Key Points
The CLL15 signature, based on the expression of genes associated with microenvironment signaling, predicts early progression in CLL.
The predictive power of the CLL15 signature is independent of the IGHV mutational status and IPS-E CLL score.
Abstract
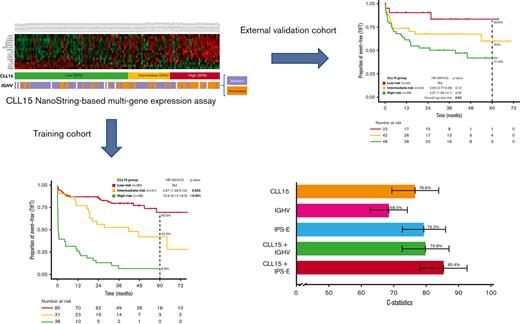
Several gene expression profiles with a strong correlation with patient outcomes have been previously described in chronic lymphocytic leukemia (CLL), although their applicability as biomarkers in clinical practice has been particularly limited. Here we describe the training and validation of a gene expression signature for predicting early progression in patients with CLL based on the analysis of 200 genes related to microenvironment signaling on the NanoString platform. In the training cohort (n = 154), the CLL15 assay containing a 15-gene signature was associated with the time to first treatment (TtFT) (hazard ratio [HR], 2.83; 95% CI, 2.17-3.68; P < .001). The prognostic value of the CLL15 score (HR, 1.71; 95% CI, 1.15-2.52; P = .007) was further confirmed in an external independent validation cohort (n = 112). Notably, the CLL15 score improved the prognostic capacity over IGHV mutational status and the International Prognostic Score for asymptomatic early-stage (IPS-E) CLL. In multivariate analysis, the CLL15 score (HR, 1.83; 95% CI, 1.32-2.56; P < .001) and the IPS-E CLL (HR, 2.23; 95% CI, 1.59-3.12; P < .001) were independently associated with TtFT. The newly developed and validated CLL15 assay successfully translated previous gene signatures such as the microenvironment signaling into a new gene expression–based assay with prognostic implications in CLL.
Introduction
It is well accepted that patients with chronic lymphocytic leukemia (CLL) who are asymptomatic and in an early clinical phase do not require therapy.1 Nevertheless, cumulative data on the risk of clonal evolution2-4 renewed interest in early therapeutic intervention in patients at diagnosis who are likely to progress rapidly.5 Therefore, the identification of these patients at diagnosis has been an intense focus of clinical research in the field of CLL. Prognostication in this setting has classically relied on a myriad of laboratory values, cytogenetic abnormalities, gene mutations, or the mutational status of the IGHV genes.6-10 More recently, the International Prognostic Score for Early-stage CLL (IPS-E) has been developed employing 3 covariates: unmutated IGHV, absolute lymphocyte count > 15 × 109/L, and presence of palpable lymph nodes.11
Despite this extensive investigation, the accuracy of these models may be improved.11-16 In addition, the emergence of novel targeted agents has attracted interest in the early treatment of patients at high risk of early progression.5
Gene expression profiles and the clinical course of patients with CLL have been correlated in various studies.7,8,17-26 Unfortunately, biomarkers based on gene expression profiles exhibit several caveats that preclude them from being widely applied in the prognostication of patients with CLL. These include the lack of reproducibility and standardization and the complexity of bioinformatics analysis. Significantly, the prognostic value of clustering methods is limited by the fact that the assignment of an individual may vary when different patients are included in the clustering process, thus impeding the use of these methods in real time. In this regard, the development of new platforms that allow direct and reproducible quantification of gene expression, such as NanoString nCounter, should facilitate the attainment of gene expression biomarkers applicable in clinical settings.27,28 Among different gene signatures, and because CLL is a malignancy that is particularly dependent on interaction with the microenvironment for survival and proliferation,25IGHV mutational status signature7,8,17,18 and genes involved in the activation of malignant cells in the microenvironment, including stimulation of the B-cell receptor (BCR),24-26,29 are of particular interest. Indeed, this notion is reinforced by the standard use of different small molecules targeting CLL-microenvironment interactions, particularly Bruton’s tyrosine kinase inhibitors.30,31
Herein, we developed, evaluated, and validated a multigene expression signature using genes associated with the activation of CLL cells in the microenvironment and the IGHV mutational status. This assay, based on the NanoString platform, should facilitate its applicability in clinical settings.
Materials and methods
Study design and patient population
The overall design of the process for developing and evaluating a new assay to assess the risk of progression in patients with CLL is shown in supplemental Figure 1. For the training cohort of the study, 156 untreated samples, 119 from the University Hospital Vall d’Hebron and 37 from the University of Salamanca, were used. The assay was validated using 112 samples from an independent cohort of patients from the German Cancer Research Center, Heidelberg, Germany. The details of the validation cohort have been reported elsewhere.32
Samples were obtained at diagnosis, whenever possible. For patients who did not have a sample at the time of diagnosis, samples were collected during follow-up but always before the patients received any treatment. Gene expression quantification was performed in blood samples from untreated patients diagnosed with CLL. Peripheral blood mononuclear cells were obtained using Ficoll-Paque Plus density gradient (GE Healthcare, Buckinghamshire, United Kingdom) and subsequently cryopreserved until analysis. Tumor cells were purified using immunomagnetic depletion by EasySep Human B Cell Enrichment Kit (StemCell Technologies), and the final tumor content was assessed by flow cytometry. The estimated median tumor content was 98.3% (range, 80-99.9) in the training cohort and 95.7% (range, 86.8%-99.4%) in the validation cohort.
Written informed consent was obtained from all individuals in accordance with the Declaration of Helsinki. The study was approved by the clinical research ethics committee of the Vall d’Hebron Barcelona Hospital Campus.
Gene expression analysis
Gene expression was quantified in 250 ng of RNA on the NanoString platform (NanoString Technologies, WA) using the “high sensitivity” setting on the nCounter PrepStation and 555 fields of view on the nCounter Digital Analyzer. A total of 178 genes were selected from the literature, including genes related to the activation of CLL cells in the microenvironment,23-26 genes that were differentially expressed according to the mutational status of IGHV,7,8,17,18 and other genes of prognostic interest in CLL (supplemental Methods, supplemental Table 1). Normalization for RNA loading was performed using the geometric mean of 22 housekeeping genes (supplemental Table 1). The normalized data were log10 transformed. The reference gene selection is further described in the “Data supplement.”
Predictive gene expression score
Detailed descriptions of model building and performance assessment are provided in the “Data supplement.” In brief, we used the gene expression data from the training cohort to produce a parsimonious predictive model for time to first treatment (TtFT) using a penalized Cox model.33 To evaluate the global performance of the multivariate Cox model obtained from the selected genes, different diagnostic parameters were calculated and are summarized in the “Data supplement” (supplemental Table 2), including R2, Brier score, iAUC (a summary measure of the area under the receiver operating characteristic curve calculated for the different times), and Harrell’s C-statistic, a generalization of the AUC.34,35 The graph obtained for the AUC values at the different time points is shown in supplemental Figure 2. For illustrative purposes, we dichotomized the predictive gene expression score in 3 risk groups using the R partykit package.
Statistical analysis
The statistical analysis plan was prespecified before the evaluation of the gene expression in the training and validation cohort. The primary end point of the study was TtFT, defined as the time from the date of obtaining the sample to the date of treatment onset. To study the predictive capacity of the gene expression score, we relaxed the linearity assumption using restricted cubic splines by means of rms R package (Harrell, F. E. Jr Package “rms” [The Comprehensive R Archive Network, 2016]). Harrell’s C-statistic was calculated to compare the discrimination capacities of different models. The analysis of deviance (analysis of variance R function) was used to study whether the inclusion of new factors had a significant improvement in the predictive capacity of the model. Survival curves were estimated using the Kaplan-Meier method to visualize gene expression risk groups and were compared by the log-rank test. Cox proportional-hazard models were used to obtain hazard ratios (HRs) with 95% CIs without dichotomizing continuous factors.36 To select prognostic variables with the highest impact in TtFT, we performed a least absolute shrinkage and selection operator regression using package glmnet in the R software to build the most parsimonious multivariate model. Imputation of random missing values was carried out via the mice R package (supplemental Table 3). The median follow-up was calculated using the reverse Kaplan-Meier method. All analyses were performed using the R statistical software version 3.6.2.
Results
Generation of a prognostic model based on gene expression: the CLL15 assay
The training cohort was comprised of 156 patients with previously untreated CLL. The median age of the series was 66 years (range, 34-90 years), and 57% of the patients were men. In total, 37% of samples were obtained at the time of CLL diagnosis, whereas 63% were obtained during the follow-up of patients before any CLL treatment. The median time from CLL diagnosis to sample collection was 11.9 months (95% CI, 7.1-22.6). The analysis of TtFT was calculated from the date of collecting the sample to the date of treatment onset. The main clinical and biological characteristics of the series are shown in Table 1. Ninety-two cases (59%) were IGHV mutated, 54 cases (35%) were IGHV unmutated, and 9 cases (6%) were undetermined because of polyclonal, unproductive, or biclonal rearrangement. In 1 case, no IGHV mutational data were obtained.
Patient and disease characteristics of the training cohort
| . | Total cohort (n = 154), n (%) . | CLL15 categories . | P value . | ||
|---|---|---|---|---|---|
| Low-risk group (n = 85), n (%) . | Intermediate-risk group (n = 31), n (%) . | High-risk group (n = 38), n (%) . | |||
| Male | 88 (57.1) | 47 (55.3) | 16 (51.6) | 25 (65.8) | .435 |
| Female | 66 (42.9) | 38 (44.7) | 15 (48.4) | 13 (34.2) | |
| Age, median (range) years | 70 (34-91) | 72 (34-91) | 69 (46-91) | 64 (44-85) | .05 |
| Binet stage | <.01 | ||||
| A | 116 (76.3) | 79 (92.9) | 24 (80) | 13 (35.1) | |
| B | 27 (17.8) | 6 (7.1) | 4 (13.3) | 17 (45.9) | |
| C | 9 (5.9) | 0 | 2 (6.7) | 7 (18.9) | |
| Missing, n | 2 | — | 1 | 1 | |
| Lymphocyte cell count, 109/L – median (range) | 16.8 (3.2-323) | 16.8 (3.2-238) | 15.6 (4.2-323) | 22.1 (7.9-207.4) | .18 |
| Missing, n | 38 | 3 | 7 | 28 | |
| β2-microglobulin | <.01 | ||||
| ≤3.5 mg/dL | 108 (74) | 68 (81.9) | 24 (85.7) | 16 (45.7) | |
| >3.5 mg/dL | 38 (26) | 15 (18.1) | 4 (14.3) | 19 (54.3) | |
| Missing, n | 8 | 2 | 3 | 3 | |
| CLL-IPI | <.01 | ||||
| Low (0-1) | 54 (43.9) | 38 (56.7) | 11 (42.3) | 5 (16.7) | |
| Intermediate (2-3) | 32 (20.8) | 16 (23.9) | 9 (34.6) | 7 (23.3) | |
| High (4-6) | 31 (20.1) | 12 (17.9) | 5 (19.2) | 14 (46.7) | |
| Very high (7-10) | 6 (3.9) | 1 (1.5) | 1 (3.8) | 4 (13.3) | |
| Missing, n | 31 | 18 | 5 | 8 | |
| CLL IPS-E | .785 | ||||
| Low (0) | 24 (27.3) | 16 (25.4) | 7 (36.8) | 1 (16.7) | |
| Intermediate (1) | 44 (50) | 32 (50.8) | 9 (47.4) | 3 (50) | |
| High (2-3) | 20 (22.7) | 15 (23.8) | 3 (15.8) | 2 (33.3) | |
| Missing, n | 28 | 16 | 5 | 7 | |
| IGHVmutational status | <.01 | ||||
| Mutated | 90 (62.5) | 58 (74.4) | 22 (71) | 10 (28.6) | |
| Unmutated | 54 (37.5) | 20 (25.6) | 9 (29) | 25 (71.4) | |
| Undetermined, n | 9 | 7 | — | 2 | |
| Missing, n | 1 | — | 1 | ||
| ZAP-70 | .121 | ||||
| <20% | 88 (74.6) | 54 (78.3) | 20 (80) | 14 (58.3) | |
| ≥20% | 30 (25.4) | 15 (21.7) | 5 (20) | 10 (41.7) | |
| Missing, n | 36 | 16 | 6 | 14 | |
| CD38 | .011 | ||||
| <30% | 117 (84.2) | 69 (90.8) | 24 (85.7) | 24 (68.6) | |
| ≥30% | 22 (15.8) | 7 (9.2) | 4 (14.3) | 11(31.4) | |
| Missing, n | 15 | 9 | 3 | 3 | |
| FISH analysis | |||||
| 17 deletion | 11 (7.9) | 6 (8.1) | 3 (10.3) | 2 (5.4) | |
| 11q deletion | 14 (10) | 8 (10.8) | 3 (10.3) | 3 (8.1) | |
| 13q deletion | 77 (55) | 38 (51.4) | 21 (72.4) | 18 (48.6) | |
| Trisomy 12 | 26 (18.6) | 18 (24.3) | 5 (17.2) | 3 (8.1) | |
| Missing, n | 14 | 11 | 2 | 1 | |
| Complex karyotype (≥3 abnormalities) | .877 | ||||
| No | 63 (90) | 42 (89.4) | 14 (93.3) | 7 (87.5) | |
| Yes | 7 (10) | 5 (10.6) | 1 (6.7) | 1 (12.5) | |
| Missing, n | 84 | 38 | 16 | 30 | |
| TP53 mut | .009 | ||||
| No | 92 (92) | 61 (98.4) | 20 (83.3) | 11 (78.6) | |
| Yes | 8 (8) | 1 (1.6) | 4 (16.7) | 3 (21.4) | |
| Missing, n | 54 | 23 | 7 | 24 | |
| NOTCH1 mut | .351 | ||||
| No | 86 (82.7) | 49 (79) | 23 (92) | 14 (82.4) | |
| Yes | 18 (17.3) | 13 (21) | 2 (8) | 3 (17.6) | |
| Missing, n | 50 | 23 | 6 | 21 | |
| SF3B1 mut | .066 | ||||
| No | 92 (94.8) | 61 (98.4) | 21 (91.3) | 10 (83.3) | |
| Yes | 5 (5.2) | 1 (1.6) | 2 (8.7) | 2 (16.7) | |
| Missing, n | 57 | 23 | 8 | 26 | |
| MYD88 mut | .395 | ||||
| No | 85 (94.6) | 60 (96.8) | 21 (91.3) | 7 (87.5) | |
| Yes | 5 (5.4) | 2 (3.2) | 2 (8.7) | 1 (12.5) | |
| Missing, n | 61 | 23 | 8 | 30 | |
| Median follow-up, months (mo) | 43.8 | 43.6 | 43.8 | 45.9 | .61 |
| . | Total cohort (n = 154), n (%) . | CLL15 categories . | P value . | ||
|---|---|---|---|---|---|
| Low-risk group (n = 85), n (%) . | Intermediate-risk group (n = 31), n (%) . | High-risk group (n = 38), n (%) . | |||
| Male | 88 (57.1) | 47 (55.3) | 16 (51.6) | 25 (65.8) | .435 |
| Female | 66 (42.9) | 38 (44.7) | 15 (48.4) | 13 (34.2) | |
| Age, median (range) years | 70 (34-91) | 72 (34-91) | 69 (46-91) | 64 (44-85) | .05 |
| Binet stage | <.01 | ||||
| A | 116 (76.3) | 79 (92.9) | 24 (80) | 13 (35.1) | |
| B | 27 (17.8) | 6 (7.1) | 4 (13.3) | 17 (45.9) | |
| C | 9 (5.9) | 0 | 2 (6.7) | 7 (18.9) | |
| Missing, n | 2 | — | 1 | 1 | |
| Lymphocyte cell count, 109/L – median (range) | 16.8 (3.2-323) | 16.8 (3.2-238) | 15.6 (4.2-323) | 22.1 (7.9-207.4) | .18 |
| Missing, n | 38 | 3 | 7 | 28 | |
| β2-microglobulin | <.01 | ||||
| ≤3.5 mg/dL | 108 (74) | 68 (81.9) | 24 (85.7) | 16 (45.7) | |
| >3.5 mg/dL | 38 (26) | 15 (18.1) | 4 (14.3) | 19 (54.3) | |
| Missing, n | 8 | 2 | 3 | 3 | |
| CLL-IPI | <.01 | ||||
| Low (0-1) | 54 (43.9) | 38 (56.7) | 11 (42.3) | 5 (16.7) | |
| Intermediate (2-3) | 32 (20.8) | 16 (23.9) | 9 (34.6) | 7 (23.3) | |
| High (4-6) | 31 (20.1) | 12 (17.9) | 5 (19.2) | 14 (46.7) | |
| Very high (7-10) | 6 (3.9) | 1 (1.5) | 1 (3.8) | 4 (13.3) | |
| Missing, n | 31 | 18 | 5 | 8 | |
| CLL IPS-E | .785 | ||||
| Low (0) | 24 (27.3) | 16 (25.4) | 7 (36.8) | 1 (16.7) | |
| Intermediate (1) | 44 (50) | 32 (50.8) | 9 (47.4) | 3 (50) | |
| High (2-3) | 20 (22.7) | 15 (23.8) | 3 (15.8) | 2 (33.3) | |
| Missing, n | 28 | 16 | 5 | 7 | |
| IGHVmutational status | <.01 | ||||
| Mutated | 90 (62.5) | 58 (74.4) | 22 (71) | 10 (28.6) | |
| Unmutated | 54 (37.5) | 20 (25.6) | 9 (29) | 25 (71.4) | |
| Undetermined, n | 9 | 7 | — | 2 | |
| Missing, n | 1 | — | 1 | ||
| ZAP-70 | .121 | ||||
| <20% | 88 (74.6) | 54 (78.3) | 20 (80) | 14 (58.3) | |
| ≥20% | 30 (25.4) | 15 (21.7) | 5 (20) | 10 (41.7) | |
| Missing, n | 36 | 16 | 6 | 14 | |
| CD38 | .011 | ||||
| <30% | 117 (84.2) | 69 (90.8) | 24 (85.7) | 24 (68.6) | |
| ≥30% | 22 (15.8) | 7 (9.2) | 4 (14.3) | 11(31.4) | |
| Missing, n | 15 | 9 | 3 | 3 | |
| FISH analysis | |||||
| 17 deletion | 11 (7.9) | 6 (8.1) | 3 (10.3) | 2 (5.4) | |
| 11q deletion | 14 (10) | 8 (10.8) | 3 (10.3) | 3 (8.1) | |
| 13q deletion | 77 (55) | 38 (51.4) | 21 (72.4) | 18 (48.6) | |
| Trisomy 12 | 26 (18.6) | 18 (24.3) | 5 (17.2) | 3 (8.1) | |
| Missing, n | 14 | 11 | 2 | 1 | |
| Complex karyotype (≥3 abnormalities) | .877 | ||||
| No | 63 (90) | 42 (89.4) | 14 (93.3) | 7 (87.5) | |
| Yes | 7 (10) | 5 (10.6) | 1 (6.7) | 1 (12.5) | |
| Missing, n | 84 | 38 | 16 | 30 | |
| TP53 mut | .009 | ||||
| No | 92 (92) | 61 (98.4) | 20 (83.3) | 11 (78.6) | |
| Yes | 8 (8) | 1 (1.6) | 4 (16.7) | 3 (21.4) | |
| Missing, n | 54 | 23 | 7 | 24 | |
| NOTCH1 mut | .351 | ||||
| No | 86 (82.7) | 49 (79) | 23 (92) | 14 (82.4) | |
| Yes | 18 (17.3) | 13 (21) | 2 (8) | 3 (17.6) | |
| Missing, n | 50 | 23 | 6 | 21 | |
| SF3B1 mut | .066 | ||||
| No | 92 (94.8) | 61 (98.4) | 21 (91.3) | 10 (83.3) | |
| Yes | 5 (5.2) | 1 (1.6) | 2 (8.7) | 2 (16.7) | |
| Missing, n | 57 | 23 | 8 | 26 | |
| MYD88 mut | .395 | ||||
| No | 85 (94.6) | 60 (96.8) | 21 (91.3) | 7 (87.5) | |
| Yes | 5 (5.4) | 2 (3.2) | 2 (8.7) | 1 (12.5) | |
| Missing, n | 61 | 23 | 8 | 30 | |
| Median follow-up, months (mo) | 43.8 | 43.6 | 43.8 | 45.9 | .61 |
P values are for comparisons across the 3 risk groups determined by the CLL15 score.
CLL-IPI, International Prognostic Index for CLL; FISH, fluorescence in situ hybridization.
Digital gene expression for 178 genes of interest and 22 housekeeping genes (supplemental Table 1) was determined in 156 samples from the training cohort. Adequate gene expression was obtained in 154 (99%) samples. Two samples (1%) with not enough quality for expression testing were excluded from the analysis.
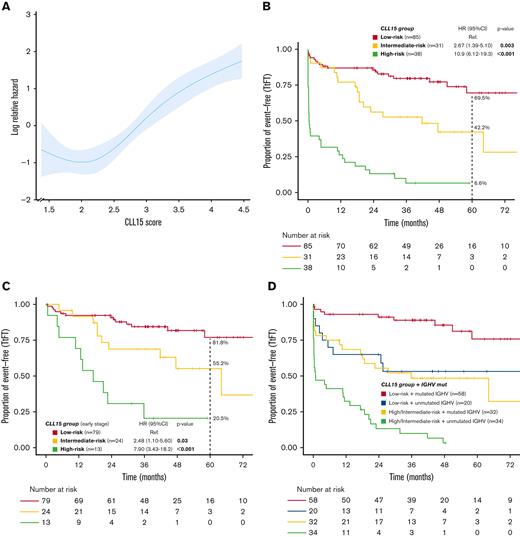
The expression of 76 genes was significantly associated with TtFT in univariate Cox regression analysis (adjusted P value controlling for false discovery rate [FDR] < .05), and 88 with FDR < .1. A total of 46 genes (FDR < .1) met the prespecified inclusion criteria and were selected for further analysis (see “Methods”). Among them, a total of 15 genes (MYC, ITGA4, CERS6, ZNF471, ZNF667, SEPT10P1, ZAP70, LTK, CCL3, CNR1, EGR2, TNF, IL4R, FGL2, PPBP) were finally selected for a prognostic model of TtFT using a penalized Cox method. In addition, 15 housekeeping genes were selected based on their low variance across the samples. A final model, named CLL15, to predict TtFT in the training cohort was developed using the expression of the 15 predictive genes normalized with the 15 housekeeping genes (Figure 1). Subsequently, a linear equation comprising log-transformed, normalized gene expression levels of the 15 genes multiplied by their respective regression coefficients was established and calculated for each patient of the training cohort to obtain the CLL15 score. The C-statistic for the model was 0.77. Figure 2A shows the shape of the association between the CLL15 score and TtFT risk after relaxing the linearity assumption for continuous variables. As a continuous variable, the CLL15 assay score was associated with TtFT (HR, 2.83; 95% CI, 2.17-3.68; P < .001). To better stratify the risk of progression, the optimal thresholds for defining 3 groups with differentiated outcomes (TtFT) were determined using the R partykit package. The low-risk group (score ≤ 2.718, comprising 55% of the cohort) had a 5-year estimated risk of treatment initiation of 30.5%. In the intermediate-risk group (score ≤ 3.535 and >2.718, comprising 20% of the cohort), the 5-year estimated risk of treatment initiation was 57.8% (HR, 2.67; 95% CI, 1.39-5.10; P = .003). Finally, in the high-risk group (score > 3.535, comprising 25% of the cohort) the 5-year estimated risk of treatment initiation was 93.4% (HR, 10.9; 95% CI, 6.12-19.3; P < .001) (Figure 2B). Notably, the CLL15 score exhibited a similar prognostic capacity in the subgroup of patients with an early clinical stage (n = 116), with a 5-year estimated risk of treatment initiation of 18.2%, 44.8%, and 79.54% in the low-, intermediate-, and high-risk groups, respectively (Figure 2C).
The geneexpression–based model to predict TtFT in patients with CLL. A heatmap of the CLL15 assay with 15 informative genes shown as rows and 154 patient samples as columns. The 3 patient groups identified by the assay are shown below the heatmap together with the mutational status of the IGHV genes.
The geneexpression–based model to predict TtFT in patients with CLL. A heatmap of the CLL15 assay with 15 informative genes shown as rows and 154 patient samples as columns. The 3 patient groups identified by the assay are shown below the heatmap together with the mutational status of the IGHV genes.
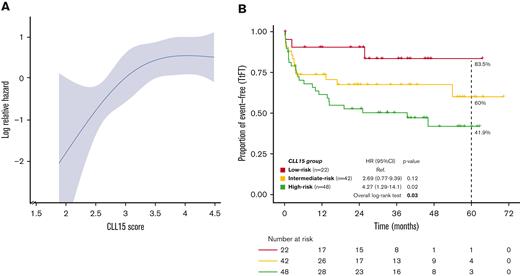
Time to first treatment in the training cohort. (A) Log-relative hazard according to the CLL15 score. (B) Kaplan-Meier curves of the TtFT of the 3 patient groups identified by the CLL15 assay. (C) Kaplan-Meier curves of the TtFT of the 3 patient groups identified by the CLL15 assay in the subgroup of patients with early-stage disease (Binet A 0/I). (D) Kaplan-Meier curves of the TtFT according to CLL15 assay and IGHV mutational status.
Time to first treatment in the training cohort. (A) Log-relative hazard according to the CLL15 score. (B) Kaplan-Meier curves of the TtFT of the 3 patient groups identified by the CLL15 assay. (C) Kaplan-Meier curves of the TtFT of the 3 patient groups identified by the CLL15 assay in the subgroup of patients with early-stage disease (Binet A 0/I). (D) Kaplan-Meier curves of the TtFT according to CLL15 assay and IGHV mutational status.
The prognostic value of the CLL15 score is independent of the IGHV mutational status and IPS-E CLL
We analyzed the association between the progression risk groups obtained by the CLL15 assay with known biological prognostic factors in CLL, including the most common chromosomal alterations determined by FISH (del17p, del11q, and trisomy 12), the level of protein expression of ZAP-70 and CD38 determined by flow cytometry, the mutations in TP53, NOTCH1, SF3B1, and MYD88 genes, the mutational status of IGHV, CLL-IPI, and the IPS-E CLL score.
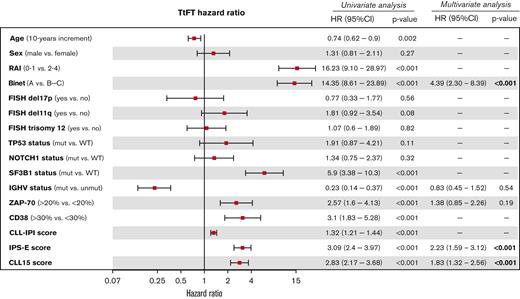
In the univariate analysis, several factors such as the SF3B1 mutations, IGHV status, the expression of ZAP-70 and CD38 by flow cytometry, clinical stage (RAI and Binet), the CLL-IPI, and the IPS-E score were associated with TtFT (Figure 3). In the final multivariate analysis, the CLL15 score, the IPS-E CLL, and the Binet stage were the only factors that maintained their independent statistical significance (Figure 3).
Univariate and multivariate analysis for TtFT according to prognostic factors in CLL.
Univariate and multivariate analysis for TtFT according to prognostic factors in CLL.
We subsequently explored the introduction of the mutational status of the IGHV (mutated/unmutated) as a variable in an expression model and compared its performance with that of a previous model of only gene expression. The C-statistic for the combined model was 0.79, and the analysis of deviance showed that the addition of IGHV status to the gene expression score (and vice versa) provided significant predictive information (analysis of deviance P < .001). According to these results, the model combining gene expression with the IGHV variable performed better in predicting TtFT than the models of gene expression and IGHV by themselves. In the pairwise multivariate Cox models, both variables, IGHV mutational status, and the categorized groups of progression risk according to the gene expression model contributed prognostically (Figure 2D; supplemental Table 4).
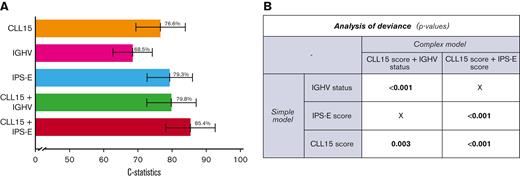
The inclusion of the CLL15 score also improved the capacity to predict TtFT of the IPS-E score. Figure 4A shows the increment in discrimination capacity in terms of C-statistic when the CLL15 score was included in the model concurrently with the IPS-E score or IGHV status. Moreover, in pairwise multivariate Cox models, the CLL-IPI and CLL15 also independently contributed to TtFT in the training cohort, with a C-statistic of 0.73 for the CLL-IPI alone and 0.81 for the combination. However, when the IPS-E score was included, the information on the CLL-IPI did not improve the model (supplemental Table 4). Finally, the (1) CLL15 score, (2) IGHV status, and (3) IPS-E score were all independent factors that improved the prediction of TtFT (all analyses of deviance pairwise comparison, P < .01) (Figure 4B).
Different models to predict TtFT according to CLL15 score, IGHV and IPS-E CLL score. (A) Discrimination capacity in terms of C-statistic according to models including CLL15 score, IGHV mutational status, and IPS-E CLL score. (B) Pairwise ANOVA comparisons. ANOVA, analysis of variance.
Different models to predict TtFT according to CLL15 score, IGHV and IPS-E CLL score. (A) Discrimination capacity in terms of C-statistic according to models including CLL15 score, IGHV mutational status, and IPS-E CLL score. (B) Pairwise ANOVA comparisons. ANOVA, analysis of variance.
Validation and reproducibility of the CLL15 assay
The CLL15 assay was then validated in cryopreserved samples from 112 patients from an independent cohort from Heidelberg (supplemental Table 5). As a continuous variable, the CLL15 score was significantly associated with TtFT (HR, 1.71; 95% CI, 1.15-2.52; P = .007). Figure 5A shows the association between CLL15 score and TtFT risk after relaxing the linearity assumption in the validation cohort. Using the preestablished cut-off in the training cohort, the assay assigned 22 (19.6%) patients to the low-risk group, 42 (37.5%) to the intermediate-risk group, and 48 (42.9%) to the high-risk group. These 3 groups presented differentiated outcomes with a 60-month estimated risk of treatment initiation of 16.5%, 40%, and 58.1% in the low-, intermediate-, and high-risk groups, respectively (P = .03 overall log-rank test, Figure 5B). Moreover, as observed in the training cohort, the gene expression information, both as a continuous variable and as a risk group, was an independent prognostic factor in the presence of IGHV mutational status (supplemental Table 6). The C-statistic for the IGHV mutational status and the gene expression model was 0.6 and 0.63, respectively, whereas the C-statistic for the combined model was 0.67. As observed in the training cohort, 3 risk groups were identified by combining the CLL15 score and the IGHV mutational status information (supplemental Figure 3). To determine the reproducibility of the CLL15 assay, we selected 9 samples with scores distributed across the assay (low risk, intermediate risk, and high risk). The RNA from each of the samples was run on the CLL15 assay in triplicate, with each run performed on a different NanoString cartridge. The results showed 100% concordance of risk-group assignment across triplicates (supplemental Figure 4), with a standard deviation of 0.073 points.
Time to first treatment in the validation cohort. (A) Log-relative hazard according to the CLL15 score in the validation cohort. (B) Kaplan-Meier curves of the TtFT of the 3 patient groups in the validation cohort identified by the CLL15 assay.
Time to first treatment in the validation cohort. (A) Log-relative hazard according to the CLL15 score in the validation cohort. (B) Kaplan-Meier curves of the TtFT of the 3 patient groups in the validation cohort identified by the CLL15 assay.
Discussion
In this study, we translated a gene expression prognostic signature comprising genes involved in the microenvironment activation and IGHV mutational status into a test applicable to categorize patients into the differentiated risk of progression and requiring treatment for their CLL. The assay demonstrated the ability to identify patients at a high risk of requiring treatment in a short time or with an extremely stable disease.
Based on the enormous advances in the biology and treatment of CLL, classical staging systems have been complemented by a plethora of new prognostic parameters based on CLL genetics and biology, including gene expression profiles.14,15,37,38 Despite the fact that gene expression profiles have been strongly correlated with the clinical course of the patients,7,8,17-26 their translational value in clinical practice has been difficult to implement due to methodological reasons. The recent advent of new platforms such as NanoString nCounter, capable of digital, direct quantification on a real-time basis for individual patients, allows the attainment of gene expression analysis in a clinical setting.27,28 In this regard, we demonstrated the clinical strength and reproducibility of the CLL15 assay in an independent cohort of previously untreated patients with CLL and its analytical reproducibility by showing a very low variability across repeated measurements.
Several in vitro and in vivo data indicate that CLL is a malignancy highly dependent on microenvironment signals for survival and proliferation, with BCR signaling being the most prominent pathway activated in CLL cells isolated from lymph nodes.25 The role of the microenvironment in CLL pathogenesis has been reinforced when molecules targeting CLL-microenvironment interactions have shown unprecedented therapeutic results.30,31 The CLL15 assay included genes coding for cytokines, chemokines, and cytokines receptors such as CCL3, TNF, PPBP, and IL4R; integrins such as ITGA4; and transcription regulatory factors such as MYC and EGR2, which are involved in microenvironment activation in different studies in CLL.23-26,39-41 In addition, genes previously reported to be differentially expressed according to the IGHV mutational status, including CERS6, CNR1, FGL2, LTK, SEPT10P1, ZAP70, ZNF471, and ZNF667, were also selected in the CLL15 assay.17,18,24,26,41-44 Notably, the levels of expression of the aforementioned genes could also be regulated in microenvironment activation processes.18,25,45 Thus, ZAP-70 expression has been associated with enhanced and prolonged BCR signaling,46,47 higher responsiveness to chemokines [56-58], and enhanced migration of CLL cells,48,49 reinforcing the notion that increased ZAP-70 expression is associated with a more aggressive clinical course of patients with CLL.37,50,51
It is worth mentioning that the CLL15 signature kept its predictive value independent of the IGHV mutational status, the CLL-IPI, and the IPS-E CLL score. More importantly, the inclusion of the CLL15 score improved the discrimination capacity to predict TtFT when IGHV or IPS-E was included in the model, suggesting that the CLL15 signature could complement the prognostic value of these other variables. In addition, the combination of the CLL15 and CLL-IPI provided independent predictive information; however, with the inclusion of the IPS-E score, the information of the CLL-IPI did not contribute prognostically to the model. In this sense, the combination of the IPS-E and the CLL15 assay was highly discriminative for the TtFT, with a C-statistic of 0.85. It appears that combining a more clinical–based score, such as the IPS-E, with a molecular score (CLL15) could increase the accuracy of both models. Unfortunately, the IPS-E score was not available for the validation cohort and this comparison could not be validated in this cohort.
On the other hand, the combination of IGHV and CLL15 also improved the predictive capacity of the model. Three clearly different risk groups were identified after combining the CLL15 and IGHV status. However, a limited improvement of the C-statistic was observed, and the lower statistical power in the validation cohort did not allow for the validation of all findings.
Currently, one of the moving fields is the possibility of early treatment of patients at early stages that are likely to progress within a short period.5 The selection of these patients is usually based on standard prognostic scores. The usage of more accurate methods for prognostication, such as the CLL15 score, should allow for better identification of patients with an increased risk of early progression and thus support future trials based on risk-adapted therapeutic intervention.
In conclusion, the biological prognostication of CLL relies on the use of genetic aberrations together with the mutational status of IGHV. Unfortunately, the use of gene expression profiles has been difficult owing to its technical difficulties and reproducibility, precluding its use in clinical practice. The use of newer and more reproducible methods to assess gene expression could round off well-established prognostic parameters, appraising the entire biological profile for the prognostication of patients with CLL. The study presented herein successfully translates previously described gene expression signatures with strong prognostic value into a new gene expression–based assay, the CLL15, applicable in the routine diagnostic setting.
Acknowledgments
The authors thank the patients for their blood donations. The authors would also like to thank the Cellex Foundation for providing research facilities and equipment and the CERCA Programme /Generalitat de Catalunya for institutional support. Part of the statistical analysis was performed in the Statistics and Bioinformatics Unit (UEB) of the Vall Hebron Hospital Research Institute.
This work was supported by research funding from the Asociación Española Contra el Cáncer grant [5U01CA157581-05, ECRIN-M3 - A29370] and in part by the Instituto de Salud Carlos III, Fondo de Investigaciones Sanitarias [PI17/00950, M.C., PI17/00943, F.B, PI18/01392, P.A.], and the Spanish Ministry of Economy and Competitiveness [CIBERONC-CB16/12/00233], the Education Council or Health Council of the Junta de Castilla y León [GRS 2036/A/19], and Gilead Sciences [GLD15/00348]. This work was supported by research funding from the Asociación Española Contra el Cáncer grant [5U01CA157581-05, ECRIN-M3 - A29370] and in part by the Instituto de Salud Carlos III, Fondo de Investigaciones Sanitarias [PI17/00950, M.C., PI17/00943, F.B, PI18/01392, P.A.], and the Spanish Ministry of Economy and Competitiveness [CIBERONC-CB16/12/00233], the Education Council or Health Council of the Junta de Castilla y León [GRS 2036/A/19], Gilead Sciences [GLD15/00348] and Gilead Fellowships [GLD16/00144, GLD18/00047, F.B.], and Fundació la Marató de TV3 [201905-30-31 F.B]. All Spanish funding was cosponsored by the European Union FEDER program “Una manera de hacer Europa”. M.C. holds a contract from Ministerio de Ciencia, Innovación y Universidades [RYC-2012-2018].
Authorship
Contribution: P.A., T.Z., M.C., and F.B. designed and supervised this work; P.A., M.C., J.L., T.Z., M.A., M.G., G.I., S.B., and A.M.-N. provided samples; D.M., J.C., J.B., and B.T.-V. performed experiments; P.A., G.V., M.C., and F.B. analyzed and interpreted the data; P.A., G.V., M.C., and F.B. wrote the manuscript; and all authors revised the manuscript.
Conflict-of-interest disclosure: P.A. received honoraria from Janssen, Roche, Celgene, AbbVie, and AstraZeneca. G.V. received research honoraria for speaker activities from MSD and an advisory role from AstraZeneca. M.A. received honoraria for speaker activities from AstraZeneca, an advisory role from Janssen, and nonfinancial support from Janssen, and AbbVie. A.M.-N. received honoraria from Janssen, Roche, Takeda, Gilead, AbbVie, and Celgene for speaker activities and from Janssen, Takeda, Gilead, Kiowa Kirin, AstraZeneca, and Beigene for participating in advisory boards. M.C. received research funding from Janssen, Roche, and AstraZeneca. F.B. received honoraria and research grants from Roche, Celgene, Takeda, AstraZeneca, Novartis, AbbVie, Lilly, Beigene, and Janssen. The remaining authors declare no competing financial interests.
Correspondence: Pau Abrisqueta, Department of Hematology, University Hospital Vall d’Hebron, Pssg Vall d’Hebron 119-129, 08035, Barcelona, Spain; e-mail: pabrisqueta@vhio.net.
References
Author notes
Data are available on request from the corresponding author, Pau Abrisqueta (pabrisqueta@vhio.net).
The full-text version of this article contains a data supplement.
T.Z., M.C., and F.B. contributed equally to this study.