Background
The first Department of Clinical Haematology in Myanmar was established in 1994, and since then, specific treatments have been offered for a variety of hematological disorders except for the option of hematopoietic stem cell transplantation (HSCT). Although there was improvement in health care, there were many patients suffering from incurable diseases due to the lack of a HSCT program, which is extremely costly and complicated for a developing country.
Limitations in Myanmar
Myanmar has very limited human resources with <20 hematologists, old and young, covering a population of >50 million. Almost all hospitals are under the Ministry of Health, and HSCT is not a priority compared with the burden of infectious diseases and nutritional deficiencies. Red tape and strict regulations under the previous military government were also not favorable for new projects.
Disease burden
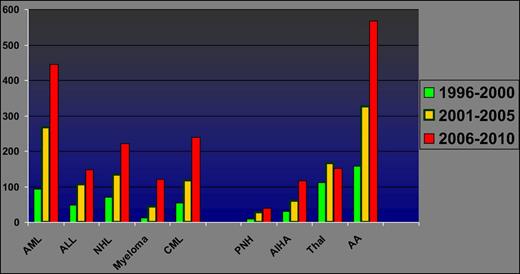
Myanmar has a high burden of hematological disorders, with a large number of hematologic malignancies in particular with increasing numbers of new cases each year (Figure 1).
Trends in hematological disorders at Yangon General Hospital (1996 to 2010), showing increasing numbers of new cases of aplastic anemia and hematologic malignancies in recent years.
Trends in hematological disorders at Yangon General Hospital (1996 to 2010), showing increasing numbers of new cases of aplastic anemia and hematologic malignancies in recent years.
Role of the Myanmar Society of Haematology
In 2003, Myanmar hematologists together with pathologists and clinicians interested in hematology established the Myanmar Society of Haematology (MSH) and started academic activities. Overseas speakers were invited at the local conferences to educate Myanmar clinicians on HSCT. The MSH and eminent transplant physicians visiting Myanmar advocated for HSCT to administrative authorities, including the Minister of Health. In 2010, a leukemia-lymphoma special interest group was formed, under which dedicated members interested in initiating a HSCT started capacity-building initiatives. Hematologists and trainees were also funded to attend overseas meetings and studies.
Role of the Ministry of Health
Along with the transition from a military to a democratic government, the health budget was improved, and the Ministry of Health was able to provide funding for drugs and equipment for apheresis, flow cytometry, and training.
Helping hands from countries in the Asia-Pacific region
Transplant physicians from Singapore, Thailand, India, Australia, Hong Kong, and Japan, who are also members of the Asia-Pacific Blood and Marrow Transplant Group (APBMT) voluntarily visited Myanmar, gave advice, educational talks, and knowledge updates, and shared their experience to help initiate a transplant program in Myanmar (Tables 1 and 2). Volunteers from the Singapore Health Sciences Authorities have come regularly since 2004 to help develop blood group serology and transfusion services in Myanmar.
International experts visiting Myanmar in support of transplant capacity-building
| Period . | Visit of volunteers and experts who are members of APBMT . | Activities . |
|---|---|---|
| 2004-2014 | Regular visits by a team of volunteer hematologists and blood bank technicians from Singapore International Foundation led by a transplant physician to Yangon and Mandalay | Blood group serology workshops and support on blood safety and transfusion services in Myanmar |
| Lectures on stem cell transplantation, case discussions | ||
| Situation analysis and advocacy to authorities | ||
| Advice on individual cases for transplant | ||
| 2009-2013 | Frequent visits by hematologist/transplant physicians from Siriraj Hospital, Thailand, and the Thai Society of Haematology | Meeting with MSH for collaboration and offering training for doctors, nurses, and laboratory personnel |
| Continuing medical education lectures, case consultation | ||
| Education symposium | ||
| Site visit and advice for initiating program | ||
| 2009, 2011 | Visit by hematologist/transplant physicians from Christian Medical College, Vellore, India, and Tata Memorial Hospital, Mumbai, India | Education symposium, meeting with MSH for collaboration and advice on initiating transplant program |
| Site visit and advice for initiating program | ||
| 2013 | Visit by hematologist/transplant physicians from Hong Kong | Education symposium, site visit, and advice |
| 2013 | A team of volunteer hematologist/transplant physicians and infectious disease specialists from St. Vincent’s Hospital, Sydney, New South Wales, Australia | Educational talks on various topics related to HSCT, including infection control and management of infectious complications |
| Courtesy call to Minister of Health and advocacy on HSCT | ||
| Technical advice, advice on specification of flow cytometer, and apheresis machine | ||
| Advice on individual cases for transplant |
| Period . | Visit of volunteers and experts who are members of APBMT . | Activities . |
|---|---|---|
| 2004-2014 | Regular visits by a team of volunteer hematologists and blood bank technicians from Singapore International Foundation led by a transplant physician to Yangon and Mandalay | Blood group serology workshops and support on blood safety and transfusion services in Myanmar |
| Lectures on stem cell transplantation, case discussions | ||
| Situation analysis and advocacy to authorities | ||
| Advice on individual cases for transplant | ||
| 2009-2013 | Frequent visits by hematologist/transplant physicians from Siriraj Hospital, Thailand, and the Thai Society of Haematology | Meeting with MSH for collaboration and offering training for doctors, nurses, and laboratory personnel |
| Continuing medical education lectures, case consultation | ||
| Education symposium | ||
| Site visit and advice for initiating program | ||
| 2009, 2011 | Visit by hematologist/transplant physicians from Christian Medical College, Vellore, India, and Tata Memorial Hospital, Mumbai, India | Education symposium, meeting with MSH for collaboration and advice on initiating transplant program |
| Site visit and advice for initiating program | ||
| 2013 | Visit by hematologist/transplant physicians from Hong Kong | Education symposium, site visit, and advice |
| 2013 | A team of volunteer hematologist/transplant physicians and infectious disease specialists from St. Vincent’s Hospital, Sydney, New South Wales, Australia | Educational talks on various topics related to HSCT, including infection control and management of infectious complications |
| Courtesy call to Minister of Health and advocacy on HSCT | ||
| Technical advice, advice on specification of flow cytometer, and apheresis machine | ||
| Advice on individual cases for transplant |
Foreign centers supporting capacity building for HSCT in Myanmar
| Period . | Transplant center . | Trainees, n . |
|---|---|---|
| 2008-2013 | Bone Marrow Transplant Unit and Transfusion Medicine Department, Siriraj Hospital, Thailand | Transplant physician, 2 |
| Transplant nurses, 3 | ||
| Apheresis/blood bank personnel, 2 | ||
| Laboratory personnel for enumeration of stem cells, 2 | ||
| 2013 | Christian Medical College, Vellore, India | Transplant physician, 1 |
| Transplant nurse, 1 | ||
| 2014 | University of Maryland Greenebaum Cancer Center, Baltimore, MD | Transplant physician, 1 |
| 2015 | St. Vincent’s Hospital, Sydney, New South Wales, Australia | Cryopreservation, 1 |
| Period . | Transplant center . | Trainees, n . |
|---|---|---|
| 2008-2013 | Bone Marrow Transplant Unit and Transfusion Medicine Department, Siriraj Hospital, Thailand | Transplant physician, 2 |
| Transplant nurses, 3 | ||
| Apheresis/blood bank personnel, 2 | ||
| Laboratory personnel for enumeration of stem cells, 2 | ||
| 2013 | Christian Medical College, Vellore, India | Transplant physician, 1 |
| Transplant nurse, 1 | ||
| 2014 | University of Maryland Greenebaum Cancer Center, Baltimore, MD | Transplant physician, 1 |
| 2015 | St. Vincent’s Hospital, Sydney, New South Wales, Australia | Cryopreservation, 1 |
Leadership from the Worldwide Network for Blood and Marrow Transplantation and APBMT
By participating in annual meetings of the APBMT since 2010, knowledge and networks were widened, and experience among the member countries could be shared.
The First International Workshop on HSCT in Emerging Countries, organized by the Worldwide Network for Blood and Marrow Transplantation, was held in 2011 in Vietnam. It was a landmark for HSCT-related activities in the region.
Transplant team and the first HSCT case in Myanmar
In 2014, the very first case of autologous HSCT in Myanmar was successfully performed for a patient with multiple myeloma without cryopreservation in a resource-poor setting.
The unique feature of the first transplant case in Myanmar is that the transplant team, made up of dedicated members of the MSH working in different departments and specialized in different areas, came to make the joint effort to initiate the first step.
Current status of HSCT in Myanmar
From May 2014 to October 2016, a total of 6 cases of autologous HSCT for multiple myeloma were performed (Table 3). All patients except 1 achieved a minimum of 1 year of relapse-free survival at this time.
Characteristics of the patients who underwent autologous stem cell transplantation in Myanmar from 2014 to 2016
| Age | 53-62 years |
| Sex | 4 males and 2 females |
| Myeloma stage | Durie-Salmon stage IIIA in 5 patients, 1 IIIA; International Staging System stage II-III |
| Induction | Bortezomib-thalidomide-dexamethasone induction |
| Remission status prior transplant | Stringent complete remission (CR) to very good partial remission (VGPR) |
| Time from diagnosis to transplant | 6 months to 5 years |
| Mobilization | Granulocyte colony-stimulating factor 10 μg/kg per day subcutaneously, except 1 case of 15 μg/kg per day; high-dose etoposide in 1 case |
| Peripheral blood stem cell harvest | Day 5-7 |
| Storage | In pharmaceutical refrigerator, at 2-4˚C, for 24-72 hours |
| Conditioning | High-dose melphalan (dose, 110-200 mg/m2) |
| Stem cell reinfusion | Reinfuse after high-dose melphalan without cryopreservation after 24-72 hours |
| Stem cell dose | 1.45 × 106-4.75 × 106/kg |
| Engraftment | Neutrophil engraftment: day 10-11; platelet engraftment: day 14-18 |
| Age | 53-62 years |
| Sex | 4 males and 2 females |
| Myeloma stage | Durie-Salmon stage IIIA in 5 patients, 1 IIIA; International Staging System stage II-III |
| Induction | Bortezomib-thalidomide-dexamethasone induction |
| Remission status prior transplant | Stringent complete remission (CR) to very good partial remission (VGPR) |
| Time from diagnosis to transplant | 6 months to 5 years |
| Mobilization | Granulocyte colony-stimulating factor 10 μg/kg per day subcutaneously, except 1 case of 15 μg/kg per day; high-dose etoposide in 1 case |
| Peripheral blood stem cell harvest | Day 5-7 |
| Storage | In pharmaceutical refrigerator, at 2-4˚C, for 24-72 hours |
| Conditioning | High-dose melphalan (dose, 110-200 mg/m2) |
| Stem cell reinfusion | Reinfuse after high-dose melphalan without cryopreservation after 24-72 hours |
| Stem cell dose | 1.45 × 106-4.75 × 106/kg |
| Engraftment | Neutrophil engraftment: day 10-11; platelet engraftment: day 14-18 |
Transplant physicians from Asia and the Pacific region visiting Myanmar for capacity building.
Transplant physicians from Asia and the Pacific region visiting Myanmar for capacity building.
Hematologists from Myanmar attending an APBMT congress and the First International Workshop on HSCT in Emerging Countries.
Hematologists from Myanmar attending an APBMT congress and the First International Workshop on HSCT in Emerging Countries.
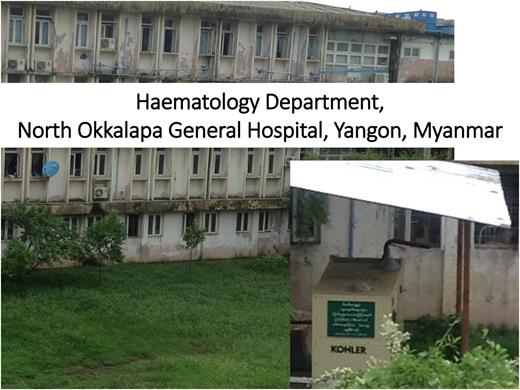
The hematology department at North Okkalapa General Hospital. The first HSCT in Myanmar was done at this hospital in a resource-poor setting. A power generator was used to ensure a stable supply of electricity.
The hematology department at North Okkalapa General Hospital. The first HSCT in Myanmar was done at this hospital in a resource-poor setting. A power generator was used to ensure a stable supply of electricity.
Conclusions
Myanmar has spent several years overcoming many barriers to start an HSCT program. The successful start of this program was made possible with collaboration and support from APBMT members, especially in building the capacity of the Myanmar transplant team. We need to strengthen our transplant capacity to cover not only autologous but also allogeneic transplantation and to cover autologous transplantation for other diseases by improving, for example, cryopreservation techniques, management of posttransplant complications, and data management systems.
Acknowledgments:
The authors thank Yoshihira Kodera and S. Okamoto (APBMT, Japan), Mammen Chandy and Tapan Saikia (India), the Thai Society of Haematology, James C. S. Chim (Hong Kong), Nay Win (NHS Blood and Transplant, United Kingdom), and Aaron Rapoport (University of Maryland).
Conflict-of-interest disclosure: A.S.: Bayer Healthcare, Shire, Novo Nordisk, Roche Genentech, and LFB (research funding, other). Other authors: No competing financial interests declared.
Correspondence: Aye Aye Gyi, Department of Clinical Haematology, North Okkalapa General and Teaching Hospital, Yangon, Myanmar; e-mail: ayeayegyi@gmail.com.