Key Points
In relapsed T-NHL, response to salvage chemotherapy is poor with only a minority of patients proceeding to SCT.
Risk of second relapse is half for patients treated with BV compared with chemotherapy, independent of histological subtype.
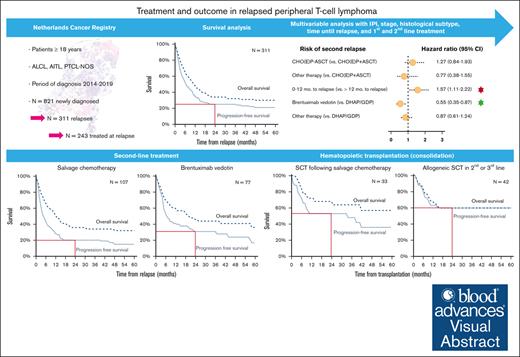
Visual Abstract
Optimal treatment in patients with refractory or relapsed peripheral T-cell lymphomas (R/R T-NHLs) is unknown. In this population-based study, outcomes in R/R peripheral T-cell lymphoma not otherwise specified (PTCL NOS), angioimmunoblastic T-cell lymphoma (AITL), and anaplastic lymphoma kinase-positive (ALK+) and ALK-negative (ALK–) anaplastic large cell lymphoma (ALCL) were evaluated. Patients with PTCL NOS, AITL, ALK+ ALCL, and ALK– ALCL (≥18 years) diagnosed in 2014 to 2019 were identified using the Netherlands Cancer Registry. End points were overall response rate (ORR), progression-free survival (PFS), and overall survival (OS). The 2-year PFS of 821 patients was 57%. Among 311 patients with a relapse, 243 received second-line treatment: 44% received salvage chemotherapy, 20% received brentuximab vedotin (BV), and 36% received other treatment. In third-line treatment, BV was most commonly used (38%). ORR after second-line treatment was 47%. Two-year PFS and OS after relapse were 25% and 34%, respectively. The risk of second relapse was negatively affected by early relapse (<12 months after diagnosis), whereas BV reduced this risk compared with salvage chemotherapy. Reduced risk of relapse was independent of histological subtype. The best outcomes were observed for patients treated with salvage chemotherapy receiving consolidative autologous and allogeneic stem cell transplantation (SCT) (2-year OS 68%), patients treated with BV achieving a second complete remission (2-year OS 74%) and patients with allogeneic SCT (2-year OS 60%). The risk of second relapse was significantly lower for patients with R/R T-NHL treated with BV compared with patients treated with salvage chemotherapy, and this was irrespective of subtype. Therefore, the use of salvage chemotherapy for patients with R/R T-NHL is challenged.
Introduction
The peripheral T-cell lymphomas (T-NHLs) comprise a heterogeneous group of mature T- and NK-cell neoplasms. In the Netherlands, peripheral T-cell lymphoma not otherwise specified (PTCL NOS), angioimmunoblastic T-cell lymphoma (AITL), and anaplastic large cell lymphoma (ALCL) are the most common diagnoses, with an annual incidence of 1.14 per 100 000 individuals.1
First-line treatment of PTCL NOS, AITL, and ALCL consists of CHOP (cyclophosphamide-doxorubicin-vincristine-prednisolone). In some countries, the addition of etoposide to CHOP is preferred, especially for patients with anaplastic lymphoma kinase-positive (ALK+) ALCL.2 In patients with ALCL, brentuximab vedotin (BV) in combination with cyclophosphamide-doxorubicin-prednisone (CHP) showed a superior outcome than CHOP; however, a comparison between BV-CHP and CHOEP (cyclophosphamide, doxorubicin, vincristine, prednisone, and etoposide) is lacking.3 In younger, fit patients with responsive disease to first-line treatment, consolidative autologous hematopoietic stem cell transplantation (ASCT) may be considered.4 However, it is worth noting that the widespread application of this approach has only recently been emphasized. The decrease in relapse rate after consolidation with allogeneic hematopoietic stem cell transplantation (allogeneic SCT) in first-line treatment is offset by an increase in treatment-related mortality.5
Despite initial responses to induction therapy, a significant proportion of patients experience relapse or refractory (R/R) disease. Historically, the outcome of patients with R/R T-NHL has been poor, with modest response rates after therapy with chemotherapy, small molecules, and checkpoint inhibitors.6-11 Rates for complete remission are low, and the duration limited. In a few patients, salvage chemotherapy, histone deacetylase inhibitors (HDACi),12,13 BV,14,15 and allogeneic transplantation offer curative treatment options.16,17 In the Netherlands, BV has been available since 2013 and implemented in second-line treatment of ALCL and other CD30+ lymphomas, including PTCL NOS and AITL. Despite favorable results in selected R/R patients in clinical trials, the impact of these novel strategies on outcome for all R/R patients is unknown.
In this contemporary nationwide population-based study, treatment strategies and their impact on outcome among patients with relapsed PTCL NOS, AITL, and ALK+ and anaplastic lymphoma kinase-negative (ALK–) ALCL are evaluated.
Materials and methods
Netherlands Cancer Registry
The nationwide population-based the Netherlands Cancer Registry (NCR) is maintained and hosted by the Netherlands Comprehensive Cancer Organization and has nationwide coverage of at least 95% of all malignancies since 1989. The NCR relies on comprehensive case notification through the Nationwide Histopathology and Cytopathology Data Network and the Nationwide Registry of Hospital Discharges (ie, inpatient and outpatient discharges). Information on dates of birth and diagnosis, sex, topography and morphology, hospital type of diagnosis, and first-line therapy (<12 months after diagnosis) is routinely recorded by trained registrars of the NCR through retrospective medical records review. For this study, we additionally gathered follow-up on subsequent treatment and outcomes with ≥2 years of follow-up after diagnosis. Information on the last known vital status for all patients (ie, alive, dead, or emigrated) is obtained through annual linkage with the Nationwide Population Registries Network that holds vital statistics on all residents of the Netherlands.
Since 1 January 2014, detailed information on diagnostic and treatment characteristics for all hematological malignancies diagnosed in the Netherlands has been recorded in the NCR. The best response was routinely collected from the medical records. Response (complete remission [CR], partial remission [PR], or stable/progressive disease) was determined according to the Lugano classification, by physician assessment using positron emission tomography–computed tomography adapted from international guidelines.
Study population
We identified all newly diagnosed patients ≥18 years of age diagnosed with PTCL NOS, AITL, or ALCL in the Netherlands between 1 January 2014 and 31 December 2019 who received at least 1 cycle of systemic therapy, using the International Coding system of Disease for Oncology of the World Health Organization (WHO) morphology codes 9702 to 9705 and 9714 to 9715 according to local pathology reports. ALK+ and ALK– ALCL were registered as distinct entities in the NCR, according to the WHO classification of 2008 (fourth edition). Patients with other T-NHL subtypes (n = 282) and patients with PTCL NOS, AITL, and ALCL (n = 243) who did not receive primary treatment were excluded from further analyses.
First-line therapy was categorized into 3 groups: (1) CHO(E)P with ASCT, (2) CHO(E)P without ASCT, and (3) other. Treatment in subsequent lines was categorized into 4 groups, that is, multiagent chemotherapy consisting of either dexamethasone, high-dose cytarabine and cisplatin (DHAP) or gemcitabine-cisplatin-dexamethasone (GDP), BV, other, and none. Data on CD30 expression by immunohistochemistry were retrieved for patients treated with DHAP/GDP and patients treated with BV.
In analysis A, overall survival (OS) and progression-free survival (PFS) were evaluated for all patients diagnosed with PTCL NOS, AITL, and ALCL according to the type of first-line treatment. Treatment strategies in second- and third-line were evaluated in analysis B, whereas the impact of DHAP/GDP, BV and allogeneic SCT on outcome among patients with R/R T-NHL was analyzed in analysis C (supplemental Figure 1).
End points
The primary end points for analysis A were OS and PFS. OS was defined as the time after the date of diagnosis until all-cause death. PFS was defined as the time between diagnosis and the first date of relapse or all-cause death, whichever occurred first. Analysis B is descriptive, in which the treatment was evaluated for each individual patient. The primary end points for analysis C were survival outcomes after relapse, OS2 and PFS2. OS2 was defined as the duration of time between the date of relapse and all-cause death. PFS2 was defined as the duration of time between the date of the first or second relapse and all-cause death, whichever occurred first. For PFS2, recurrence of disease was determined when patients experienced complete remission in the previous treatment line. Survival follow-up is until 1 February 2022 (patients alive were censored on this date).
Statistical analyses
Descriptive statistics were used to present patient and treatment characteristics, that is, the Pearson χ2 test was used to compare categorical covariables, and the Kruskal-Wallis test was used to compare nonnormally distributed continuous covariables between the 3 treatment groups in first line. A P value <.05 was considered statistically significant. The Kaplan-Meier method served to estimate OS(2) and PFS(2), and the log-rank test was used to examine differences in survival distributions. OS and PFS were calculated overall as well as for AITL, PTCL NOS, ALK+ and ALK– ALCL separately, and for CHO(E)P with or without ASCT and other therapy. Then, the impact of age at relapse, sex, subtype of T-NHL, time to relapse (≤12 months after diagnosis, >12 months after diagnosis), and second-line treatment on the risk of mortality and (second) relapse was evaluated using univariable and multivariable Cox proportional hazard regression analysis. The results from the Cox regression analyses produce hazard ratios (HRs) with associated 95% confidence intervals (CIs). The proportional hazard assumption was tested based on the Schoenfeld residuals. All covariables, presented as patient and clinicopathological factors in Table 1, were introduced in the multivariable regression model simultaneously, thereby using a backward selection method to exclude covariables with a P value <.05. All analyses were performed using STATA/SE 17.1 (StataCorp LP, College Station, TX).
Baseline characteristics for 821 patients with PTCL NOS, AITL, and ALCL treated in first-line with CHO(E)P with or without autologous SCT or other therapy
| . | Total . | CHO(E)P with ASCT . | CHO(E)P without ASCT . | Other therapy . | ||||
|---|---|---|---|---|---|---|---|---|
| N = 821 . | n = 178 . | n = 542 . | n = 101 . | |||||
| No. . | % . | No. . | % . | No. . | % . | No. . | % . | |
| Male sex | 497 | 61 | 109 | 61 | 336 | 62 | 52 | 51 |
| Median age (range), y | 64 (18-96) | 56 (20-71) | 67 (18-88) | 70 (22-96) | ||||
| Subtype | ||||||||
| PTCL NOS | 266 | 32 | 57 | 32 | 173 | 32 | 36 | 36 |
| AITL | 306 | 37 | 80 | 45 | 199 | 37 | 27 | 27 |
| ALCL | 249 | 30 | 41 | 23 | 170 | 31 | 38 | 38 |
| ALK+ | 95 | 38 | 2 | 5 | 88 | 52 | 5 | 13 |
| ALK– | 148 | 59 | 38 | 93 | 78 | 46 | 32 | 84 |
| ALK unknown | 6 | 3 | 1 | 2 | 4 | 2 | 1 | 3 |
| Ann Arbor stage | ||||||||
| I-II | 173 | 21 | 28 | 16 | 108 | 20 | 37 | 37 |
| III-IV | 640 | 78 | 148 | 83 | 431 | 80 | 61 | 60 |
| Unknown | 8 | 1 | 2 | 1 | 3 | 1 | 3 | 3 |
| Elevated LDH | 417 | 51 | 86 | 48 | 296 | 55 | 35 | 35 |
| WHO performance score | ||||||||
| 0-1 | 356 | 43 | 98 | 55 | 209 | 39 | 49 | 49 |
| 2-4 | 87 | 11 | 14 | 8 | 58 | 11 | 15 | 15 |
| Unknown | 378 | 46 | 66 | 37 | 275 | 51 | 37 | 37 |
| >1 extranodal localization | 160 | 19 | 39 | 22 | 108 | 20 | 13 | 13 |
| IPI score | ||||||||
| 0-1 | 237 | 29 | 58 | 33 | 134 | 25 | 45 | 45 |
| 2 | 232 | 28 | 68 | 38 | 140 | 26 | 24 | 24 |
| 3-5 | 352 | 43 | 52 | 29 | 268 | 49 | 32 | 32 |
| . | Total . | CHO(E)P with ASCT . | CHO(E)P without ASCT . | Other therapy . | ||||
|---|---|---|---|---|---|---|---|---|
| N = 821 . | n = 178 . | n = 542 . | n = 101 . | |||||
| No. . | % . | No. . | % . | No. . | % . | No. . | % . | |
| Male sex | 497 | 61 | 109 | 61 | 336 | 62 | 52 | 51 |
| Median age (range), y | 64 (18-96) | 56 (20-71) | 67 (18-88) | 70 (22-96) | ||||
| Subtype | ||||||||
| PTCL NOS | 266 | 32 | 57 | 32 | 173 | 32 | 36 | 36 |
| AITL | 306 | 37 | 80 | 45 | 199 | 37 | 27 | 27 |
| ALCL | 249 | 30 | 41 | 23 | 170 | 31 | 38 | 38 |
| ALK+ | 95 | 38 | 2 | 5 | 88 | 52 | 5 | 13 |
| ALK– | 148 | 59 | 38 | 93 | 78 | 46 | 32 | 84 |
| ALK unknown | 6 | 3 | 1 | 2 | 4 | 2 | 1 | 3 |
| Ann Arbor stage | ||||||||
| I-II | 173 | 21 | 28 | 16 | 108 | 20 | 37 | 37 |
| III-IV | 640 | 78 | 148 | 83 | 431 | 80 | 61 | 60 |
| Unknown | 8 | 1 | 2 | 1 | 3 | 1 | 3 | 3 |
| Elevated LDH | 417 | 51 | 86 | 48 | 296 | 55 | 35 | 35 |
| WHO performance score | ||||||||
| 0-1 | 356 | 43 | 98 | 55 | 209 | 39 | 49 | 49 |
| 2-4 | 87 | 11 | 14 | 8 | 58 | 11 | 15 | 15 |
| Unknown | 378 | 46 | 66 | 37 | 275 | 51 | 37 | 37 |
| >1 extranodal localization | 160 | 19 | 39 | 22 | 108 | 20 | 13 | 13 |
| IPI score | ||||||||
| 0-1 | 237 | 29 | 58 | 33 | 134 | 25 | 45 | 45 |
| 2 | 232 | 28 | 68 | 38 | 140 | 26 | 24 | 24 |
| 3-5 | 352 | 43 | 52 | 29 | 268 | 49 | 32 | 32 |
IPI, International Prognostic Index; LDH, lactate dehydrogenase; No., number.
According to the Central Committee on Research involving Human Subjects, this type of observational study does not require approval from an ethics committee in the Netherlands. The privacy review board of the NCR approved the use of anonymous data for this study.
Results
Analysis A: first-line treatment and outcome
A total of 821 patients (median age, 64 years; 61% males; 78% stage III-IV) were identified, including 266 patients (32%) with PTCL NOS, 306 (37%) with AITL, and 249 (30%) with ALCL. Among the 249 patients with ALCL, 148 were ALK–, 95 ALK+ and for 6 patients, the ALK status was unknown.
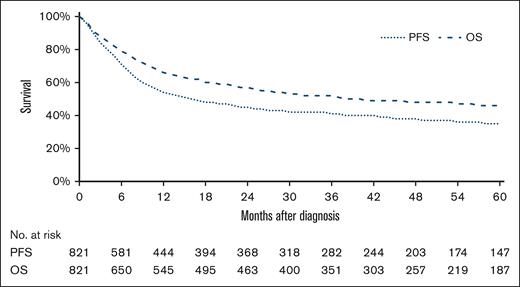
Of the 821 patients, 178 (22%) received CHO(E)P with ASCT, 542 (66%) received CHO(E)P without ASCT, and 101 (12%) received other therapies such as cyclophosphamide-vincristine-prednisolone (COP), COP with etoposide (CEOP), or DHAP. Baseline characteristics according to first-line treatment regimens are shown in Table 1. Overall, the complete remission rates according to CHO(E)P with or without ASCT, or other therapy were 88%, 45%, and 31%, respectively (P < .01; supplemental Figure 2). Progressive disease during first-line treatment was observed for 58 (7%) patients, and relapse after a complete remission (CR) was observed for 253 (30%) patients with a median time of 8 months (range, 1-86) after diagnosis. The incidence of relapse in the central nervous system was 4%. With a median follow-up of 29 months (range, 0.03-97), 2-year PFS and OS estimates were 45% (95% CI, 41-48) and 57% (95% CI, 53-60), respectively (Figure 1) and were superior for patients with an ALK+ ALCL compared with patients with an ALK– ALCL, PTCL NOS, or AITL (supplemental Figure 3).
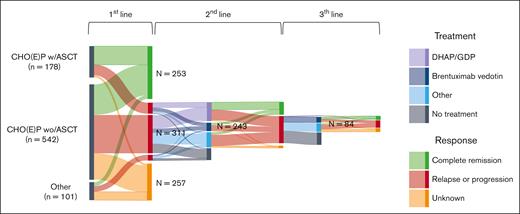
Analysis B: treatment in relapsed T-NHL
Subtype distribution among the 311 patients with R/R T-NHL was 113 (36%) with PTCL NOS, 126 (41%) with AITL, 21 (7%) with ALK+ ALCL, and 51 (16%) with ALK– ALCL (supplemental Table 1). The relapse rate was highest for patients with PTCL NOS (42%), compared with patients with AITL (41%), ALK– ALCL (33%), and ALK+ ALCL (22%; P < .01). Treatment patterns and sequencing across different lines of therapy are visualized in a Sankey plot (Figure 2). Overall, 243 patients (78%) received second-line treatment. Second-line treatment strategies differed between patients who received CHO(E)P with ASCT, CHO(E)P without ASCT or other therapy in first-line. Most of the relapsed patients treated with CHO(E)P with ASCT received DHAP/GDP (n = 28; 45%) or BV (n = 21; 34%), whereas 9 patients (15%) received other therapy, and 4 patients (6%) did not receive further treatment (supplemental Figure 4). Of the relapsed patients treated with CHO(E)P without ASCT in first line, 77 (35%) received DHAP/GDP, of whom 4 in combination with BV, 23 (11%) received BV only, 63 (29%) received other therapies, and 54 (25%) patients did not receive further therapy. Of the relapsed patients treated with other therapies in first-line, 2 (6%) received DHAP/GDP, 5 (16%) received BV, 15 (47%) received other therapy, and 10 (31%) did not receive further therapy. Treatment strategies among the 86 patients in second-line treated otherwise in first-line were heterogenous and consisted of low-dose chemotherapy, CHOP-based, radiotherapy, immunosuppression, steroids, intensive chemotherapy, purine analogues, HDACi, or resection. Among this subgroup of patients, 11 received additional rituximab, of whom 10 had a AITL subtype (supplemental Table 2). Overall, ASCT in second-line was performed in 24 patients (10%), allogeneic SCT in 27 patients (12%), and 1 patient received an ASCT followed by an allogeneic SCT. Among the 28 patients treated with DHAP/GDP in second-line after CHO(E)P with ASCT in first- line, 14 patients (50%) proceeded to allogeneic transplantation. None of these patients received another ASCT in second-line.
Treatment strategies among 821 patients with PTCL NOS, AITL, and ALCL in first-, second-, and third-line treatment.
Treatment strategies among 821 patients with PTCL NOS, AITL, and ALCL in first-, second-, and third-line treatment.
Regarding histological subtype, patients with ALK+ ALCL were most frequently treated with DHAP/GDP, whereas patients with PTCL NOS, AITL, and ALK– ALCL were more often treated with BV or other therapy (P < .01; supplemental Figure 5).
Among 96 patients who experienced a second relapse, 84 (87%) were treated in third-line with BV (n = 32; 38%), DHAP/GDP (n = 3; 4%), or other therapy (n = 49; 58%; Figure 2), that is, low-dose chemotherapy regimens, immunosuppression, intensive chemotherapy regimens, radiotherapy, HDACi, purine analogues, steroids, and CHOP-based regimens (supplemental Table 2). Of the 84 patients, 14 (12%) received an allogeneic SCT, of whom 4 patients also received an ASCT in second-line.
Analysis C: outcome in relapsed T-NHL
With a median follow-up of 10 months (range, 0.03-89.6), the overall response rate for 243 patients treated in second-line was 47% (n = 113), of whom 35% (n = 84) achieved a CR and 12% (n = 29) a PR. The CR rates of patients who received DHAP/GDP, BV, or other therapy were 40%, 43%, and 23% (P = .02), respectively. The CR rate was highest for patients with ALK+ ALCL compared with patients with ALK– ALCL, AITL, and PTCL NOS regardless of type of second-line therapy (supplemental Figure 6). Among the 84 patients treated in third-line, the overall response rate was 43%, of whom 25% experienced a CR.
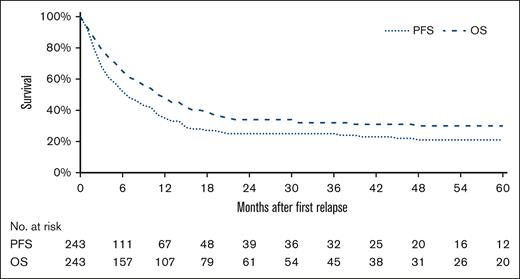
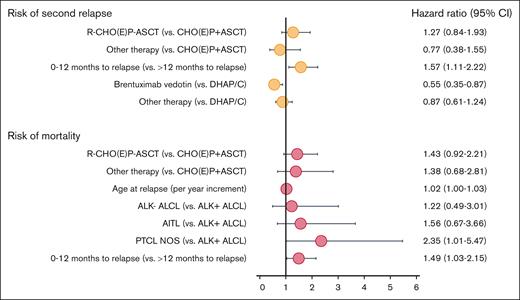
The 2-year OS and PFS estimates after first relapse (OS2 and PFS2) for all R/R patients were 29% and 21%, respectively, and for R/R patients treated with DHAP/GDP, BV or other therapy, 34% and 25%, respectively (Figure 3). In multivariable analysis simultaneously adjusted for treatment regimen in first-line, sex, age at relapse, International Prognostic Index score, stage, histological subtype of T-NHL, time between primary diagnosis and first relapse (0-12 months or >12 months), and type of treatment in secondline, the risk of second relapse was negatively affected when first relapse occurred within 12 months after diagnosis (HR, 1.57; 95% CI, 1.11-2.22; P = .01), whereas BV was associated with a decreased risk of relapse (HR, 0.55; 95% CI 0.35-0.87; P = .01). The risk of mortality for treated R/R patients was adversely affected by older age per year increment (HR, 1.02; 95% CI, 1.00-1.03; P = .01), relapse within 12 months of diagnosis (HR,1.49; 95% CI, 1.03-2.15; P = .03), and PTCL NOS subtype (HR, 2.35; 95% CI, 1.01-5.47; P = .02). Type of treatment in second-line did not affect risk of mortality (Figure 4 and supplemental Figure 7).
PFS and OS among 243 relapsed patients with T-NHL treated with chemotherapy in second-line.
PFS and OS among 243 relapsed patients with T-NHL treated with chemotherapy in second-line.
Forest plot of multivariable analysis for risk of mortality and risk of relapse among 243 patients relapsed T-NHL.
Forest plot of multivariable analysis for risk of mortality and risk of relapse among 243 patients relapsed T-NHL.
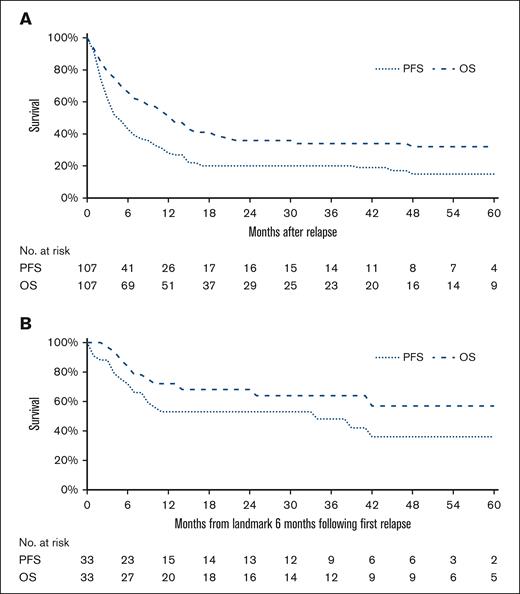
Because of the crossover between treatments in second- and third-line, survival data for DHAP/GDP and BV were analyzed separately. The 2-year OS2 and PFS2 for patients treated with DHAP/GDP were 36% (95% CI, 26-45) and 20% (95% CI, 13-29), respectively (Figure 5A). At 5-year follow-up, the PFS decreased to 15%. In multivariable analyses, CHO(E)P without ASCT negatively affected the risk of mortality and risk of relapse (supplemental Tables 3 and 4). Moreover, older age at relapse negatively affected the risk of mortality, whereas early relapse did not (supplemental Table 3). A landmark analysis at 6 months after first relapse among 33 patients treated with subsequent SCT (31%; 17 autologous and 16 allogeneic) showed an improved 2-year OS2 and PFS2 of 68% (95% CI, 49-81) and 53% (95% CI, 34-68), respectively (Figure 5B). There was not a significant difference in outcome between patients who received an ASCT or allogeneic SCT in second-line (2-year OS 69% [95% CI, 45-84] and 63% [95% CI, 42-78], respectively; P = .08).
Survival curves among 107 patients with relapsed T-NHL treated with DHAP/GDP in second-line. (A) 5-year OS and PFS curves are presented. (B) 5-year OS and PFS are presented for 33 patients who received autologous or allogeneic SCT after DHAP/GDP, using a landmark analysis.
Survival curves among 107 patients with relapsed T-NHL treated with DHAP/GDP in second-line. (A) 5-year OS and PFS curves are presented. (B) 5-year OS and PFS are presented for 33 patients who received autologous or allogeneic SCT after DHAP/GDP, using a landmark analysis.
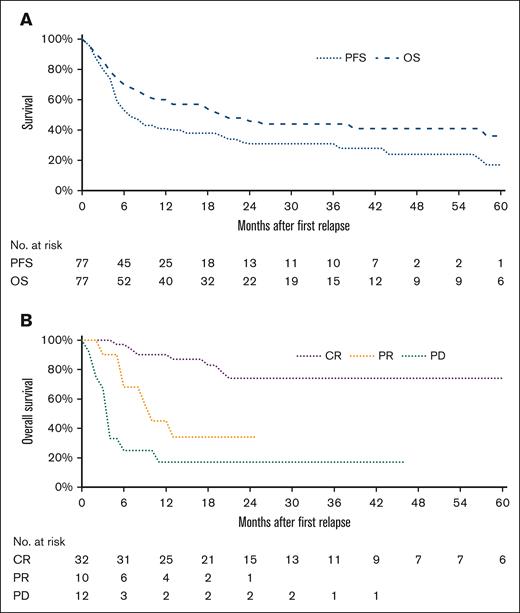
The 2-year OS2 and PFS2 for 77 patients treated with BV (40% ALCL, 34% AITL, and 26% PTCL NOS) were 44% (95% CI, 32-56) and 31% (95% CI, 20-42), respectively (Figure 6A). In univariable and multivariable analyses including first-line treatment, time to first relapse, age at first relapse, subtype of T-NHL, and whether BV was administered in second- or third-treatment line, only PTCL NOS negatively affected the risk of mortality (supplemental Table 5) and risk of relapse (supplemental Table 6), whereas first-line treatment, age, time to first relapse, and BV sequelae did not. For 32 patients who achieved a CR after BV, the 2-year OS was 74% (Figure 6B) and this was irrespective of histological subtype. One patient received a subsequent ASCT, 17 patients received an allogeneic SCT, and 14 patients did not receive consolidation. Two-year OS among patients who received consolidative SCT was similar to patients who did not receive consolidative SCT (P = .70), although this analysis was based on small numbers of patients.
Survival curves among 77 patients with relapsed T-NHL treated with BV in second- and third-line. (A) 5-year OS and PFS curves are presented. (B) The 5-year OS curves according to response outcome are presented.
Survival curves among 77 patients with relapsed T-NHL treated with BV in second- and third-line. (A) 5-year OS and PFS curves are presented. (B) The 5-year OS curves according to response outcome are presented.
In total, 42 patients (17%) with R/R T-NHL received an allogeneic SCT. The median age at first relapse of patients who received an allogeneic SCT in the second- or third-line was significantly lower compared with patients without an allogeneic SCT (54 years and 65 years, respectively; P < .01). The 2-year OS2 and PFS2 for patients undergoing an allogeneic SCT were both 60% (supplemental Figure 8).
Discussion
In this contemporary, nationwide population-based study among newly diagnosed patients with PTCL, we demonstrated a relapse rate of almost 40%. Most of the R/R patients were treated with DHAP/GDP or BV. For patients treated with BV, 2-year PFS was superior as compared with patients treated with DHAP/GDP. Long-term remission was observed for patients treated with salvage chemotherapy receiving consolidative autologous and allogeneic SCT, patients in CR with BV, and selected patients undergoing allogeneic SCT. This study is, to our knowledge, the largest population-based study to date, offering comprehensive information on the incidence of relapse as well as the impact of (salvage) therapy on outcome among patients with T-NHL.
The outcome for R/R patients treated with systemic therapy is generally considered poor. Outcome of patients not fit for second-line treatment is detrimental. Also, in patients who are eligible for second-line treatment, sustainable remission rates were seen in only 20% of the patients, similar to what was observed in previous studies.18,19 Prognostic factors at relapse were PTCL NOS subtype, older age, and relapse within 12 months after diagnosis.
Because of a paucity of prospective studies in R/R T-NHL, data on optimal treatment strategies are lacking. Here, we observed a heterogenous treatment landscape in the Netherlands, reflecting the variety in histological subtype, applied treatment in first-line, and individual patient characteristics. Most commonly used regimens in refractory settings were salvage chemotherapy and BV. The use of novel agents other than BV was limited to only a handful of patients.
Patients consolidated with ASCT in first-line were most likely to be treated for their relapse, either with DHAP/GDP or BV. Among patients with R/R T-NHL without an ASCT in first-line, salvage therapy with DHAP/GDP was favored over BV in second-line. Consolidation strategies after DHAP/GDP in the second-line varied with respect to the initial therapy. Patients who did not receive ASCT in the first-line were consolidated in the subsequent treatment lines, whereas patients who had received prior ASCT were most likely considered for allogeneic SCT. Patients who received other therapy in the first-line were most likely not to receive subsequent treatment at relapse, possibly reflecting a higher percentage of unfit patients and/or a preference for palliative treatment.
The use of BV was reimbursed for all R/R CD30+ lymphomas, including ALCL, PTCL NOS, and AITL, in the Netherlands from 2013 onward. Currently, there are no data available supporting a potential association between CD30 expression and the efficacy of BV.20 As such, CD30 expression of 1% or more established with immunohistochemistry, is indicated as positive in Dutch clinical practice, irrespective of histological subtype. Among the histological subtypes, BV was most commonly used for patients with ALCL as compared with patients with PTCL NOS or AITL. The efficacy of BV as a single agent in R/R ALCL was reported in 2012 with a CR rate of 59%, which led to a provisional European Medicines Agency (EMA) approval.14 Until now, its efficacy has not been confirmed in monotherapy studies among patients with R/R ALCL. In a phase 2 study from 2014, BV showed improved outcome for patients with PTCL NOS and AITL, but a formal EMA approval is pending.15 Nevertheless, in this study, BV was used as second-line treatment in over 10% of the patients with PTCL NOS and AITL. Moreover, BV was the most frequently used therapy in the third-line.
The proportion of patients receiving a consolidative allogeneic SCT in R/R setting was low. This probably reflects either the poor response to salvage therapy or comorbidities prohibiting consolidative SCT. In previous studies, the impact of allogeneic SCT in the R/R setting showed a rather favorable outcome. Explanations may lie in differences between the evaluated patient populations, including the number of patients as well as the exclusion of the most frail or unfit patients.16,17
The PFS2 for patients treated with DHAP/GDP was poor. The best survival outcome was seen in patients who received a consolidative SCT and were disease-free at 5 months, reflecting chemotherapy-sensitive disease. The 2-year OS2 of 68% for R/R patients with SCT is in line with similar observations in studies among patients with large B-cell lymphoma, where patients with lymphoma sensitive to chemotherapy benefit from ASCT.21,22 Similar to large B-cell lymphoma, assessment of biological features or disease response, either by using interim positron emission tomography scans or cell-free circulating tumor DNA dynamics, might help in screening T-NHL patients eligible for salvage chemotherapy in an R/R setting.23
The PFS2 and OS2 of BV were analyzed for R/R patients who received BV in second- and/or third-line. Surprisingly, the outcome was superior compared to patients who received DHAP/GDP, regardless of histological subtype. Response rates were in line with those observed in phase 2 studies among patients with R/R CD30+ T-NHL.14,15 Patients achieving a CR after BV had superior outcome, with less than 50% of the patients receiving a consolidative allogeneic SCT. Because of these findings, BV seems to be the preferred salvage regimen for patients with R/R T-NHL, not only in ALCL but also for AITL and PTCL NOS. Moreover, in a pivotal phase 2 study, long-term remission rates in patients with ALCL without SCT were observed, similar to our study.24 Although numbers are limited, these findings challenge us as to whether or not using consolidative SCT to achieve long-lasting CR status.
Studies combining BV and salvage chemotherapy have been reported for classical Hodgkin lymphoma and, more recently, T-NHL.25-27 In classical Hodgkin lymphoma, the toxicity of BV added to DHAP was manageable.25 A preliminary report on the efficacy of BV combined with gemcitabine in R/R T-NHL reported a CR rate of 20%.26 Here, as well as for single-agent BV, the complete remission for patients in CR lasted over 15 months.
In the past decade, most novel agents failed to improve outcome in R/R T-NHL. Although there was a survival plateau for patients with R/R T-NHL treated with HDACi, analyzed in a phase 2 study with limited number of patients, the administration of HDACi in the Netherlands is rare.12 Meanwhile, the impact of PI3K inhibitors, SYK/JAK (spleen tyrosine kinase/janus kinase) inhibitors, and ALK inhibitors seem promising, but confirmatory data are awaited.10,28,29
The main strength of the current study is the use of a nationwide population-based cancer registry, including follow-up data regarding subsequent treatment lines. The limitations of our study mainly pertain to the lack of detailed information on comorbidities, clinical decision-making, toxicities, and, in particular, for patients treated with noncurative intent, the WHO performance score at baseline and response outcome. Moreover, potential misclassification of subtypes of T-NHL may have occurred, although with the current diagnostics and regional tumor boards in the Netherlands, this phenomenon is expected to be less common than in the initial years of the NCR.30 Despite these limitations, our study gives insight into the outcome of patients who are usually not eligible for clinical trials. Future research is needed to support the finding that BV, as a single agent or in combination with other drug agents, is the preferred strategy for patients with R/R T-NHL.
Conclusion
In this contemporary population-based study among patients with R/R T-NHL, the outcome after salvage chemotherapy was poor. The risk of a second relapse was significantly lower for patients with R/R T-NHL receiving BV in second- or third-line treatment compared with salvage chemotherapy. The use of salvage chemotherapy is challenged because of the superior outcome of BV.
Acknowledgments
The authors thank the registrars of the Netherlands Cancer Registry (NCR) for their dedicated data collection. The nationwide population-based NCR is maintained and hosted by the Netherlands Comprehensive Cancer Organisation.
Takeda Netherlands provided funding for data management by the Netherlands Cancer Registry (grant number 95327).
Takeda had no role in collecting, analysis, or writing of the manuscript.
Authorship
Contribution: M.B., F.H., J.S.P.V., W.J.P., and M.N. contributed to study conception and design; M.B., F.H., and M.N. contributed to data analysis; M.B., F.H., W.J.P., and M.N. contributed to writing the original draft of the manuscript; ; M.B., and M.N. had access to and verified the raw data; and all authors contributed to interpretation of data, contributed to writing, reviewing, and editing of the manuscript, and approved submission of the manuscript for publication.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Marcel Nijland, Department of Hematology, University Medical Center Groningen, Hanzeplein 1, Groningen, 9700RB, The Netherlands; email: m.nijland@umcg.nl.
References
Author notes
The data that support the findings of this study are available via the Netherlands Comprehensive Cancer Organization. These data are not publicly available, and restrictions apply to the availability of the data used for the current study. However, these data are available upon reasonable request and with permission of the Netherlands Comprehensive Cancer Organization.
The full-text version of this article contains a data supplement.