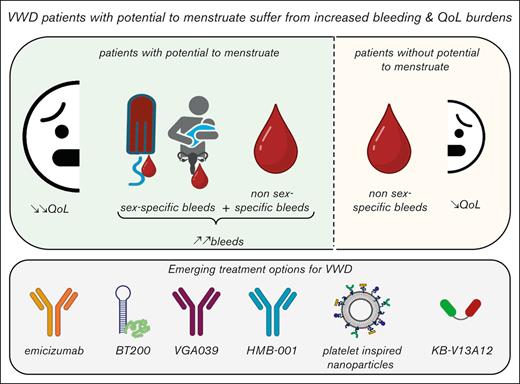
Visual Abstract
Innovation in therapies for patients with von Willebrand disease (VWD) has lagged far behind that for hemophilia, creating inequity in the bleeding disorder community. Although currently existing treatments of antifibrinolytics, desmopressin, and plasma-derived von Willebrand factor replacement are considered effective, multiple studies report poor quality of life in patients with VWD, especially those with heavy menstrual bleeding (HMB). This disconnect underscores the need for novel therapies that are safe and effective and that consider a patient’s specific contraceptive and reproductive needs. Recombinant von Willebrand factor is the most recent new therapy for VWD; the data specific to women are reviewed. We also present emerging data on emicizumab for the treatment of VWD, BT200 (rondoraptivon pegol), generalized hemostatic therapies (VGA039 and HMB-011), as well as treatments based on nanotechnology (platelet-inspired nanoparticles and KB-V13A12). We are optimistic as we move toward pivotal clinical trials for these elegant and innovative treatments.
Introduction
In the past decade, the bleeding disorder community has seen an explosion of innovation in therapeutics to treat and prevent bleeds. The majority of this has been focused on hemophilia including extended half-life concentrates, nonfactor-based therapies, rebalancing agents, and gene therapy.1,2 In contrast, the development of novel therapies for von Willebrand disease (VWD) has lagged far behind, despite its being the most common inherited bleeding disorder. The reasons for this are many and include the heterogeneity of bleeding symptoms experienced by patients with VWD, as well as an under-appreciation of the impact of the disease. The latter is strongly rooted in sexist attitudes about the gynecologic and obstetric bleeding symptoms that exclusively affect women, girls, and people with the potential to menstruate (WGPPM).3
In addition, the pathophysiology of bleeding in VWD is complex and involves deficiency of both the multimeric glycoprotein von Willebrand factor (VWF) as well as coagulation factor VIII (FVIII), in addition to multiple possible specific functional VWF defects (ie, impaired platelet, collagen, or FVIII binding).4,5 This makes designing and implementing treatments, as well as performing clinical trials to evaluate novel VWD therapies, challenging.
VWD is currently classified into 3 types: type 1 is characterized by reduced levels of functionally normal VWF; type 2 is divided into 4 subtypes: 2A (decreased VWF–platelet binding because of loss of high molecular weight multimers), 2B (increased affinity of VWF for platelets, resulting in loss of high molecular weight multimers and variable thrombocytopenia), 2M (decreased VWF–platelet binding with normal multimers), and 2N (decreased VWF–FVIII binding); and type 3, which is caused by a virtual absence of VWF with secondary FVIII deficiency.6 Patients present with a variety of bleeding symptoms including heavy menstrual bleeding (HMB) and postpartum hemorrhage but also nonsex-specific symptoms such as hemarthrosis, gastrointestinal bleeds, epistaxis, easy bruising, oral cavity bleeding, and bleeding after surgery and dental procedures. Currently existing treatments for VWD, including antifibrinolytics, desmopressin, and plasma-derived von Willebrand factor (pdVWF) replacement have been around for decades and are widely considered safe and effective.7 However, quality of life in patients with VWD is known to be poor, especially for those with HMB, which is the most common presenting symptom.8-11 This disconnect underscores the problem facing the VWD community: if current treatments are good, why are patients still suffering?
Multiple studies highlight the inequity and barriers facing women with VWD, including diagnostic delays, serial dismissal of symptoms, and lack of access to appropriate care.12-14 Indeed, in a recent publication, focused on the management of HMB in a tertiary care multidisciplinary clinic, only 68% could be successfully managed medically, and only 17% were satisfied with first-line treatment. This means that patients sequentially trial multiple therapies alone or in combination, only to end up with surgical management to control their bleeding.15 Clearly, there is an urgent need for novel therapies and optimized management strategies for patients with VWD. Here, we summarize new and emerging therapies for WGPPM with VWD, including recombinant von Willebrand factor (rVWF), emicizumab, BT200, generalized hemostatic therapies, and nanotechnology-based therapies. We conclude with a discussion on the characteristics of an ideal treatment for these patients and a view to future pivotal clinical trials.
New treatment options
rVWF
rVWF is the most recent new therapy to become available for patients with VWD. Its pharmacokinetics, safety, and efficacy were reported in 2 prospective trials that enrolled both males and females.16,17 The first, published in 2015, enrolled 37 patients with severe VWD, including 20 females. Participants received rVWF (with or without rFVIII) for on-demand treatment. Overall, bleed control for all (100%) treated bleeds (n = 192 bleeds in 22 patients) was rated as good or excellent. In total, 32 of the mucosal bleeds were menorrhagia, requiring 37 infusions with rVWF. There was a small number of adverse events (AEs; 6 nonserious AEs in 4 patients, and 2 concurrent serious AEs in 1 patient [chest discomfort and increased heart rate without cardiac symptomatology]) and no thrombotic events or severe allergic reactions. For prophylactic treatment, the safety and efficacy of rVWF was reported in 2022.17 In this prospective, open-label, nonrandomized phase 3 study, participants received rVWF prophylaxis at a starting dose of 50 +/- 10 VWF:RCo IU/kg IV twice weekly (or based on their prior pdVWF weekly dosing schedule). The results showed a reduction in spontaneous bleeding events of 91.5% in 13 patients who had previously on-demand received treated, and of 45.0% in 10 patients previously on pdVWF prophylaxis. Of the 23 included patients, 11 were female. Five patients required treatment for spontaneous bleeding events while on study; 3 of these were for menorrhagia. Antifibrinolytics were permitted for treatment of minor or moderate breakthrough bleeds if additional doses of rVWF were not required, and 2 patients received this, but it is not clear whether these were the patients with menorrhagia. In general, it is not possible to distinguish most of the results from these 2 studies based on the sex of participants.
In contrast, the VWDMin study focused exclusively on female patients and was a phase 3, open-label, randomized crossover trial comparing the use of rVWF with tranexamic acid for HMB in patients with mild and moderate VWD.18 Patients were excluded if they were on combined hormonal contraceptives and if they were pregnant or lactating. Participants were assigned to 2 consecutive cycles of rVWF at a dose of VWF:RCo 40 IU/kg IV on day 1 of menses or oral tranexamic acid 1300 mg, 3 times daily on days 1 to 5, in random order. Menstrual blood loss was measured by the pictorial bleeding assessment chart (PBAC) score. Thirty-six patients completed the trial, and the results showed a lower median PBAC score for tranexamic acid (146) than for rVWF (213); however, both remain consistently >100, the threshold used to define HMB. Importantly, the primary end point (a 40-point reduction in PBAC score by day 5 after 2 cycles of treatment) was not met, and the trial was stopped early because of slow recruitment. The fact that all participants received the same single dose of rVWF regardless of baseline VWF levels, and the variability among study participants, likely influenced the results. The authors concluded that rVWF is not superior to tranexamic acid in reducing HMB and advocated for shared decision making with patients when discussing treatment options. The fact that all trial participants still had HMB after treatment with either rVWF or tranexamic acid clearly highlights the need for novel therapies.
Emerging treatment options
Emicizumab
Emicizumab is a bispecific monoclonal antibody that mimics the function of FVIII by bridging activated factor IX and factor X. It has been demonstrated to be highly effective for the prevention of bleeds in patients with hemophilia with and without inhibitors.19 In contrast to standard therapy that involves multiple intravenous infusions of coagulation factor concentrate per week, emicizumab is administered subcutaneously (SC) weekly, biweekly, or monthly, dramatically decreasing the burden of care.19 The off-label use of emicizumab in type 3 VWD has been reported in patients with and without anti-VWF antibodies, with an improvement in hemostasis in all cases.20-25 These case reports include the successful treatment of hemarthrosis in males and females, as well as substantial improvement in HMB in an 11 year old girl with type 3 VWD, anemia, and hypovolemic shock. She had not responded to hormonal therapy, cryoprecipitate, nor tranexamic acid. After the addition of low dose emicizumab (3mg/kg SC, once a month) she had no further menorrhagia or bleeding episodes.25 Moreover, recent in vitro work shows an improvement in thrombus formation under shear in all types of VWD, potentially expanding its clinical use beyond type 3 VWD.26,27
BT200 (rondoraptivon pegol)
BT200 (rondoraptivon pegol) is a pegylated aptamer that binds to the VWF A1 domain and increases VWF and FVIII by decreasing the clearance of both molecules.28 Interestingly, its predecessor, ARC1779, was originally developed as an antithrombotic agent because of its ability to inhibit VWF–platelet interactions.29 BT200 has been studied in type 2B VWD in a prospective phase 2 trial. Participants initially received loading doses of 3 mg SC on days 1, 4, and 7, followed by 6 to 9 mg every week until day 28.30 Five patients, including 2 women, were included, and participant-level data presented. VWF and FVIII levels increased more than twofold, and platelet counts by more than threefold. In all patients with thrombocytopenia, plasma levels of VWF:GPIbM (glycoprotein Ib binding assay for VWF using recombinant mutated GPIb [no ristocetin]) and VWF–collagen binding increased, and high molecular weight multimers were restored. Data presented at the 2023 International Society on Thrombosis and Haemostasis congress showed that BT200 prolongs VWF half-life by blocking its interaction with the macrophage scavenger receptor LRP1, providing in vitro support for a role beyond type 2B VWD.31 Further studies evaluating this molecule in larger numbers of patients with VWD, with bleeding end points, are necessary.
Generalized hemostatic therapies,VGA039 and HMB-001
VGA039
VGA039 is a monoclonal antibody directed against human protein S that inhibits its cofactor activity for tissue factor pathway inhibitor α and activated protein C, enhancing thrombin generation through both the initiation and propagation phases of coagulation. It is administered parenterally (either IV or SC) and has a relatively long half-life of 21 and 12 days, respectively, at doses of 1 mg/kg. In vitro studies showed enhanced thrombin generation in VWF-deficient plasma ,and ex vivo studies showed concentration-dependent increases in thrombin generation as well as dose- and concentration-dependent increases in D-dimer levels.32 Future studies in patients with VWD are critical to establish safety and efficacy
HMB-001
HMB-001 is a bispecific antibody that binds and accumulates endogenous activated FVII in circulation. It promotes activation of factor X and thrombin generation by placing endogenous activated FVII on the surface of activated platelets.33,34 To date, studies have focused on in vivo and ex vivo models of Glanzmann thrombasthenia, but HMB-001 has the potential to treat other bleeding disorders including VWD.
Nanotechnology: platelet-inspired nanoparticles and KB-V13A12
Platelet-inspired hemostatic nanoparticles
Synthetic platelet nanoparticles are small liposomal particles decorated with multiple peptides facilitating concomitant binding to collagen, VWF, and activated platelets. In vitro studies using microfluidic assays show an improvement in thrombus formation using blood from mice with type 2B VWD and deficient of VWF (VWF knockout). In vivo studies using a tail-clip assay showed a reduction in blood loss of 35% in type 2B VWD and of 68% in VWF-knockout mice.35 Clearly, much additional work is needed to translate this therapy into humans and to determine its suitability to treat WGPPM with HMB. However, the customizable nature of synthetic platelet nanoparticles makes them an attractive treatment option for VWD, with its varied and heterogeneous pathophysiology across types/subtypes.
Nanobody-based KB-V13A12
A bifunctional molecule that binds both albumin and VWF, KB-V13A12 prolongs the half-life of endogenous VWF. It has been tested in a mouse model of type 1 VWD; SC administration of the molecule was shown to increase plasma VWF levels by approximately twofold for up to 10 days and restore functional hemostasis in a tail-clip assay.36 A single SC injection with a long half-life is promising for the treatment of HMB, pending translational studies.
Moving toward the future
We must consider the unique values and preferences of WGPPM with VWD as we move forward with pivotal clinical trials for these molecules. Of course, safe and effective therapies are required. However, attention must also be paid to the specific issues of fertility, teratogenicity, and the changing requirement for contraception over the lifespan of these patients. The monthly nature of menses makes an SC treatment with a half-life of many days very attractive and, for nonhormonal therapies, the ability to be safely combined with contraception is critical.
As mentioned earlier, clinical trials in patients with VWD are complicated. Patients with VWD experience a variety of bleeding symptoms and are heterogeneous in terms of the pathobiological manifestations of their disease. This means inclusion/exclusion criteria must be developed thoughtfully. Additionally, clinical trial design must be equitable; we cannot continue to exclude the very patients who need novel treatments the most. In contrast to hemophilia clinical trials, which have the benefit of a fairly straight forward primary outcome of reduction in annual bleeding rate focused on musculoskeletal bleeds, an appropriate outcome for the mucocutaneous bleeds seen in VWD is more difficult to define. Therefore, we call on the community to adopt and adhere to a set of core outcomes to be reported by all trials that encompass the burden of disease experienced by patients with VWD, and we expect results to be presented in a way that allows for sex-specific interpretation. We also expect trial end points to be feasible and patient-focused and urge regulators to move away from the reliance on arcane measures such as alkaline hematin methods for the evaluation of menstrual blood loss. We understand that recruiting trial participants is likely to be a challenge in the very near future. However, as a community, we managed to navigate this for novel therapies for hemophilia; patients with VWD deserve no less.
The innovation and elegance of the aforementioned molecules is impressive and inspiring. We are optimistic for the future of care for WGPPM with VWD.
Acknowledgment
The visual abstract was created using BioRender.com.
Authorship
Contribution: All authors contributed to the writing of this manuscript and have approved its final version.
Conflict-of-interest disclosure: C.C. is coinventor on a patent regarding KB-V13A12. J.L. has received honoraria payments from CSL Behring. P.D.J. receives research funding from Bayer and consultancy fees from Band/Guardian Therapeutics, Star/Vega Therapeutics, BioMarin, and Roche.
Correspondence: Paula D. James, Queen’s University, Medicine, Room 2015, Etherington Hall, 94 Stuart St, Kingston, ON K7L 3N6, Canada; email: jamesp@queensu.ca.