadic carriers (ie, carriers with no other known relatives affected by hemophilia); group 2 maternal aunts, nieces, and granddaughters; group 3 maternal grandmothers and cousins; and group 4 maternal grandaunts and grandcousins. Nine females could not be assigned to a specific priority group.
Prevalence of genetic testing according to hemophilia type, severity, and priority group
| . | Genetic testing performed . | Genetic testing not yet performed . | Total, n (100%) . | P value . |
|---|---|---|---|---|
| HA | .213 | |||
| Severity in family | ||||
| Severe | 129 (39.3%) | 199 (60.7%) | 328 | |
| Moderate | 19 (28.8%) | 47 (71.2%) | 66 | |
| Mild | 93 (35.0%) | 173 (65.0%) | 266 | |
| HB | .001 | |||
| Severity in family | ||||
| Severe | 31 (32.6%) | 64 (67.4%) | 95 | |
| Moderate | 38 (59.4%) | 26 (40.6%) | 64 | |
| Mild | 25 (30.9%) | 56 (69.1%) | 81 | |
| HA | <.001 | |||
| Priority group 1 | 167 (43.0%) | 221 (57.0%) | 388 | |
| Priority group 2 | 43 (26.4%) | 120 (73.6%) | 163 | |
| Priority group 3 | 25 (30.9%) | 56 (69.1%) | 81 | |
| Priority group 4 | 1 (5.3%) | 18 (94.7%) | 19 | |
| HB | .009 | |||
| Priority group 1 | 69 (44.5%) | 86 (55.5%) | 155 | |
| Priority group 2 | 13 (21.7%) | 47 (78.3%) | 60 | |
| Priority group 3 | 11 (45.8%) | 13 (54.2%) | 24 | |
| Priority group 4 | 1 (100.0%) | 0 (0.0%) | 1 |
| . | Genetic testing performed . | Genetic testing not yet performed . | Total, n (100%) . | P value . |
|---|---|---|---|---|
| HA | .213 | |||
| Severity in family | ||||
| Severe | 129 (39.3%) | 199 (60.7%) | 328 | |
| Moderate | 19 (28.8%) | 47 (71.2%) | 66 | |
| Mild | 93 (35.0%) | 173 (65.0%) | 266 | |
| HB | .001 | |||
| Severity in family | ||||
| Severe | 31 (32.6%) | 64 (67.4%) | 95 | |
| Moderate | 38 (59.4%) | 26 (40.6%) | 64 | |
| Mild | 25 (30.9%) | 56 (69.1%) | 81 | |
| HA | <.001 | |||
| Priority group 1 | 167 (43.0%) | 221 (57.0%) | 388 | |
| Priority group 2 | 43 (26.4%) | 120 (73.6%) | 163 | |
| Priority group 3 | 25 (30.9%) | 56 (69.1%) | 81 | |
| Priority group 4 | 1 (5.3%) | 18 (94.7%) | 19 | |
| HB | .009 | |||
| Priority group 1 | 69 (44.5%) | 86 (55.5%) | 155 | |
| Priority group 2 | 13 (21.7%) | 47 (78.3%) | 60 | |
| Priority group 3 | 11 (45.8%) | 13 (54.2%) | 24 | |
| Priority group 4 | 1 (100.0%) | 0 (0.0%) | 1 |
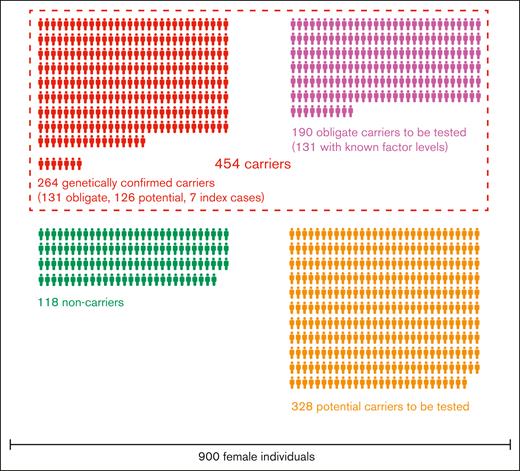
Diagnosis of carriers
Of 900 females, 454 (50.4%) were found to be obligate and/or genetically proven carriers of hemophilia (329 HA and 125 HB) and 118 could be identified as noncarriers (Figure 3). In 8 of these noncarriers, carriership was ruled out because of genetic testing results confirming noncarrier status in their mothers. Carrier status has been confirmed through genetic testing in 131 obligate carriers, 126 potential carriers, and 7 index cases. Genetic testing is yet to be conducted for 328 potential carriers and 190 obligate carriers.
Mean age at diagnosis of carriership or noncarriership of female individuals for whom this exact age could be determined was 30.7 years (range, 1-82) in families with HA and 30.1 years (range, 0.5-93) in families with HB (P = .809). In families with severe, moderate, and mild hemophilia, mean age at diagnosis of females was, respectively, 29.7 (range, 1.0-76.0), 29.6 (range, 0.5-77.0), and 32.1 years (range, 1.0-93.0) (P = .535). Mean age at diagnosis of females with a FVIII or FIX deficiency (lowest factor level <40 IU/dL) was 25.8 years (standard deviation, 18.4; range, 1.0-63.0) compared with 31.8 years (standard deviation, 19.1; range, 0.5-82.0) for those without a factor deficiency (P = .034). Given that the exact age at diagnosis could not be determined in the 2 females with severe hemophilia and there were no females with moderate hemophilia, the reported mean age at diagnosis of females with a factor deficiency equals the mean age at diagnosis of females with mild hemophilia in our cohort.
In families with HA, the proportion of female individuals who have had genetic testing was 39.3%, 28.8%, and 35.0% in families with severe, moderate, and mild hemophilia, respectively (P = .132). In families with HB, female individuals were more likely to be tested in families with moderate hemophilia (59.4%) than those with severe (32.6%) and mild hemophilia (30.9%) (P = .01); however, this difference can be attributed to the presence of 1 large family comprising 6 male persons with moderate HB and 22 female individuals, of whom most (n = 18, 82%) have had genetic testing.
The prevalence of genetic testing according to priority group is presented in Table 1.
Coagulation factor levels
Frequencies of different coagulation factor level ranges in carriers and noncarriers are shown in Table 2. Coagulation factor levels had been measured at least once in 57.5% of carriers. Among carriers with known factor levels, 23.0% (n = 42) and 29.5% of HA and HB carriers (n = 23), respectively, had a factor deficiency <40 IU/dL (P = .264), and 35.5 % (n = 65) and 41.0% (n = 32) had a factor level <50 IU/dL (P = .399). Carriers with a factor deficiency most often had mild hemophilia. One HA carrier and 1 HB carrier were regularly followed for severe hemophilia. One-third of HA carriers (33.3%) and approximately one-fourth of HB carriers (24.4%) had borderline factor levels, ranging between 40 and 60 IU/dL.
Mean minimum coagulation factor levels and frequencies of different coagulation factor level ranges in carriers and noncarriers
| . | HA carriers . | HA noncarriers . | Total . | P value . |
|---|---|---|---|---|
| FVIII minimum level | ||||
| Mean, IU/dL (SD) | 61.42 (28.20) | 117.93 (35.32) | <.001 | |
| <1 IU/dL, n (%) | 1 (0.5) | 0 (0.0) | 1 (0.4) | |
| 1-5 IU/dL, n (%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| 6-15 IU/dL, n (%) | 3 (1.6) | 0 (0.0) | 3 (1.3) | |
| 16-39 IU/dL, n (%) | 38 (20.8) | 0 (0.0) | 38 (15.8) | |
| 40-60 IU/dL, n (%) | 61 (33.3) | 1 (1.8) | 62 (25.8) | |
| ≥61 IU/dL, n (%) | 80 (43.7) | 56 (98.2) | 136 (56.7) | |
| Total, n | 183 | 57 | 240 | |
| VWF:Ag minimum level | ||||
| Mean, IU/dL (SD) | 111.19 (45.04) | 112.54 (38.10) | .853 | |
| VWF:RCo minimum level | ||||
| Mean, IU/dL (SD) | 107.80 (42.79) | 116.80 (44.56) | .221 |
| . | HA carriers . | HA noncarriers . | Total . | P value . |
|---|---|---|---|---|
| FVIII minimum level | ||||
| Mean, IU/dL (SD) | 61.42 (28.20) | 117.93 (35.32) | <.001 | |
| <1 IU/dL, n (%) | 1 (0.5) | 0 (0.0) | 1 (0.4) | |
| 1-5 IU/dL, n (%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| 6-15 IU/dL, n (%) | 3 (1.6) | 0 (0.0) | 3 (1.3) | |
| 16-39 IU/dL, n (%) | 38 (20.8) | 0 (0.0) | 38 (15.8) | |
| 40-60 IU/dL, n (%) | 61 (33.3) | 1 (1.8) | 62 (25.8) | |
| ≥61 IU/dL, n (%) | 80 (43.7) | 56 (98.2) | 136 (56.7) | |
| Total, n | 183 | 57 | 240 | |
| VWF:Ag minimum level | ||||
| Mean, IU/dL (SD) | 111.19 (45.04) | 112.54 (38.10) | .853 | |
| VWF:RCo minimum level | ||||
| Mean, IU/dL (SD) | 107.80 (42.79) | 116.80 (44.56) | .221 |
| . | HB carriers . | HB noncarriers . | Total . | P value . |
|---|---|---|---|---|
| FIX minimum level | ||||
| Mean, IU/dL (SD) | 59.36 (29.90) | 103.09 (30.40) | <.001 | |
| <1 IU/dL, n (%) | 1 (1.3) | 0 (0.0) | 1 (1.0) | |
| 1-5 IU/dL, n (%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| 6-15 IU/dL, n (%) | 1 (1.3) | 0 (0.0) | 1 (1.0) | |
| 16-39 IU/dL, n (%) | 21 (26.9) | 0 (0.0) | 21 (21.0) | |
| 40-60 IU/dL, n (%) | 19 (24.4) | 2 (9.1) | 21 (21.0) | |
| ≥61 IU/dL, n (%) | 36 (46.2) | 20 (90.9) | 56 (56.0) | |
| Total, n | 78 | 22 | 100 |
| . | HB carriers . | HB noncarriers . | Total . | P value . |
|---|---|---|---|---|
| FIX minimum level | ||||
| Mean, IU/dL (SD) | 59.36 (29.90) | 103.09 (30.40) | <.001 | |
| <1 IU/dL, n (%) | 1 (1.3) | 0 (0.0) | 1 (1.0) | |
| 1-5 IU/dL, n (%) | 0 (0.0) | 0 (0.0) | 0 (0.0) | |
| 6-15 IU/dL, n (%) | 1 (1.3) | 0 (0.0) | 1 (1.0) | |
| 16-39 IU/dL, n (%) | 21 (26.9) | 0 (0.0) | 21 (21.0) | |
| 40-60 IU/dL, n (%) | 19 (24.4) | 2 (9.1) | 21 (21.0) | |
| ≥61 IU/dL, n (%) | 36 (46.2) | 20 (90.9) | 56 (56.0) | |
| Total, n | 78 | 22 | 100 |
SD, standard deviation.
Mean minimum FVIII and FIX levels were significantly lower in carriers of HA and HB than in noncarriers (Table 2). No statistically significant difference was observed between the mean minimum FVIII level in HA carriers and the mean minimum FIX level in HB carriers (P = .597). Carriers of HA with blood group O had significantly lower FVIII, VWF:Ag, and VWF:RCo levels than carriers of HA with blood group non-O (Table 3). In both HA and HB carriers, the proportion of carriers with a factor level <40 IU/dL did not significantly differ between families with severe, moderate, and mild hemophilia (Table 4), neither did mean coagulation factor levels in carriers with a factor deficiency in these groups (26.2, 30.4, and 27.1 IU/dL in families with severe, moderate, and mild HA and HB, respectively; P = .344).
FVIII and VWF levels according to blood group O or non-O in carriers of HA
| HA carriers . | Blood group O . | Blood group non-O . | P value . |
|---|---|---|---|
| FVIII minimum level | n = 44 | n = 46 | |
| Mean, IU/dL (SD) | 49.07 (22.45) | 62.00 (24.88) | .011 |
| VWF:Ag minimum level | n = 40 | n = 37 | |
| Mean, IU/dL (SD) | 88.03 (32.50) | 118.38 (30.35) | <.001 |
| VWF:RCo minimum level | n = 40 | n = 36 | |
| Mean, IU/dL (SD) | 84.40 (32.40) | 117.72 (37.58) | <.001 |
| HA carriers . | Blood group O . | Blood group non-O . | P value . |
|---|---|---|---|
| FVIII minimum level | n = 44 | n = 46 | |
| Mean, IU/dL (SD) | 49.07 (22.45) | 62.00 (24.88) | .011 |
| VWF:Ag minimum level | n = 40 | n = 37 | |
| Mean, IU/dL (SD) | 88.03 (32.50) | 118.38 (30.35) | <.001 |
| VWF:RCo minimum level | n = 40 | n = 36 | |
| Mean, IU/dL (SD) | 84.40 (32.40) | 117.72 (37.58) | <.001 |
Prevalence of coagulation factor deficiency and low coagulation factor levels according to hemophilia type and severity
| . | HA . | HB . | P value . |
|---|---|---|---|
| Minimum factor level, <40 IU/dL | |||
| Severity in family | |||
| Carriers | 42/183 (23.0%) | 23/78 (29.5%) | |
| Severe | 20/97 (20.6%) | 8/27 (29.6%) | |
| Moderate | 5/18 (27.8%) | 12/31 (38.7%) | |
| Mild | 17/68 (25.0%) | 3/20 (15.0%) | |
| P = .706 | P = .193 | ||
| Noncarriers | 0/57 (0.0%) | 0/22 (0.0%) | |
| P value | <.001 | .004 | .264 |
| Minimum factor level, <50 IU/dL | |||
| Severity in family | |||
| Carriers | 65/183 (35.5%) | 32/78 (41.0%) | |
| Severe | 34/97 (35.1%) | 11/27 (40.7%) | |
| Moderate | 7/18 (38.9%) | 15/31 (48.4%) | |
| Mild | 24/68 (35.3%) | 6/20 (30.0%) | |
| P = .951 | P = .427 | ||
| Noncarriers | 1/57 (1.8%) | 1/22 (4.5%) | |
| P value | <.001 | .001 | .399 |
| . | HA . | HB . | P value . |
|---|---|---|---|
| Minimum factor level, <40 IU/dL | |||
| Severity in family | |||
| Carriers | 42/183 (23.0%) | 23/78 (29.5%) | |
| Severe | 20/97 (20.6%) | 8/27 (29.6%) | |
| Moderate | 5/18 (27.8%) | 12/31 (38.7%) | |
| Mild | 17/68 (25.0%) | 3/20 (15.0%) | |
| P = .706 | P = .193 | ||
| Noncarriers | 0/57 (0.0%) | 0/22 (0.0%) | |
| P value | <.001 | .004 | .264 |
| Minimum factor level, <50 IU/dL | |||
| Severity in family | |||
| Carriers | 65/183 (35.5%) | 32/78 (41.0%) | |
| Severe | 34/97 (35.1%) | 11/27 (40.7%) | |
| Moderate | 7/18 (38.9%) | 15/31 (48.4%) | |
| Mild | 24/68 (35.3%) | 6/20 (30.0%) | |
| P = .951 | P = .427 | ||
| Noncarriers | 1/57 (1.8%) | 1/22 (4.5%) | |
| P value | <.001 | .001 | .399 |
Bleeding symptoms
Relative risks of different bleeding symptoms in HA and HB carriers according to minimum coagulation factor levels are presented in Table 5. Heavy menstrual bleeding (HMB) was the most frequent bleeding symptom in both adult HA and adult HB carriers, affecting 30.5% and 28.7% of them, respectively (P = .200). Carriers of HA with a factor deficiency had a >2-fold risk of experiencing HMB than noncarriers of HA (risk ratio [RR], 2.39; 95% confidence interval [CI], 1.46-3.92) and a twofold risk compared with HA carriers with normal FVIII levels (RR, 1.96; 95% CI, 1.12-3.42). Carriers of HA with borderline factor levels had an increased risk of HMB (n = 20, 41.7%) compared with noncarriers (n = 7, 20.0 %; P = .037; RR, 1.48; 95% CI, 1.05-2.09), but were not found to have an increased risk compared with HA carriers with normal levels (P = .626; RR, 1.11; 95% CI, 0.73-1.71). Although HA carriers with a FVIII deficiency experienced HMB more often than those with borderline factor levels, this difference was not statistically significant (P = .057).
Bleeding symptoms in HA and HB carriers according to minimum coagulation factor levels
| . | FVIII level . | FIX level . | ||||
|---|---|---|---|---|---|---|
| <40 IU/dL . | 40-60 IU/dL . | >60 IU/dL . | <40 IU/dL . | 40-60 IU/dL . | >60 IU/dL . | |
| HMB∗ | ||||||
| Frequency, n (%) | 22/35 (62.9) | 20/48 (41.7) | 23/62 (37.1) | 8/18 (44.4) | 5/16 (31.3) | 10/29 (34.5) |
| RR (95% CI) | 1.96 (1.12-3.42) | 1.11 (0.73-1.71) | 1 | 1.29 (0.63-2.65) | 0.91 (0.39-2.14) | 1 |
| RTB∗,† | ||||||
| Frequency, n (%) | 2/35 (5.7) | 5/48 (10.4) | 7/62 (11.3) | 7/18 (38.9) | 2/16 (12.5) | 3/29 (10.3) |
| RR (95% CI) | 0.59 (0.17-2.07) | 0.95 (0.47-1.92) | 1 | 2.36 (1.24-4.47) | 1.14 (0.36-3.62) | 1 |
| Easy bruising | ||||||
| Frequency, n (%) | 16/38 (42.1) | 20/50 (40.0) | 17/66 (25.8) | 5/22 (22.7) | 3/18 (16.7) | 6/32 (18.8) |
| RR (95% CI) | 1.57 (0.96-2.57) | 1.42 (0.95-2.14) | 1 | 1.15 (0.55-2.42) | 0.91 (0.33-2.50) | 1 |
| Epistaxis | ||||||
| Frequency, n (%) | 8/38 (21.1) | 11/50 (22.0) | 7/66 (10.6) | 3/22 (13.6) | 2/18 (11.1) | 4/32 (12.5) |
| RR (95% CI) | 1.58 (0.91-2.76) | 1.54 (0.99-2.39) | 1 | 1.06 (0.42-2.67) | 0.92 (0.28-3.04) | 1 |
| Hematomas | ||||||
| Frequency, n (%) | 4/38 (10.5) | 2/50 (4.0) | 1/66 (1.5) | 2/22 (9.1) | 0/18 (0.0) | 1/32 (3.1) |
| RR (95% CI) | 2.33 (1.39-3.91) | 1.57 (0.69-3.60) | 1 | 1.70 (0.71-4.06) | — | 1 |
| Bleeding after dental procedures | ||||||
| Frequency, n (%) | 5/38 (13.2) | 2/50 (4.0) | 5/66 (7.6) | 5/22 (22.7) | 0/18 (0.0) | 2/32 (6.3) |
| RR (95% CI) | 1.42 (0.72-2.81) | 0.65 (0.20-2.13) | 1 | 1.98 (1.08-3.61) | — | 1 |
| Perioperative bleeding | ||||||
| Frequency, n (%) | 5/38 (13.2) | 2/50 (4.0) | 8/66 (12.1) | 5/22 (22.7) | 1/18 (5.6) | 2/32 (6.3) |
| RR (95% CI) | 1.06 (0.51-2.22) | 0.44 (0.13-1.55) | 1 | 1.98 (1.08-3.61) | 0.92 (0.18-4.77) | 1 |
| Mucosal bleeding | ||||||
| Frequency, n (%) | 5/38 (13.2) | 10/50 (20.0) | 5/66 (7.6) | 2/22 (9.1) | 1/18 (5.6) | 3/32 (9.4) |
| RR (95% CI) | 1.42 (0.72-2.81) | 1.68 (1.10-2.59) | 1 | 0.98 (0.32-3.02) | 0.68 (0.12-3.85) | 1 |
| Bleeding requiring transfusion | ||||||
| Frequency, n (%) | 0/38 (0.0) | 0/50 (0.0) | 6/66 (9.1) | 3/22 (13.6) | 1/18 (5.6) | 0/32 (0.0) |
| RR (95% CI) | — | — | 1 | 2.68 (1.88-3.83) | 2.88 (1.96-4.23) | 1 |
| Abnormal bleeding after trauma | ||||||
| Frequency, n (%) | 5/38 (13.2) | 2/50 (4.0) | 2/66 (3.0) | 2/22 (9.1) | 0/18 (0.0) | 0/32 (0.0) |
| RR (95% CI) | 2.10 (1.22-3.62) | 1.17 (0.43-3.18) | 1 | 2.60 (1.84-3.67) | — | 1 |
| Hemarthrosis | ||||||
| Frequency, n (%) | 4/38 (10.5) | 0/50 (0.0) | 0/66 (0.0) | 1/22 (4.5) | 0/18 (0.0) | 0/32 (0.0) |
| RR (95% CI) | 2.94 (2.24-3.87) | — | 1 | 2.52 (1.81-3.52) | — | 1 |
| Other bleeding | ||||||
| Frequency, n (%) | 1/38 (2.6) | 0/50 (0.0) | 0/66 (0.0) | 0/22 (0.0) | 0/18 (0.0) | 0/32 (0.0) |
| RR (95% CI) | 2.78 (2.15-3.60) | — | 1 | — | — | 1 |
| Anemia | ||||||
| Frequency, n (%) | 9/38 (23.7) | 3/50 (6.0) | 3/66 (4.5) | 4/22 (18.2) | 4/18 (22.2) | 1/32 (3.1) |
| RR (95% CI) | 2.38 (1.53-3.71) | 1.17 (0.51-2.68) | 1 | 2.18 (1.23-3.86) | 2.57 (1.39-4.77) | 1 |
| Iron deficiency | ||||||
| Frequency, n (%) | 10/38 (26.3) | 4/50 (8.0) | 4/66 (6.1) | 3/22 (13.6) | 2/18 (11.1) | 0/32 (0.0) |
| RR (95% CI) | 2.30 (1.46-3.61) | 1.17 (0.57-2.43) | 1 | 2.68 (1.88-3.83) | 3.00 (2.01-4.48) | 1 |
| . | FVIII level . | FIX level . | ||||
|---|---|---|---|---|---|---|
| <40 IU/dL . | 40-60 IU/dL . | >60 IU/dL . | <40 IU/dL . | 40-60 IU/dL . | >60 IU/dL . | |
| HMB∗ | ||||||
| Frequency, n (%) | 22/35 (62.9) | 20/48 (41.7) | 23/62 (37.1) | 8/18 (44.4) | 5/16 (31.3) | 10/29 (34.5) |
| RR (95% CI) | 1.96 (1.12-3.42) | 1.11 (0.73-1.71) | 1 | 1.29 (0.63-2.65) | 0.91 (0.39-2.14) | 1 |
| RTB∗,† | ||||||
| Frequency, n (%) | 2/35 (5.7) | 5/48 (10.4) | 7/62 (11.3) | 7/18 (38.9) | 2/16 (12.5) | 3/29 (10.3) |
| RR (95% CI) | 0.59 (0.17-2.07) | 0.95 (0.47-1.92) | 1 | 2.36 (1.24-4.47) | 1.14 (0.36-3.62) | 1 |
| Easy bruising | ||||||
| Frequency, n (%) | 16/38 (42.1) | 20/50 (40.0) | 17/66 (25.8) | 5/22 (22.7) | 3/18 (16.7) | 6/32 (18.8) |
| RR (95% CI) | 1.57 (0.96-2.57) | 1.42 (0.95-2.14) | 1 | 1.15 (0.55-2.42) | 0.91 (0.33-2.50) | 1 |
| Epistaxis | ||||||
| Frequency, n (%) | 8/38 (21.1) | 11/50 (22.0) | 7/66 (10.6) | 3/22 (13.6) | 2/18 (11.1) | 4/32 (12.5) |
| RR (95% CI) | 1.58 (0.91-2.76) | 1.54 (0.99-2.39) | 1 | 1.06 (0.42-2.67) | 0.92 (0.28-3.04) | 1 |
| Hematomas | ||||||
| Frequency, n (%) | 4/38 (10.5) | 2/50 (4.0) | 1/66 (1.5) | 2/22 (9.1) | 0/18 (0.0) | 1/32 (3.1) |
| RR (95% CI) | 2.33 (1.39-3.91) | 1.57 (0.69-3.60) | 1 | 1.70 (0.71-4.06) | — | 1 |
| Bleeding after dental procedures | ||||||
| Frequency, n (%) | 5/38 (13.2) | 2/50 (4.0) | 5/66 (7.6) | 5/22 (22.7) | 0/18 (0.0) | 2/32 (6.3) |
| RR (95% CI) | 1.42 (0.72-2.81) | 0.65 (0.20-2.13) | 1 | 1.98 (1.08-3.61) | — | 1 |
| Perioperative bleeding | ||||||
| Frequency, n (%) | 5/38 (13.2) | 2/50 (4.0) | 8/66 (12.1) | 5/22 (22.7) | 1/18 (5.6) | 2/32 (6.3) |
| RR (95% CI) | 1.06 (0.51-2.22) | 0.44 (0.13-1.55) | 1 | 1.98 (1.08-3.61) | 0.92 (0.18-4.77) | 1 |
| Mucosal bleeding | ||||||
| Frequency, n (%) | 5/38 (13.2) | 10/50 (20.0) | 5/66 (7.6) | 2/22 (9.1) | 1/18 (5.6) | 3/32 (9.4) |
| RR (95% CI) | 1.42 (0.72-2.81) | 1.68 (1.10-2.59) | 1 | 0.98 (0.32-3.02) | 0.68 (0.12-3.85) | 1 |
| Bleeding requiring transfusion | ||||||
| Frequency, n (%) | 0/38 (0.0) | 0/50 (0.0) | 6/66 (9.1) | 3/22 (13.6) | 1/18 (5.6) | 0/32 (0.0) |
| RR (95% CI) | — | — | 1 | 2.68 (1.88-3.83) | 2.88 (1.96-4.23) | 1 |
| Abnormal bleeding after trauma | ||||||
| Frequency, n (%) | 5/38 (13.2) | 2/50 (4.0) | 2/66 (3.0) | 2/22 (9.1) | 0/18 (0.0) | 0/32 (0.0) |
| RR (95% CI) | 2.10 (1.22-3.62) | 1.17 (0.43-3.18) | 1 | 2.60 (1.84-3.67) | — | 1 |
| Hemarthrosis | ||||||
| Frequency, n (%) | 4/38 (10.5) | 0/50 (0.0) | 0/66 (0.0) | 1/22 (4.5) | 0/18 (0.0) | 0/32 (0.0) |
| RR (95% CI) | 2.94 (2.24-3.87) | — | 1 | 2.52 (1.81-3.52) | — | 1 |
| Other bleeding | ||||||
| Frequency, n (%) | 1/38 (2.6) | 0/50 (0.0) | 0/66 (0.0) | 0/22 (0.0) | 0/18 (0.0) | 0/32 (0.0) |
| RR (95% CI) | 2.78 (2.15-3.60) | — | 1 | — | — | 1 |
| Anemia | ||||||
| Frequency, n (%) | 9/38 (23.7) | 3/50 (6.0) | 3/66 (4.5) | 4/22 (18.2) | 4/18 (22.2) | 1/32 (3.1) |
| RR (95% CI) | 2.38 (1.53-3.71) | 1.17 (0.51-2.68) | 1 | 2.18 (1.23-3.86) | 2.57 (1.39-4.77) | 1 |
| Iron deficiency | ||||||
| Frequency, n (%) | 10/38 (26.3) | 4/50 (8.0) | 4/66 (6.1) | 3/22 (13.6) | 2/18 (11.1) | 0/32 (0.0) |
| RR (95% CI) | 2.30 (1.46-3.61) | 1.17 (0.57-2.43) | 1 | 2.68 (1.88-3.83) | 3.00 (2.01-4.48) | 1 |
In women ≥18 years old.
Other than HMB.
Carriers of HB with a FIX deficiency experienced HMB more often (n = 8, 44.4%) than noncarriers of HB (n = 4, 28.6%) (RR, 1.33; 95% CI, 0.74-2.41) and carriers of HB with normal factor levels (n = 10, 34.5%; RR, 1.29; 95% CI, 0.63-2.65), yet these differences were not statistically significant (P = .358 and P = .495, respectively). There was also no significant difference regarding occurrence of HMB in carriers of HB with borderline FIX levels (n = 5, 31.3%) compared with noncarriers of HB (n = 4, 28.6%; P = 1.000; RR, 1.33; 95% CI, 0.737-2.41) or carriers of HB with normal factor levels (P = .826; RR, 0.91; 95% CI, 0.39-2.14). The observed difference in frequency of HMB between carriers of HB with a FIX deficiency and those with borderline factor levels was not statistically significant (P = .429).
Overall, carriers with blood group O had a higher rate of HMB than carriers with non-O blood groups (55.6% vs 29.1%; P = .005) and a higher relative risk of HMB (RR, 1.7; 95% CI, 1.2-2.5). Among carriers of HA, the difference in HMB frequency (51.2% vs 32.5%; P = .085) and RR (1.4; 95% CI, 1.0-2.2) did not reach statistical significance. However, carriers of HB with blood group O experienced HMB significantly more frequently than those with non-O blood groups (72.7% vs 20.0%; P = .007; RR, 3.6; 95% CI, 1.2-10.7).
Among adult carriers with a factor deficiency, reproductive tract bleeding (RTB) other than HMB (RTB) (mostly postpartum hemorrhage [PPH], 19/27 [70.4%]) was significantly more frequent in adult HB carriers than in adult HA carriers (P = .002). In adult HA carriers with a factor deficiency, the proportion of carriers affected by RTB was exactly the same (n = 2, 5.7%) as in noncarriers of HA (n = 2, 5.7%) (P = 1.000) and lower than in HA carriers with normal FVIII levels (n = 7, 11.3%) (P = .363). In adult HA carriers with borderline FVIII levels, the proportion of carriers with RTB was higher (n = 5, 10.4%) than in noncarriers (P = .693) and was lower than in HA carriers with normal FVIII levels (P = .884), although not significantly in both cases. Adult HB carriers with a FIX deficiency had a >2-fold risk of RTB compared with HB carriers with normal FIX levels (RR, 2.36; 95% CI, 1.24-4.47). In adult HB carriers with borderline FIX levels, RTB did not occur significantly more often (n = 2, 12.5%) than in noncarriers of HB (n = 1, 7.1%; P = 1.000) or HB carriers with normal FIX levels (n = 3, 10.3%; P = 1.000). Although RTB was more frequent in HB carriers with a FIX deficiency than those with borderline FIX levels, this difference was not statistically significant (P = .125), possibly owing to the limited number of observations.
Easy bruising was more frequent in HA carriers with a factor deficiency (n = 16, 42.1%) than in HB carriers with a factor deficiency (n = 5, 22.7%), yet this difference was not statistically significant (P = .129). Both HA and HB carriers with a factor deficiency did not experience easy bruising significantly more often than noncarriers (P = .147 and P = .419, respectively). Similar frequencies of easy bruising were observed between HA carriers with a FVIII deficiency and those with borderline FVIII levels (P = .842), as well as between HB carriers with a FIX deficiency and those with borderline FIX levels (P = .790).
Epistaxis was more frequent in HA carriers with a FVIII deficiency (n = 8, 21.1%) than in HB carriers with a FIX deficiency (n = 3, 13.6%), although not significantly (P = .474). HA carriers with a FVIII deficiency had an increased risk of epistaxis compared with those with normal FVIII levels (RR, 1.58; 95% CI, 0.91-2.76), yet this was not statistically significant (P = .144). In HB carriers, the frequency of epistaxis was similar between those with a FIX deficiency and those with normal FIX levels (RR, 1.06; 95% CI, 0.42-2.67; P = 1.000). In addition, there were similar frequencies of epistaxis observed between HA carriers with a FVIII deficiency and those with borderline FVIII levels (P = .915), as well as between HB carriers with a FIX deficiency and those with borderline FIX levels (P = 1.000).
HA carriers with a FVIII deficiency had a more than twofold risk of developing anemia (RR, 2.38; 95% CI, 1.53-3.71) and iron deficiency (RR, 2.30; 95% CI, 1.46-3.61) compared with HA carriers with normal factor levels. Similar figures were observed in HB carriers, with an RR for anemia of 2.18 (95% CI, 1.23-3.86) and an RR for iron deficiency of 2.69 (95% CI, 1.88-3.83) compared with HB carriers with normal factor levels. HA carriers who experienced HMB had a 3-fold risk of being anemic (RR, 3.13; 95% CI, 1.03-9.55) compared with those who did not experience HMB. Such an increased risk could not be demonstrated for HB carriers (RR, 1.19; 95% CI, 0.37-3.78).
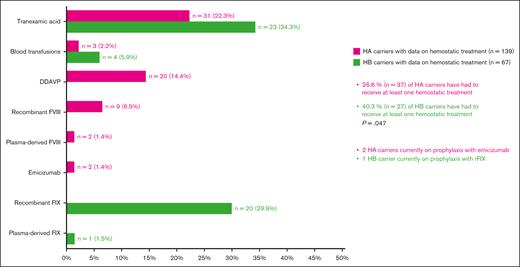
Hemostatic treatment
In carriers for whom information on hemostatic treatment use was available, 26.6% of HA carriers (n = 37) and 40.3% of HB carriers (n = 27) (P = .047) have had to receive a hemostatic treatment at least once in their lifetime at the time of the study. The most frequently used agent in both HA and HB carriers was tranexamic acid, used in 22.3% (n = 31) and 34.3% (n = 23), respectively (P = .066; Figure 4). The second most-used agent was Desmopressin (DDAVP) (14.4%, n = 20) in HA carriers and recombinant FIX products (29.9%, n = 20) in HB carriers. In HA carriers, coagulation factor replacement products were less commonly used, explained by the fact that DDAVP is available as an alternative in these patients. Two HA carriers were treated with regular emicizumab prophylaxis, and 1 HB carrier was on regular prophylaxis with an extended half-life recombinant FIX product.
Hemostatic treatments administered at least once in carriers.
Hemostatic treatments administered at least once in carriers.
Discussion
Establishing and regularly updating family pedigrees of PWHs are a fundamental yet often underutilized clinical practice in bleeding disorder care and mark the initial stride toward ending gender disparities in hemophilia care. Its primary goal is to ensure that all female and male relatives of PWHs, even the more distant ones in the pedigree, receive timely diagnosis and appropriate bleeding prophylaxis. Although the establishment of family pedigrees for genetic counseling and testing purposes figures in the 2020 WFH guidelines for the management of hemophilia and multiple reports of carrier diagnosis in PWHs’ families do exist,22,26-34 concrete strategies for systematic carrier screening, aiming to screen all potential and obligate carriers genetically linked to a PWH, have not yet been described. Moreover, to the best of our knowledge, such reports are also absent for other X-linked recessive disorders, such as Duchenne and Becker muscular dystrophies, adrenoleukodystrophy, or X-linked retinal diseases.
In a survey of 150 carriers of different X-linked disorders by Choi et al, most participants (54%) declared that they had been diagnosed as a carrier only after giving birth to an affected boy.35 This finding might seem logical if all carriers were entirely asymptomatic. However, cases of symptomatic carriers of X-linked disorders have been described and may be more frequent than expected.36 Symptomatic hemophilia carriers and WGH may go undiagnosed because their abnormal bleeding symptoms are overlooked or mistaken as normal, especially in families in which HMB is common among women carrying hemophilia.37,38
This study represents the first attempt to comprehensively identify all carriers and potential carriers in a HTC’s patient cohort and to reach out to unscreened individuals. It allowed us to obtain a precise inventory of known carriers, potential carriers yet to be tested and noncarriers in our HA and HB patient cohort. It revealed that at least more than half of the 900 female individuals within our cohort were carriers. However, a significant number of potential carriers (328; as depicted in Figure 3) have yet to undergo genetic testing. In addition, 59 obligate carriers have not had their factor levels tested. These statistics underscore the challenges of comprehensively screening all female relatives, despite our proactive efforts.
Several factors contributed to the difficulty in reaching PWHs’ relatives for testing. First, some undiagnosed potential carriers fell into age brackets that were excluded from the prospective arm of our study: among undiagnosed potential carriers with known age, 8.1% (6/74) were aged <12 years, whereas 14.9% (11/74) were aged >75 years. Furthermore, given the cosmopolitan nature of Brussels, where our HTC is located, it is unsurprising that at least 64 female individuals resided abroad, making outreach and obtaining testing results more complex. Moreover, our study started during the COVID-19 pandemic, which further complicated matters by making nonurgent hospital visits less feasible and appealing for potential participants. It also made the organization of patient information events impossible. These events, which had been regularly held before the pandemic, would have provided a valuable opportunity to explain the rationale behind carrier screening to PWHs and their female relatives during face-to-face meetings. They would have also facilitated the exchange of experiences among symptomatic carriers and WGH.
The success of any carrier screening initiative relies significantly on the awareness and proactivity of hematologists, as well as the motivation and health literacy of the probands. These probands act as intermediaries between their relatives and health care professionals during the initial contact. Unfortunately, various factors can disrupt this communication channel, including family conflicts and the stigma surrounding PWHs, as well as stigma surrounding menstruation and reproduction within certain families or cultures.39,40 In our study, we provided verbal information about the implications of hemophilia carriership, as well as written materials in the form of informational brochures. However, we faced a challenge in monitoring whether and how effectively this information was relayed to the female relatives. It is noteworthy that, before the commencement of the study, repeatedly raising awareness among male PWHs about the importance of carrier screening was already part of the clinical routine at our HTC. An additional explanation for why many female relatives of PWHs remain unscreened, despite proactive efforts by hematologists, may be that the most motivated and health-literate relatives of probands have likely already been screened. Those remaining unscreened may be harder to reach or motivate to attend the clinic. Furthermore, we hypothesize that individuals with abnormal bleeding are more likely to seek specialized care or respond to clinic invitations than those who are asymptomatic, leading to a certain selection bias when reporting bleeding symptoms in a population of female relatives of PWHs.
In addition to screening the highest possible number of potential carriers in our cohort, our study’s second objective was to compare carriers of HA and HB in various aspects. We observed similarities in the circumstances of diagnosis, with both groups having a similar proportion of carriers having had genetic testing and an average age at diagnosis of around 30 years. Within our cohort, female individuals with mild hemophilia were diagnosed, on average, 7 years later than their male counterparts with mild hemophilia (mean age at diagnosis of 18.2 years), highlighting the diagnostic delays frequently experienced by women with bleeding disorders. Considering the significant implications of carrier status for family planning, there is evidently a need for earlier detection of carriers. The ideal timing of genetic testing is debated and influenced by local legal frameworks, especially regarding testing minors.41,42 Authors of the European principles of care for women and girls with inherited bleeding disorders advise to perform genetic testing in adolescence or early adulthood and in certain cases it may be envisaged in children.21 Ideally, the genetic status should be known before pregnancy to enable informed reproductive choices.41,43,44 Today, hemophilia carriers have various reproductive choices, including preimplantation and prenatal diagnostics. These options empower them to make informed decisions regarding pregnancies, enabling them to prevent or choose to terminate a pregnancy if it is found that the child may have hemophilia or to simply be prepared for precautionary measures that will be taken during delivery and for a life with a child with hemophilia.
Our findings regarding mean coagulation factor levels in carriers vs noncarriers are in line with central tendency measures of coagulation factor levels previously reported in the literature for both groups.26,34,45-49 The correlation between the severity of hemophilia in a family and the coagulation factor levels in HA and HB carriers remains uncertain. At this time, the prevailing evidence suggests that there is more support for the absence of such a correlation,26,47,50-52 as observed in our cohort, rather than its existence.53 There were no significant differences in the proportion of carriers with a factor deficiency and in mean coagulation factor levels between HA and HB carriers. As in a previous report by James et al,54 HMB was the most frequently reported bleeding symptom experienced by HA and HB carriers, without a significant difference in occurrence in both groups. The incidence of HMB noted within our cohort of HA carriers with a factor deficiency closely aligns with findings reported by Plug et al45 in carriers (both HA and HB, predominantly HA) with a deficiency. Furthermore, compared with the Dutch cohort from 2006, we identified a comparable relative risk of anemia and iron deficiency among carriers with a factor deficiency in contrast to carriers exhibiting normal levels.45
It is interesting to note that RTB/PPH was significantly more frequent in HB carriers, although absolute numbers were low. This discrepancy between HA and HB carriers might be attributed to the fact that, unlike in HA carriers in whom FVIII levels physiologically rise during pregnancy owing to hormonal changes, FIX levels in HB carriers do not show a similar increase, potentially rendering HB carriers more vulnerable to PPH without adequate hemostatic cover. Given the low number of carriers in our cohort who experienced hemarthrosis, it is difficult to make assumptions about possible differences between HA and HB carriers. Nevertheless, it is important to acknowledge the possibility of underrecognized joint microbleeds and damage in carriers, underscoring the need for further research attention to musculoskeletal issues.37,55,56 In general, future research should gather more detailed data on bleeding symptoms and treatment of bleeding episodes in hemophilia carriers, as well as on the bleeding phenotypes of carriers with borderline factor levels.
As emphasized by Gregory et al in 2007,39 ongoing screening efforts regarding hemophilia carriers and WGH are crucial, particularly amidst the diminishing frequency and shortening of patient-health care professional interactions thanks to novel therapeutics for hemophilia. The imperative to continually update pedigrees remains essential, given that even groundbreaking treatments such as gene therapy do not alter the hereditary nature of hemophilia. In addition, the transition of PWHs from pediatric to adult care marks a vulnerable phase during which keeping track of the patient's relatives becomes challenging.41 Furthermore, girls who underwent coagulation factor level assessments during childhood still require genetic testing later in life and should not be overlooked.41 Identified carriers, especially those experiencing abnormal bleeding, should benefit from regular follow-up at the HTC.
To conclude, this study, to our knowledge, represents the first reported initiative to systematically identify and screen (potential) hemophilia carriers among families of all PWHs followed at a single HTC. We have gained new insights into practical aspects of carrier diagnostics, while also identifying persistent challenges in providing comprehensive screening to relatives of PWHs. Initiatives similar to our study should be replicated by other HTCs internationally, given that they would represent a crucial step toward ensuring equitable access to hemophilia diagnosis and care for all potentially affected individuals, regardless of sex and gender.
Limitations
The main limitation of our study lies in the mostly retrospective nature of our data. Bleeding and hemostatic treatment data were coded as binary variables and no data on specific bleeding or treatment episodes were collected. Abnormal bleeding data were aggregated from patient-reported bleeding symptoms rather than using bleeding scores such as the International Society on Thrombosis and Haemostasis Bleeding Assessment Tool. Moreover, as mentioned earlier, we assume that individuals experiencing abnormal bleeding are more likely to seek specialized medical care, leading to selection bias in the reporting of bleeding symptom frequency in female relatives of PWHs. Only the lowest coagulation factor levels of each individual were considered for the analysis, and no adjustment was made for use of estrogen and/or progesterone treatments for contraceptive or substitutive purposes and for age. Coagulation factor levels measured during pregnancy were not taken into account. Establishing family pedigrees heavily relies on patient reports, and a certain degree of imprecision, particularly in large families, cannot be entirely eliminated.
Acknowledgments
The authors thank all study participants and persons with hemophilia who helped the investigators reach out to their family members.
This project was partially funded by research grants from Swedish Orphan Biovitrum and CSL Behring.
Authorship
Contribution: E.K. contributed as coinvestigator of the study, analyzed data, conceptualized the manuscript and figures, wrote the manuscript, and designed the figures; C.L. and A.V.D. contributed as coinvestigator of the study and critically reviewed the manuscript and figures; and C.H. designed the study, served as principal investigator of the study, conceptualized the manuscript and figures, and critically reviewed the manuscript and figures.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Cedric Hermans, Division of Hematology, Hemostasis and Thrombosis Unit, Hemophilia Clinic, Cliniques universitaires Saint-Luc, Université catholique de Louvain (UCLouvain), 10 Avenue Hippocrate, Brussels 1200, Belgium; email: cedric.hermans@saintluc.uclouvain.be.
References
Author notes
Presented in abstract form at the 65th annual meeting of the American Society of Hematology in San Diego, CA, 9 December 2023. https://doi.org/10.1182/blood-2023-185067
The data are not publicly available owing to privacy or ethical restrictions. The deidentified data supporting the findings of this study are available on request from the corresponding author, Cedric Hermans (cedric.hermans@saintluc.uclouvain.be).