Background
Sickle cell anemia (SCA) is the most common and severe inherited hemoglobinopathy worldwide.1 The global burden of SCA is highest in sub-Saharan Africa, where >75% of SCA occurs.1
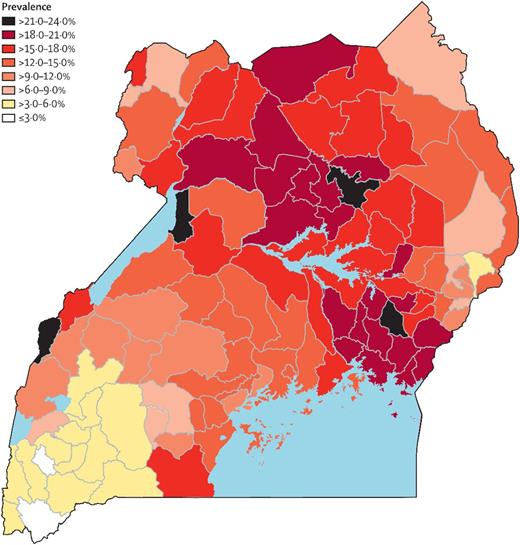
In Uganda, the gene prevalence of HbS is 13%, with an estimated 20 000 children born with SCA annually2 (Figure 1). It is estimated that <50% of Ugandan children with SCA survive to their fifth birthday2 , whereas children with SCA in developed countries are excepted to live up to 60 years.3 Delayed diagnosis, difficulties in accessing adequate care, and a shortage of trained health care professionals contribute to the high rate of early mortality.
The prevalence of sickle cell trait across 112 districts in Uganda. The prevalence ranged from 2.5% to 23.9%.1
The prevalence of sickle cell trait across 112 districts in Uganda. The prevalence ranged from 2.5% to 23.9%.1
SCA is increasingly being recognized as an important cause of childhood morbidity and mortality in Ugandan children. This has led to an increase in the number of collaborative research studies on children with SCA and an overall increase in community awareness about SCA.
The Department of Paediatrics and Child Health, Makerere University, has a number of well-established collaborations with North American institutions that are leading to the development of research capacity in SCA. Each collaborator brings different skills to address critical questions of mutual interest in pediatric SCA research.
The following institutions are currently collaborating with the Department of Paediatrics and Child Health, Makerere University.
University of Montreal: sends a pediatric hematologist who spends 6 months each year working in the sickle cell clinic to train and mentor pediatric residents and hematology fellows.
Columbia University: established an exchange program for faculty with interest in SCA and research.
Indiana University (IU) and Cincinnati Children’s Hospital Medical Center (CCHMC): have 2 clinical trials currently evaluating new treatments for children with SCA. These two institutions collaborate with Global Health Uganda, a local multidisciplinary research and grants management organization.
Outcomes
University of Montreal/Makerere University collaboration
Development of written treatment guidelines for the management of SCA.
Created an electronic database for all SCA children attending the sickle cell clinic at Mulago National Referral Hospital, Kampala Uganda.
Faculty provides ongoing training and mentorship for pediatric residents and hematology-oncology fellows.
Columbia University/Makerere University collaboration
Established an exchange program for faculty to train local doctors on how to read and interpret transcranial Doppler scans to guide patient care.
Conducting research on central nervous system complications in SCA, which includes doing magnetic resonance imaging scans and treatment and follow-up of children.
An R21 grant was awarded to a Ugandan physician scientist to conduct the work, with the goal of applying for an R01 grant.
IU/CCHMC/Makerere University collaboration
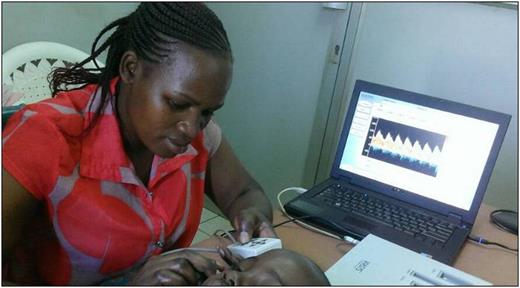
Trained a Ugandan technician to perform, read, and interpret transcranial Doppler scans with ongoing quality control monitoring by an expert reader at CCHMC. The technician is currently training others from across the country to work on other studies (Figure 2).
Provide critical training in data management and use of online databases.
Provide critical training in the design, implementation, conduct, and monitoring of clinical trials that are directly impacting policies regarding clinical care for SCA.
Established a research laboratory to perform immunological and molecular studies with an IU faculty member on site to provide training and mentoring to local investigators.
A study technician conducting a transcranial Doppler scan on a child with SCA.
Conclusions
International research collaborations with Makerere University have:
raised the profile of SCA research at Makerere University;
built research capacity leading to high-quality studies locally;
established relationships with leading experts from various western institutions;
produced results that are informing policy in caring for children with SCA;
expanded local expertise in the care and treatment of SCA; and
enabled local investigators to obtain independent research funding.
Future directions
Continue collaborating with the current and new institutions.
Initiate new clinical trials to inform the clinical management of children with SCA.
Change policies regarding SCA care, focusing specifically on SCA care in sub-Saharan Africa.
Acknowledgments: This work was supported by the Doris Duke Charitable Foundation (NOHARM and NOHARM/MTD studies, International Clinical Research Fellows), the Cincinnati Children’s Hospital and Medical Center, Indiana University, and a National Institutes of Health/Fogarty International Center NPGH Fogarty R25 Fellowship.
Conflict-of-interest disclosure: R.W.: Nova Laboratories (consultancy), Agios (membership on board of directors or advisory committees); Bristol-Myers Squibb (research funding); Addmedica (research funding); and Global Blood Therapeutics (consultancy). The remaining authors declare no competing financial interests.
Correspondence: Ruth Namazzi, College of Health Sciences, Makerere University, Kampala, Uganda; e-mail: namazzi101@gmail.com.