TO THE EDITOR:
Sickle cell disease (SCD) is an inherited blood disorder, which predominantly affects ethnic and racial minority groups1 who may broadly face some health disparities.2 Among other morbidities, there are numerous male reproductive health care needs specific to SCD and its treatments that remain unaddressed, such as genetic transmission implications and education on contraception and potential impact on fertility.3-5 Adolescents and young adults (AYAs) with SCD have expressed interest in learning more about their reproductive health,6-8 and 89% of pediatric SCD clinicians agree that this education should be provided.9 However, previous research shows that AYAs with SCD have knowledge gaps on these topics8,10 and that reproductive health counseling and education are not routinely provided in a format that is accessible and understandable.9,11
Despite calls for the integration of reproductive health education into SCD clinics,11,12 to the best of our knowledge, there are no educational tools for male AYAs with SCD that address the genetic inheritance of SCD, methods to prevent unplanned pregnancy and sexually transmitted infections, and potential fertility impacts of SCD and its treatments. Thus, we developed a web-based reproductive health education program entitled Fertility edUcation To Understand ReproductivE health in Sickle cell disease (FUTURES)13 that is specific for male AYAs with SCD and their caregivers.10 The aims of this pilot study were to examine the program’s preliminary efficacy in achieving high reproductive health knowledge (RHK) and assess acceptability among male AYAs with SCD and their caregivers. We also explored factors associated with RHK gain, such as sociodemographic factors, health literacy, and satisfaction with the FUTURES.
An institutional review board–approved study was conducted among male AYAs aged from 14 to 22 years with SCD and their caregivers (legal guardians) at a large Midwestern pediatric academic medical center. Eligible participants (reporting English proficiency and primarily receiving care at the center) were recruited at the clinic or via telephone between November 2022 and April 2023. AYAs who were ineligible had received a bone marrow transplant (because a fertility consult is a routine part of this procedure) or participated in a community advisory board that informed FUTURES’ development. After obtaining informed consent (and assent if patients were aged <18 years), participants electronically (via the provided tablet or a personal device) completed the following: (1) initial surveys assessing sociodemographics, RHK (using a survey developed by the research team),10 and the Newest Vital Signs screening14; (2) FUTURES (2023; a ∼10-minute, self-administered education program)13; and (3) follow-up surveys assessing RHK and attitudes and satisfaction with FUTURES, administered to all participants immediately after completion of FUTURES. Medical information (eg, genotype and treatment history) was extracted from electronic medical records.
Participants with ≥70% correct answers on the 10 RHK questions were considered to have high RHK. Individuals were considered to have limited health literacy if they scored <4 on the Newest Vital Signs screening tool.14 Paired-sample t tests and McNemar tests were used to examine differences in knowledge scores before and after completing the educational program. Pearson correlations and Fisher exact tests were used to examine bivariate associations between focal variables (eg, sociodemographic characteristics, health literacy, and knowledge). Analyses were completed using Statistical Package for the Social Sciences (version 28.0).15
Of the eligible AYAs (n = 48), 45 could be reached, and 33 (73%) enrolled. Of the 25 approached caregivers, 19 (76%) enrolled, and 17 completed all parts of the study; 89% of enrolled caregivers had a child aged <18 years who was enrolled in the study. Twelve of the 52 total participants completed their participation via telephone. The median age of the AYAs was 17 years (interquartile range, 4); 19 (58%) had hemoglobin SS, 10 (30%) had hemoglobin SC, and 4 (12%) had another genotype. Twenty-one (64%) used hydroxyurea at some time point. Ten (30%) were sexually active, of whom 7 reported never/inconsistently using contraception, and 1 had a biological child. Caregivers were mostly female (89%), and ≤56% had a high school diploma. Nine caregivers reported an annual household income ≤$35 000. In total, 88% of participants were African or African American, and 78% primarily spoke English at home.
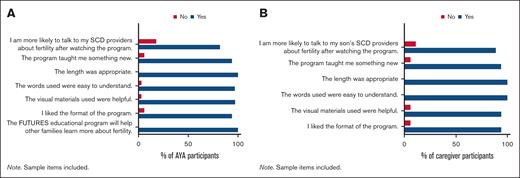
The majority of AYAs (73%) and caregivers (82%) expressed interest (or that their child had interest) in being a biological parent in the future (Table 1). Mean RHK scores before vs after completion of the FUTURES program increased among AYAs (3.73 vs 7.70; P < .001) and caregivers (3.71 vs 7.41; P < .001) (Table 2). The number of AYAs and caregivers achieving high RHK after completion of FUTURES compared with before FUTURES also increased (P < .0001 and P = .02, respectively). Five AYAs (15%) and 3 caregivers (18%) had high RHK scores before completion of FUTURES, compared with 28 (85%) AYAs and 11 (65%) caregivers achieving high RHK after FUTURES. Twenty-two AYAs and 10 caregivers had limited health literacy; having adequate health literacy was not associated with achieving high RHK among AYAs (P > .05), but it was among caregivers (P = .04). Finally, most AYAs and caregivers reported that they liked the format and content of the program and that they learned something new (Figures 1A-B).
Reproductive health attitudes
| Reproductive health attitudes items . | AYA (% agree) . | Caregiver (% agree) . |
|---|---|---|
| I (my son) would like to have a biological child in the future. | 73 | 82 |
| My (my son’s) future goals would be disrupted if I can’t have a biological child. | 24 | 24 |
| My (my son’s) current or future partner may want to have a biological child. | 48 | 94 |
| I would be as happy adopting a child as having a biological child. (It is important to me for my son to have a biological child.) | 55 | 76 |
| I received information about my (my son’s) fertility from my SCD health care team. | 39 | 24 |
| I received information about my (my son’s) fertility from my family. | 36 | 25 |
| I received information about my fertility from the media or internet. | 21 | 12 |
| I have enough knowledge about my (my son’s) fertility. | 30 | 24 |
| I would like more information about how SCD and its treatment could affect my (my son’s) fertility. | 67 | 77 |
| I received information on my (my son’s) fertility from_________. | — | — |
| Reproductive health attitudes items . | AYA (% agree) . | Caregiver (% agree) . |
|---|---|---|
| I (my son) would like to have a biological child in the future. | 73 | 82 |
| My (my son’s) future goals would be disrupted if I can’t have a biological child. | 24 | 24 |
| My (my son’s) current or future partner may want to have a biological child. | 48 | 94 |
| I would be as happy adopting a child as having a biological child. (It is important to me for my son to have a biological child.) | 55 | 76 |
| I received information about my (my son’s) fertility from my SCD health care team. | 39 | 24 |
| I received information about my (my son’s) fertility from my family. | 36 | 25 |
| I received information about my fertility from the media or internet. | 21 | 12 |
| I have enough knowledge about my (my son’s) fertility. | 30 | 24 |
| I would like more information about how SCD and its treatment could affect my (my son’s) fertility. | 67 | 77 |
| I received information on my (my son’s) fertility from_________. | — | — |
AYAs, n = 33; caregivers, n = 17.
Reproductive health knowledge
| RHK items . | AYA (% correct) . | Caregiver (% correct) . | ||
|---|---|---|---|---|
| Before . | After . | Before . | After . | |
| My (my son’s) SCD might affect my (my son’s) fertility. | 49 | 94 | 24 | 53 |
| Receiving a bone marrow transplant has no known effects on fertility for males with SCD. | 21 | 52 | 35 | 47 |
| Taking hydroxyurea might have effects on fertility for males with SCD. | 12 | 91 | 12 | 82 |
| Taking tylenol can affect fertility. | 21 | 64 | 29 | 35 |
| To find out if I (my son) could have a child with SCD, my (son’s) partner must have a blood test. | 76 | 94 | 53 | 94 |
| It may still be possible to get someone pregnant if I received a bone marrow transplant. | 21 | 73 | 44 | 94 |
| It is not possible for a male with SCD to get someone pregnant if he takes/has taken hydroxyurea. | 27 | 61 | 35 | 71 |
| All males with SCD need to use birth control to prevent unplanned pregnancies. | 36 | 82 | 24 | 88 |
| Semen analysis is used to determine whether my sperm is healthy and whether I may be able to have a biological child. | 70 | 79 | 53 | 94 |
| Semen samples can be collected by masturbation. | 39 | 82 | 65 | 82 |
| RHK items . | AYA (% correct) . | Caregiver (% correct) . | ||
|---|---|---|---|---|
| Before . | After . | Before . | After . | |
| My (my son’s) SCD might affect my (my son’s) fertility. | 49 | 94 | 24 | 53 |
| Receiving a bone marrow transplant has no known effects on fertility for males with SCD. | 21 | 52 | 35 | 47 |
| Taking hydroxyurea might have effects on fertility for males with SCD. | 12 | 91 | 12 | 82 |
| Taking tylenol can affect fertility. | 21 | 64 | 29 | 35 |
| To find out if I (my son) could have a child with SCD, my (son’s) partner must have a blood test. | 76 | 94 | 53 | 94 |
| It may still be possible to get someone pregnant if I received a bone marrow transplant. | 21 | 73 | 44 | 94 |
| It is not possible for a male with SCD to get someone pregnant if he takes/has taken hydroxyurea. | 27 | 61 | 35 | 71 |
| All males with SCD need to use birth control to prevent unplanned pregnancies. | 36 | 82 | 24 | 88 |
| Semen analysis is used to determine whether my sperm is healthy and whether I may be able to have a biological child. | 70 | 79 | 53 | 94 |
| Semen samples can be collected by masturbation. | 39 | 82 | 65 | 82 |
AYAs, n = 33; caregivers, n = 17.
RHK items that had a significantly change (P < .05) in response are bolded.
Participants' satisfaction with FUTURES. (A) AYAs’ satisfaction. (B) Caregivers’ satisfaction. Sample items are included.
Participants' satisfaction with FUTURES. (A) AYAs’ satisfaction. (B) Caregivers’ satisfaction. Sample items are included.
In alignment with prior research showing inadequate RHK in AYAs with SCD,5,7,8,16 our study revealed low baseline RHK among male AYAs and their caregivers. Notably, RHK improved (ie, regarding genetic transmission, and hydroxyurea impacts on fertility) immediately after completion of FUTURES in male AYAs and caregivers, including many with limited health literacy. This is similar to findings from prior research using web-based tools to provide reproductive health education to adolescent populations.17-19 However, this is a novel and significant contribution because this is, to our knowledge, the first structured program addressing SCD-specific considerations regarding genetic transmission, contraception, and fertility for male AYAs with SCD and their caregivers.17,20 FUTURES was also highly acceptable, as demonstrated by high recruitment rates and satisfaction ratings, in alignment with previous research showing interest in this topic among AYAs with SCD.6-8
Although high RHK was achieved among 85% of AYAs and 65% of caregivers, we did identify remaining knowledge gaps, particularly among caregivers with limited health literacy, including bone marrow transplant–related fertility impacts and the process by which a semen sample is collected. A notable remaining gap for AYAs was the purpose of a semen analysis. Moreover, after completion of FUTURES, only 61% of AYAs and 71% of caregivers knew that it was possible for a male with SCD to get someone pregnant even if they had taken hydroxyurea, which is especially worrisome for our cohort, given that the majority of AYAs were on hydroxyurea and, never/inconsistently used contraception when sexually active, and 1 AYA already had a biological child. The research team intends to refine the materials in future iterations by adjusting the language of survey items to be clearer, applying formal health literacy evaluation tools (Center for Disease Control Clear Communication Index21 and the Patient Education Materials Assessment Tool22), and updating content to reflect data that emerge on reproductive health in SCD. Findings should be considered among its limitations of being a small, single-site, and cross-sectional study and the lack of a control group to contextualize RHK findings. Future studies are needed to determine whether knowledge gain is sustained and whether limited device and/or internet access could reduce scalability.
In conclusion, findings suggest web-based programs such as FUTURES have the potential to educate AYAs with SCD on various health topics to allow them to make informed health decisions and overcome the access and time constraint barriers that are common to this population.2,23,24 Larger, multicenter, longitudinal studies are warranted to determine whether FUTURES could achieve high and sustained RHK across diverse SCD populations and improve reproductive and psychosocial outcomes.
Acknowledgment: This work was supported by The Ohio State University Center for Clinical and Translational Science Award under grant UL1TR002733.
Contribution: L.N. and S.E.C. were the principal investigators and obtained research funding; L.N., S.E.C., G.P.Q., M.A.A., T.B.-K., C.J.S., S.M.L., and Z.A.C. contributed to study conception and design; C.J.S., S.M.L., and Z.A.C. coordinated the project; C.J.S., S.M.L., and J.R.S. analyzed the data; C.J.S., L.N., and S.E.C. contributed to writing the first draft of the manuscript; and all authors contributed to the revision of the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Susan Creary, Nationwide Children's Hospital, 700 Children’s Dr, Columbus, OH 43205; e-mail: susan.creary@nationwidechildrens.org.
References
Author notes
∗C.J.S. and S.E.C. contributed equally to this study.
Data are available on request from the corresponding author, Susan E. Creary (susan.creary@nationwidechildrens.org).