Introduction
The survival gap between children with hematologic malignancies in high-income countries (HICs) and those in low- and middle- income countries (LMICs) such as Mexico is astounding. The causes of high morbidity and mortality in these children include complications and infections related to neutropenic fever (NF). In LMICs, infection-related morbidity and mortality represent a significant source of largely preventable complications and deaths, but sepsis, septic shock, and death can be reduced by prompt detection and timely administration of antibiotics within the first hour after a pediatric patient arrives at the hospital. Our institution, the General Hospital of Tijuana (GHT), is the largest public hospital in Northwestern Mexico, which has a bed occupancy rate of 124% and a mean length of stay of 12 days.
The Pediatric Hematology/Oncology Unit (PHOU) at the GHT opened in 2008 and comprises an isolation ward and an ambulatory infusion center (20 beds). Since the PHOU opened, more than 1200 children have received care. There are 50 to 70 new cases of hematologic malignancies each year. In our PHOU, the second most common reason for admission is NF following administration of chemotherapy. Our aim was to implement the “Golden Hour,” a capacity-building initiative to decrease morbidity and life-threating complications related to NF in pediatric patients with hematologic malignancies.
Objectives
To describe the epidemiology of NF events in patients with hematologic malignancies (leukemias and lymphomas) in 2013 as baseline data.
To train 100% of the nurses (n = 28) in the PHOU and achieve a significant increase in knowledge (>90% gain posttest) as the first step in implementing the Golden Hour.
To train all parents of newly diagnosed patients on the basic concepts of treating fever at home.
To continue development of the Golden Hour, decrease time to antibiotic (TTA) administration to <1 hour in all patients with NF at the GHT PHOU, and measure the impact of the initiative on sepsis rates, admission rates to the Pediatric Intensive Care Unit (PICU), and hospital length of stay.
To ensure that 100% of supplies needed each day are in the Golden Box and prevent shortages of supplies.
Methods
We conducted a 4.6-year prospective cross-sectional study in 4 phases that included patients with NF who were admitted to the PHOU.
Baseline (January 1, 2013-December 31, 2013)
We collected baseline data before the initiative was implemented.
Phase 1 (January 1, 2014-December 31, 2014)
Standardized NF guidelines were developed under the leadership of the pediatric infectious disease specialist dedicated to the PHOU.
The Golden Box was procured and supplies were secured; it contains all of the supplies and medications needed for each NF event (Figure 1).
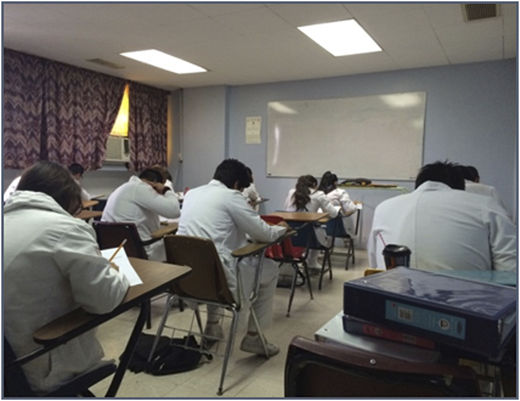
An 8-hour training workshop on NF management and the Golden Hour algorithm was held for nursing staff that included pre- and posttest assessments (Figure 2).
A training workshop was conducted for parents of newly diagnosed patients on the basic concepts of NF (Figure 3).
The program was launched, and the team was present.
All Blue Sheet data were documented (Department of Infectious Diseases, St. Jude Children’s Research Hospital, 2010).
A preliminary analysis of the impact of the program was conducted.
The Golden box showing all of the supplies and medications needed for each NF event.
The Golden box showing all of the supplies and medications needed for each NF event.
Nursing staff at an 8-hour training workshop that included pre- and posttest assessments.
Nursing staff at an 8-hour training workshop that included pre- and posttest assessments.
A training workshop being conducted for parents of newly diagnosed patients on the basic concepts of NF.
A training workshop being conducted for parents of newly diagnosed patients on the basic concepts of NF.
Phase 2 (January 1, 2015-December 31, 2015)
Data were collected and an analysis of the impact of the program was performed.
Phase 3 (January 1, 2016-December 31, 2016)
A refresher workshop was held for nursing and medical staff, and the program was re-launched (the Golden ceremony) (Figure 4).
Data were collected and an analysis of the impact of the program was conducted.
Phase 4 (January 1, 2017-July 31, 2017)
Data were collected and an analysis of the program’s impact was performed.
All procedures were performed in compliance with the Declaration of Helsinki.
Results
In 2013, we documented 12 NF events in patients with hematologic malignancies (11 leukemias and 1 lymphoma) as baseline data. Income level for all 12 patients was extreme poverty.
We trained 100% of PHOU nurses who showed a significant improvement (>90%) in their knowledge posttest. We provided targeted training to parents of diagnosed patients regarding NF.
After implementing the Golden Hour, we analyzed 100 NF events in 51 patients from January 1, 2013, to July 2017 (Table 1).
In phase 1, TTA was reduced from 73.9 minutes (range, 0-254 minutes) to 36.76 minutes (P = .0016).
In phase 2, TTA was 71.07 minutes (range, 0-450 minutes).
In phase 3, after re-intervention, TTA was decreased to 55.51 minutes (range, 15-290 minutes) (P = .01046).
In phase 4, TTA was 30.2 minutes (range, 0-60 minutes) (P = .0002).
Outcomes such as sepsis rates, rates of admission to PICU, and hospital length of stay are described in Table 2.
When there was a temporary shortage of supplies and medications, the local Patronato Foundation supplied the items to stock the Golden Box.
Time to antibiotic delivery by phase of intervention
| . | Baseline, 2013 (n = 12) . | Phase 1, 2014 (n = 25) . | Phase 2, 2015 (n = 14) . | Phase 3, 2016 (n = 29) . | Phase 4, 2017 (n = 20) . |
|---|---|---|---|---|---|
| TTA delivery | |||||
| Mean TTA (min) | 73.9 | 36.76 | 71.07 | 55.51 | 30.2 |
| Median TTA (min) | 67.5 | 30 | 30 | 30 | 30 |
| Standard deviation (min) | 28.75 | 53.4 | 118.4 | 64.9 | 16.88 |
| P | .0016 | .23404 | .010146 | .0002 |
| . | Baseline, 2013 (n = 12) . | Phase 1, 2014 (n = 25) . | Phase 2, 2015 (n = 14) . | Phase 3, 2016 (n = 29) . | Phase 4, 2017 (n = 20) . |
|---|---|---|---|---|---|
| TTA delivery | |||||
| Mean TTA (min) | 73.9 | 36.76 | 71.07 | 55.51 | 30.2 |
| Median TTA (min) | 67.5 | 30 | 30 | 30 | 30 |
| Standard deviation (min) | 28.75 | 53.4 | 118.4 | 64.9 | 16.88 |
| P | .0016 | .23404 | .010146 | .0002 |
Patient outcomes
| . | Baseline . | Phase 1 . | Phase 2 . | Phase 3 . | Phase 4 . | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. . | % . | No. . | % . | No. . | % . | No. . | % . | No. . | % . | |
| Admitted to intensive care unit | 4 | 33.3 | 3 | 12 | 2 | 14.2 | 3 | 10.7 | 1 | 5 |
| Sepsis | 5 | 41.6 | 7 | 28 | 2 | 14.2 | 2 | 7.1 | 2 | 10 |
| Length of stay ± standard deviation (median days) | 8.7 ± 4.1 | 12.6 ± 15.7 | 13.6 ± 15.7 | 9.7 ± 6.3 | 15.3 ± 11.9 | |||||
| Death | 0 | 1 | 4 | 1 | 7 | 1 | 3.5 | 0 | ||
| . | Baseline . | Phase 1 . | Phase 2 . | Phase 3 . | Phase 4 . | |||||
|---|---|---|---|---|---|---|---|---|---|---|
| No. . | % . | No. . | % . | No. . | % . | No. . | % . | No. . | % . | |
| Admitted to intensive care unit | 4 | 33.3 | 3 | 12 | 2 | 14.2 | 3 | 10.7 | 1 | 5 |
| Sepsis | 5 | 41.6 | 7 | 28 | 2 | 14.2 | 2 | 7.1 | 2 | 10 |
| Length of stay ± standard deviation (median days) | 8.7 ± 4.1 | 12.6 ± 15.7 | 13.6 ± 15.7 | 9.7 ± 6.3 | 15.3 ± 11.9 | |||||
| Death | 0 | 1 | 4 | 1 | 7 | 1 | 3.5 | 0 | ||
Conclusions
We showed a significant decrease in the TTA to <60 minutes after the Golden Hour was implemented.
Key interventions included targeted training for parents and medical and nursing staff. A re-intervention and a training refresher were needed to ensure continued impact and sustainment.
Through an effective partnership with the local foundation, we were able to ensure that all supplies and medications were readily available in the Golden Box.
PICU admission rates were also decreased. There was no initial impact on length of stay or mortality.
We demonstrated the feasibility of decreasing the TTA and improving the rate at which supplies to treat NF became readily available to be used in a timely fashion after the Golden Hour was implemented.
The Golden Hour can be successfully reproduced in other resource-strained settings.
Future directions include the periodic intervention evaluation, including impact on mortality. We will re-intervene as needed to ensure long-term sustainability and impact.
Acknowledgments
The authors thank their patients and the patients’ parents for being an inspiration and thank their team members for creating a harmonious environment in the workplace.
Authorship
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Mario Ornelas-Sánchez, Hospital General de Tijuana, Universidad Autónoma de Baja California, Tijuana, Baja California, Mexico; e-mail: marioalbertoornelas0@hotmail.com, and Paula Aristizabal, Peckham Center for Cancer and Blood Disorders, Rady Children's Hospital San Diego, San Diego, CA; Department of Pediatrics, Division of Pediatric Hematology/Oncology, University of California San Diego, La Jolla, CA; and Population Science, Disparities and Community Engagement, University of California San Diego Moores Cancer Center, La Jolla, CA; e-mail: paristizabal@rchsd.org.