Relapse after CD19-directed chimeric antigen receptor (CAR) T-cell therapy remains a major challenge in B-cell acute lymphoblastic leukemia (ALL) and B-cell non-Hodgkin lymphoma (B-NHL). One of the main strategies to avoid CD19-negative relapse has been the development of dual CAR T cells targeting CD19 and an additional target, such as CD22 or CD20. Different methods have been used to achieve this, including coadministration of 2 products targeting 1 single antigen, cotransduction of autologous T cells, use of a bicistronic vector, or the development of bivalent CARs. Phase 1 and 2 trials across all manufacturing strategies have shown this to be a safe approach with equivalent remission rates and initial product expansion. CAR T-cell persistence remains a significant issue, with the majority of relapses being antigen-positive after CAR T-cell infusion. Further, despite adding a second antigen, antigen-negative relapses have not yet been eliminated. This review summarizes the state of the art with dual-targeting CAR T cells for B-cell ALL and B-NHL, the challenges encountered, and possible next steps to overcome them.
Introduction
In B-cell acute lymphoblastic leukemia (ALL), the first trials using CD19-directed chimeric antigen receptor (CAR) T cells1-5 showed response rates of ∼80% to 90% in a patient population that was previously unsalvageable with conventional therapies (Table 1). This led to licensing of tisagenlecleucel (tisa-cel) (Kymriah) for patients aged ≤25 years with B-cell ALL in 2018 and brexucabtagene autoleucel (Tecartus or KTE-X19) for patients aged >18 years in 2021. Since then, both trial and real-world data have shown that 40% to 50% of patients who respond to CAR T cells are cured without further therapy.6,12 Although most patients respond initially, ∼50% relapse after CAR T-cell therapy and have a poor prognosis. In B-cell non-Hodgkin lymphoma (B-NHL), the first multicenter trials targeting CD1913-18 showed complete response rates ranging from 40% to 74%, a practice-changing breakthrough in this highly chemorefractory population (Table 2). For large B-cell lymphoma (LBCL), 30% to 40% of patients have sustained responses with CAR T cells as a stand-alone therapy, and median progression-free survival ranges from 3 to 55 months.23,24 Pediatric real-world data in B-NHL show best sustained responses in B-cell lymphoblastic lymphoma histology.25 A detailed overview of the licensed products including axicabtagene ciloleucel (axi-cel), brexucabtagene autoleucel, tisa-cel, and lisocabtagene maraleucel has recently been published.26
Relapse after CAR T-cell therapy follows 2 main patterns: CD19-positive (CD19+) relapse, usually due to poor CAR T-cell persistence, and CD19-negative (CD19–) relapse due to antigen escape or lineage switch,27,28 although other mechanisms have been described.29 The ELIANA study for B-cell ALL reports predominant CD19– relapses (48%), with very few CD19+ relapses (6%).4,6 In contrast, real-world studies have shown higher rates of CD19+ relapses vs CD19– relapses (ie, 60% vs 30% in a UK national study12 or 58% vs 42% in data from the Pediatric Real-World CAR Consortium30). Prerelapse and postrelapse sample analysis on the ZUMA-1 study in B-NHL also showed a higher proportion of CD19+ relapses (∼64%).13
To infer persistence, B-cell aplasia in peripheral blood is most commonly used as a surrogate marker.3,4,9 Data from studies with tisa-cel suggest that recovery of B cells before 6 months from infusion is associated with a higher risk of relapse and warrants therapeutic intervention.6,28 Early loss of CAR T-cell persistence may reflect either intrinsic factors making CAR T cells less “fit” (including CAR design, the memory phenotype of the starting material, and production methodology),31,32 CAR T-cell exhaustion in vivo,33,34 or immune-mediated rejection.5,32,35 Currently, it is not known which of these is the dominant cause of early loss of CAR T cells in patients with ALL.
Resistance to CD19-targeted CAR T cells may also result from loss or downregulation of CD19 surface antigen expression due to acquired mutations or splice site alterations.27,36 Incorporating an additional target represents a logical strategy to overcome this challenge given that a single leukemic stem cell is unlikely to lose or downregulate 2 antigens simultaneously.
In this article, we focus on the different strategies used to deliver dual-targeting CAR T cells to patients and review the published data on construct design, toxicity, expansion, response rates, relapse incidence, and outcomes following dual-targeting CAR T cells for B-cell ALL and B-NHL.
Dual antigen–targeting CAR T cells
Potential targets
CD19 is almost universally expressed at high antigen densities on B-cell ALL blasts.37,38 However, its expression is more variable in B-NHL. Certain types of lymphoma, such as diffuse LBCL or follicular lymphoma, can show diminished surface levels of CD19 and significant interpatient variability.39,40
CD22 is also almost always expressed in B-cell ALL with the exception of a proportion of patients with infant ALL.41 In B-cell ALL, treatment with CD22 CAR T cells alone has shown robust expansion and high complete remission (CR) rates.10,11,42,43 However, high rates of relapse due to downregulation of CD22 expression were observed, unless used as a bridge to allogeneic hematopoietic stem cell transplantation.10,11 This suggests that the ability of CD22 CAR T cells to recognize targets with low antigen density may be critical. In the B-NHL patient population, single-targeting CD22 CAR T cells have also been explored.22 However, CD22 expression seems to be more variable in the range of 60% to 85% CD22-positive cases depending on histology,44 and this could potentially impact efficacy.
CD20 is another possible target, expressed on most B-NHL and ∼40% to 50% of B-cell ALL. CAR T cells targeting CD20 have been developed for B-NHL.19-21 Importantly, although CD20-targeted therapy (rituximab) is used throughout B-NHL therapy, malignant cells rarely seem to lose or downregulate CD20.45
Several trials are underway using different manufacturing methods with CAR T cells targeting CD19 and CD22, or CD19 and CD20, which are reviewed herein.46,47 Indeed, some groups are exploring targeting all 3 antigens, and preclinical xenografted leukemia and lymphoma models have shown superior activity with this trispecific approach.48
Strategies for delivery of dual-targeting CAR T cells
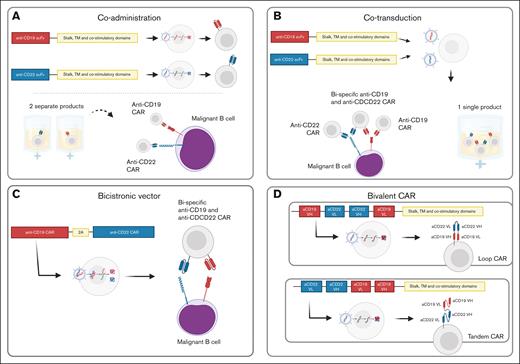
There are currently 4 main strategies to deliver dual-targeting CAR T cells to patients (Figure 1): coadministration, cotransduction, use of bicistronic vectors, and bivalent tandem CARs. Each has different advantages and disadvantages, summarized in Table 3.
Strategies for delivery of dual-targeting CAR T cells. CD19 and CD22 are shown as an example of antigenic targets. (A) Coadministration: 2 independent products are generated and infused into patients. (B) Cotransduction: T cells are transduced with 2 different vectors, generating 1 single product with a mixed population of single antigen–targeted and bispecific CAR T cells. (C) Bicistronic vector: 1 single vector with binding domains for 2 different antigens is used. The vector is then cleaved and generates CAR T cells with 1 CAR for each antigen on their surface. (D) Bivalent tandem CAR: 1 vector generates 1 single CAR on the surface of the cell. That CAR has binding domains for 2 different antigens. TM, transmembrane; VH, variable heavy chain; VL, variable light chain.
Strategies for delivery of dual-targeting CAR T cells. CD19 and CD22 are shown as an example of antigenic targets. (A) Coadministration: 2 independent products are generated and infused into patients. (B) Cotransduction: T cells are transduced with 2 different vectors, generating 1 single product with a mixed population of single antigen–targeted and bispecific CAR T cells. (C) Bicistronic vector: 1 single vector with binding domains for 2 different antigens is used. The vector is then cleaved and generates CAR T cells with 1 CAR for each antigen on their surface. (D) Bivalent tandem CAR: 1 vector generates 1 single CAR on the surface of the cell. That CAR has binding domains for 2 different antigens. TM, transmembrane; VH, variable heavy chain; VL, variable light chain.
Coadministration
Two separate single antigen–targeting CAR T-cell products are generated and infused into patients. Two different vectors are used (1 encoding a CD19, the other a CD22 or CD20 CAR) and transduced into T cells separately. Then, the 2 products can be pooled together,50 infused separately on the same day,51 on sequential days,52-54 or >1 month apart.55-57
Cotransduction
T cells are transduced with 2 different vectors at the same time, generating a mixed population of single- and dual-targeting CAR T cells.
Bicistronic vector
T cells are transduced with 1 single bicistronic vector with antigen-binding domains for both antigens. This results in a homogeneous population of CAR T cells with 2 separate CARs expressed at an equimolar concentration on their surface.
Bivalent tandem CAR
In this case, T cells are transduced with a bivalent vector that generates 1 single CAR on the surface of the cell. It has 2 binding domains, and the variable light and heavy chains of the single-chain variable fragment (scFv) can be set up in a sequential or loop design.47
Review of current trials using dual targeting for relapsed/refractory B-cell ALL
The major studies are summarized in Table 4.
CAR constructs and manufacture
Multiple CAR designs and strategies have been applied for B-cell ALL. For example, Wang et al53 applied third-generation CARs with both 4-1BB and CD28 as costimulatory molecules, and Cordoba et al49 used humanized scFvs in their bicistronic vector. Ghorashian et al60 used the previously reported5 CAT CAR backbone, designed with lower affinity to the CD19 antigen in combination with a novel CD22 CAR based on the 9A8 binder, which recognizes the target’s expression of CD22 at low antigen densities.67 Tandem CARs have generally used the murine anti-CD19 FMC63 scFv and the human anti-CD22 m971 scFv, with variations in the arrangements of light and heavy chains. Because of these differences in CAR design, it is difficult to generalize observed differences in outcomes between the varying dual-targeting strategies above or to attribute these specifically to the approach used.
CAR T cells were manufactured using both closed49,62,66 (such as the CliniMACS Prodigy system) and open50,57,60 processing procedures, variable sources of activation beads (CD3/CD28 dynabeads or TransAct), variable cytokines (eg, Cordoba et al49 adding interleukin-7 [IL-7] and IL-15 and Ghorashian et al adding no cytokines60), and durations of manufacture. These variables may impact the phenotype of the final CAR-T product, which may in turn affect persistence (see “Summary and future directions”).
Toxicity
Toxicity observed in trials in B-cell ALL is summarized in Table 5. In general, the published data do not suggest increased toxicity with the addition of a CD22-targeting construct. CAR-related toxicities were mild to moderate (grade 1-2) in most patients. The rate of grade 3 to 4 cytokine release syndrome ranged from 0% to 28.4% and from 0% to 17.6% for neurotoxicity (immune effector cell–associated neurotoxicity syndrome), which is comparable to single targeting. Previously reported70 immune effector cell–associated hemophagocytic lymphohistiocytosis–like syndrome after single antigen–targeted CD22 has not been widely observed, except in the series of Spiegel et al,62 in which 2 cases of immune effector cell–associated hemophagocytic lymphohistiocytosis-like syndrome were observed using a tandem construct.
Expansion of CAR T cells
Regardless of strategy, most clinically tested dual-targeting CAR T-cell products have shown initial expansion kinetics and peak levels broadly similar to those observed with tisa-cel.7,71 A 2022 study from Shanghai50 pooled 2 different CAR T-cell populations together at a 1:1 ratio and saw an earlier and higher peak expansion of CD19 CAR T cells compared with CD22 CAR T cells.
With the cotransduction method, expansion of different CAR T-cell populations can vary widely. During manufacture, T cells are exposed to 2 lentiviral vectors and therefore have different transduction efficiencies. Products can therefore be balanced or skewed toward a certain CAR component. Ghorashian et al60 reported a product composition with predominantly CD19/22-CAR expressing cells (median, 54.4%) with lower but balanced CD19-CAR (13%) and CD22-CAR (11.6%) components. After infusion, early in vivo expansion reflected the phenotype of the product with predominant engraftment of CD19/22 double-transduced T cells and balanced but lower engraftment of CD19 and CD22 single-positive populations. In contrast, early reports from the PLAT-05 study showed a skewed in vivo expansion of the CD19-CAR component using the CAR19x22v1 product.58 In view of this, the manufacturing methodology was altered to favor the CD22 CAR T cells in the product. However, when this was infused, in vivo expansion was then skewed toward the CD22-CAR component.59
The use of bicistronic vectors does not seem to impact early expansion, with Cordoba et al49 reporting expansion similar to that of tisa-cel.7,71 However, data from studies by the National Cancer Institute and Stanford62,66 indicated limited expansion and shorter persistence of their tandem CD19/22 CARs compared with their single antigen–targeted CD22 CAR.
Response
All studies showed minimal residual disease–negative CR or CR with incomplete recovery rates >80%, mirroring the clinical experience with CD19-directed CAR T-cell therapy so far. The only product with lower rates of reported response (57%) was the first product tested in the PLAT-05 study using a cotransduction approach.58 Coadministration strategies showed particularly favorable responses, with CR rates >90%. Given that bridging chemotherapy is generally used before lymphodepletion, we cannot attribute responses to CAR T cells alone. However, given the refractory nature of the durability of responses in many such patients, it is unlikely that bridging therapy contributes significantly to response rates.
Relapse incidence and phenotype
Regardless of the strategy used, antigen-positive relapse has been the predominant cause of treatment failure observed following dual-targeting CAR T-cell therapy, reflecting poor persistence across a substantial number of dual-targeting CAR products.49,50,57,60,62,66
Antigen-negative relapse has still been observed in most studies of dual-targeting CAR T cells in B-cell ALL (see Table 4, column “Relapse phenotype”). CD19– relapse with ongoing CD22 positivity is the main phenotype, perhaps reflecting the poor performance of the CD22 CAR across the different strategies, shorter persistence in coadministration,50 and stronger selective pressure on the CD19 compared with the CD22 target in bicistronic and tandem CARs.49,62 Consequently, CD22 negativity is rarely observed. It is important to highlight that because prolonged selective pressure is needed for outgrowth of antigen-negative clones, poor persistence may limit our ability to assess the real prevalence of antigen-negative relapse.
Outcomes
Clinical outcomes with dual-targeting CAR T cells in B-cell ALL have generally been equivalent to those reported with the single-targeting CD19 CAR.4-6,12
The most encouraging results have been achieved with coadministration of CD19 and CD22 CAR T cells. One of the 2 largest studies50 of this approach reports a 12-month event-free survival (EFS) of 74%. They used a short manufacture time (7 days) and infused a fresh, 1:1 pooled product of CD19 and CD22 CAR T cells to 225 patients. Although these results appear superior to data on tisa-cel reported in the ELIANA trial6 and real-world data,12,72 it should be noted that the patient characteristics in this study were more favorable, with 32% of patients being minimal residual disease–negative before infusion. Pan et al57 have also shown impressive outcomes, with an 18-month EFS of 79%. In this study, CD19 CAR T cells were infused first, followed 30 days later by a CD22 CAR T-cell infusion for patients in complete remission and without ongoing toxicities. Interestingly, CD22 CAR T cells expanded and persisted despite eradication of disease with the previous CD19 CAR T cells. Further, disease surveillance presumably relied on the CD22 CAR T cells given that many patients lost their CD19 CAR T cells after receiving a second cycle of lymphodepleting chemotherapy.
Using a cotransduction approach, the CARPALL cohort 3 study by Ghorashian et al60 reported a 12-month EFS of 60%. Although data need to be interpreted with caution because of the small sample size, antigen-negative relapse was not observed. This may in part reflect the use of CD22 CAR based on the 9A8 binder, which effectively targets tumor cells at low CD22 antigen density. Initial and sustained response was observed in 2 out of 3 patients who had CD19-negative disease on enrollment, demonstrating effective CD22 CAR activity. Additionally, single antigen–targeted CD22 CAR T cells were detectable in blood for longer (median of 7 vs 5 months) than their single CD19 and double CD19/CD22–targeting CAR T-cell counterparts.
Cordoba et al49 reported a lower EFS using CAR T cells transduced with a bicistronic CD19-22 CAR vector (AUTO3), with a median EFS of 5 months and 12-month EFS of 32%. They observed a high rate of antigen-positive relapses associated with CAR T-cell loss, and short persistence was considered to be the main factor for these poor results. The authors postulate that this replicated a differentiated phenotype of the CAR T-cell product, which in turn may reflect the production methodology used. However, it is also possible that signaling through 2 CARs in a single cell may predispose to activation-induced cell death and/or exhaustion.33
Using a tandem CD19-22 CAR, Spiegel et al62 reported a median EFS of 5.8 months and Shalabi et al66 a 12-month EFS of 58% in responding patients. These somewhat disappointing outcomes mirror the issues that both groups encountered with the functionality of CD22 targeting in the context of a tandem CAR structure. In the adult cohort of Spiegel et al,62 they showed that CD19/22 tandem CAR T cells had reduced cytokine polyfunctionality following stimulation with CD22-positive targets compared with T cells transduced with a CD22 CAR alone. Shalabi et al66 showed suboptimal CD22-targeting activity of the tandem CAR construct, both in vitro, with reduced cytokine secretion against CD19-CD22+ Nalm6 cell lines, and in vivo, with poor antileukemic activity in a xenogeneic CD19-negative, CD22-positive model of B-cell ALL. These data indicate decreased functionality of the CD22 CAR moiety when incorporated into a tandem structure.
Cui et al64 reported better results in a cohort of 47 patients (24-month EFS of 69%) using a tandem CAR construct, but these results need to be interpreted with caution given that 75% of patients underwent consolidative allogeneic hematopoietic stem cell transplantation at 2 months.
Review of current trials using dual targeting for relapsed/refractory LBCL
CAR constructs and manufacture
Constructs used for B-NHL are more homogeneous than those used in B-cell ALL. Tandem CARs targeting CD19 and CD20 used sequences derived from the murine scFv regions Leu-16 for CD20 and FMC63 for CD19.51,73,74,76 As for CD19 and CD22, the studies on coadministration from Wuhan52,53,78 all applied a third-generation CAR with 4-1BB and CD28 as costimulatory molecules. Roddie et al79 used 2 humanized scFv regions in a bicistronic vector: LT22 for CD22 and HD37 for CD19, the same product (AUTO3) Cordoba et al49 used for B-cell ALL. Tandem CARs targeting CD19 and CD22 use the same scFv as described for B-cell ALL, FMC63 for CD19 and m971 for CD22, in a second-generation backbone.62,80,81
In terms of manufacturing, as with B-cell ALL, processing procedures varied across studies. Larson et al73 specifically enriched the apheresis product for CD62L to obtain a higher yield of naïve and memory T cells. They extended the expansion period to 12 to 16 days before cryopreserving the final product. Manufacturing times varied from 8 to 14 days. Although shortened manufacturing methodologies, such as the T-Charge platform, have been used with CD19-directed CAR T cells,83 they have not yet been applied to dual-targeting CAR T cells.
Toxicity
The toxicity profile across the reviewed trials for B-NHL is summarized in Table 8. There does not seem to be any increased toxicity when adding CD20 or CD22 antigen recognition. Grade 3 to 4 cytokine release syndrome occurred in 0% to 28.5% of cases, and grade 3 to 4 immune effector cell–associated neurotoxicity syndrome was reported in 0% to 13.6% of cases across all studies. Larson et al73 reported a relatively low incidence of adverse events in their trial. They noted low peak cytokine levels while maintaining clinical efficacy of their CAR T-cell product. This could be explained by the skewed naïve/memory T-cell phenotype achieved during production, or the thorough preclinical construct optimization,84 leading to increased clinical efficacy and consequently allowing for a lower CAR T-cell dose (median of 55 × 106 cells).
Expansion of CAR T cells
Despite using more complex constructs, CAR T cells expand well and peak at ∼2 weeks, with a tendency toward greater expansion in patients who show a response.74,76,81 Persistence, however, has been reported to be very short in the B-NHL cohort. CAR T cells are lost earlier compared with the B-cell ALL population, with most trials reporting 3- to 6-month persistence.75,77,79,81 As observed with single antigen–targeting CAR T cells, it is not clear if a shorter persistence correlates with relapse in the B-NHL cohort. An early, greater expansion might be more significant for durable remission in lymphoma75 compared with B-cell ALL.
Response
Overall response rates range from 60% to 90% across different trials, whereas CRs range from 29% to 81%. These numbers do not differ significantly from the responses observed with single antigen–targeting CAR-T trials.26 Deep initial responses with dual-targeting CAR T cells seem to correlate with durable remissions,53 as has also been observed with single antigen targeted CAR T-cell therapy.26 Shah et al74 report a trend toward a greater proportion of naïve and central memory phenotypes in the apheresis products of patients who showed good clinical response. Although bridging therapy is frequently used in B-cell ALL, its use in B-NHL has varied historically in pivotal trials, and also varies across dual-targeting studies, with some studies not giving any,51,76,80 others permitting its use at each center’s discretion,50,62,78 and some reporting its use as part of the study protocol.73,74,79 Roddie et al79 commented on the role of effective bridging in debulking disease before CAR T-cell infusion and how low disease burden was a predictor of response to their product, AUTO3. Conversely, Zurko et al75 found inferior survival in patients who required bridging therapy, which may reflect higher disease burden on recruitment.
Relapse incidence and phenotype
In lymphoma, a biopsy is needed to assess antigen expression on tissues, often with patchy lymphoma involvement, which makes representation of CD19 and CD20/CD22 expression at baseline and relapse more challenging. Modalities to assess pre- and postrelapse antigen expression include the H-score62,85 and flow-based assessment of fine-needle aspiration material.62 From the available data,62,74,79,85 relapses seem to follow the same phenotype as with B-cell ALL. Most relapses retain expression of CD19 and CD22/CD20, as has been the case with CD19-targeted products. For example, in the ZUMA-1 trial, one-third of LBCL relapse cases after axi-cel administration were due to antigen loss, and two-thirds of cases relapsed with ongoing CD19 expression.13 In most patients with lymphoma, CAR T cells do not persist long-term, and this may account for antigen-positive relapse in some cases. However, other factors may also be contributory. Certainly, T-cell fitness and the functionality/expansion potential of CAR T cells in vivo play important roles in the achievement of clinical response. Thus, antigen-positive relapse is more likely when the CAR T-cell product is intrinsically unfit because of prior chemotherapy. Moreover, endogenous immune and tumor microenvironment-associated factors may impede T-cell function in vivo and contribute to the risk of antigen-positive relapse.29
Despite dual targeting, there are still some observed cases of suspected clonal escape with downregulation of CD19 and CD20/CD22 antigen expression.77,79 Given that exhaustion is another of the proposed mechanisms of CAR T-cell treatment failure, some studies have attempted adding checkpoint inhibitors after CAR T-cell infusion. Results are mixed. Roddie et al79 observed no clear benefit in adding pembrolizumab on day 14 after the administration of dual CAR T cells, in line with the ZUMA-6 results.86 However, Zhang et al82 reported improved response rates and progression-free survival with addition of the PD-1 inhibitor tislelizumab on day 1 after infusion.
Outcomes
Results varied regarding outcomes, with some studies reporting lower EFS and others superior EFS compared with the pivotal trials, as depicted in Tables 4 and 5.
The study by Cao et al52 using high-dose therapy with autologous hematopoietic stem cell infusion followed by CD19 and CD22-targeted CAR T cells showed a 24-month EFS and overall survival of 83%, which exceeds the outcomes of high-dose therapy alone (∼30%-40%)87 or those reported in the CD19-directed studies.18,23,25,88 It should be noted, however, that the patient population in this study was predominantly aged <50 years (73%) and transplant-naïve. Additionally, it is a complex approach that requires 2 apheresis procedures (one with stem cell mobilization) and involves toxic myeloablative conditioning.
Roddie et al79 used a bicistronic vector targeting CD19 and CD22, and they encountered issues similar to those reported in the B-cell ALL cohort with short persistence (perhaps reflecting the differentiated phenotype of the product), leading to a lower EFS of 25% at 12 months. However, effective CD22 targeting can be inferred because 7 out of 13 cases downregulated CD22 at relapse.
With tandem products, Spiegel et al62 reported an EFS of 25% at 12 months in their B-NHL cohort, and the potential reasons for these poor outcomes have been discussed in “Outcomes” of “Review of current trials using dual targeting for relapsed/refractory B-cell ALL”. Larson et al73 produced CD19-20 tandem CAR T cells through bead-based enrichment of CD62L expression, generating a final product skewed toward naïve and memory T cells. They reported an EFS of 40% at 18 months. Activity of the tandem construct against the 2 antigens did not seem to be impaired, with reports of high overall responses and CAR T-cell persistence over 6 months.
A group in Wisconsin74,75 also designed a CD19-20 tandem construct and reported outcomes equivalent to those of single-antigen targeting, with an EFS of 44% at 24 months. In CAR-naïve patients with diffuse LBCL, EFS increased to 50%. For patients who showed an initial CR and then relapsed (6/12), the relapses occurred late (>180 days), which is not the usual pattern observed with tisa-cel23 or axi-cel.13 Early expansion seems to correlate with durable responses, as suggested by this study,75 data from the CD19 National Institutes of Health (NIH) product with a CD28 costimulatory domain,24 and data from ZUMA-1 with axi-cel.88 Regarding patterns of resistance, Shah et al74 highlighted a patient who relapsed with detectable circulating CAR T cells and available relapse biopsy material. When cocultured in vitro, frozen CAR T cells were able to kill CD19+/CD20+ Raji cells, but did not show any activity against bright CD19+/CD20+ biopsy material. This suggests other mechanisms of resistance in the tumor microenvironment in B-NHL beyond antigen loss or downregulation.
Finally, a group from Beijing76,77 performed detailed in vitro screening of different tandem CAR construct candidates by measuring F-actin accumulation at the immunological synapse (IS) and polarization of the microtubule-organizing center.76 TanCAR7 proved to have the most stable IS and delivered the most effective target cell lysis, and was thus selected for further in vivo studies. In a phase 1 to 2 study of TanCAR7 in 87 patients with B-NHL, they reported an EFS of 61% at 12 months with a median EFS of 27.6 months. Median persistence duration was ∼100 days, and no significant difference was observed between patients who relapsed and those who maintained a response. Interestingly, of the 12 patients with available postrelapse biopsy samples, 5 patients still had detectable CAR T cells in the tissue, but only 1 showed CD19 and CD20 antigen loss.
Summary and future directions
In comparison with the experience with single-antigen CD19-targeting CAR T cells, dual-targeting strategies have shown equivalent initial expansion rates and have proven to be a safe approach with an equivalent toxicity profile. To date, the current generation of dual-targeting CAR T-cell studies have not resulted in significantly improved outcomes compared with targeting CD19 alone. This may reflect both the heterogeneity in approaches used and the fact that dual targeting per se does not address other mechanisms of resistance besides antigen escape. Nonetheless, important lessons have been learned.
If a CD22 CAR is used, it needs to target low antigen density
Cotransduction can lead to skewed in vivo expansion
Different transduction efficiencies can lead to heterogeneous products (of CD19, CD22, and CD19/22 CAR T cells) that can further show skewed and unpredictable expansion of the different cellular components in vivo.
Designing a tandem CAR that functions optimally for both targets is challenging
With a variety of possible designs and conformations, it has proven difficult to optimize function against 2 different antigens, perhaps reflecting differences in the distance of the epitopes from the cell membrane. Studies exploring size and rigidity of the CAR construct84 or the stability of the IS76 have proven useful in selecting CARs with the most effective target cell lysis, but in vitro assays do not necessarily recapitulate functionality in vivo.
It is possible that expression of 2 CARs on the surface could trigger cell death
The clinical application of bicistronic vectors has led to products with a differentiated T-cell phenotype and a high proportion of early CAR T-cell loss. It is possible that expressing 2 CARs on a single cell could accelerate activation-induced cell death and/or exhaustion. Further studies are needed to investigate this possibility: if this is the case, coadministration may be preferable to bicistronic or cotransduction approaches. Indeed, on the basis of the available data at present, coadministration strategies have shown the most promising outcomes in B-cell ALL.
Evasion mechanisms by malignant cells and their microenvironment could be a major barrier for the success of dual-targeting CAR T cells
Although poorly characterized, studies hint at other mechanism of disease resistance aside from loss of persistence and antigen loss/downregulation. For example, Zhang et al77 describe 4 patients with relapsed B-NHL and antigen positivity despite persisting CAR T cells in the biopsied tissue. Possible causes for such cases could be the inhibition by regulatory T cells and myeloid-derived suppressor cells in the bone marrow microenvironment,29 upregulation of immune checkpoint molecules via mutations in the IL-6/JAK/STAT3 signaling pathway,89 abnormalities in the apoptotic pathway,90 downregulation of cyclic GMP-AMP synthase-stimulator of interferon genes (cGAS-STING) pathway signaling,91 or production of adenosine by tumor cells.92
Poor CAR T-cell persistence remains a key challenge
Several mechanisms underlying poor CAR T-cell persistence have been suggested, such as poor CAR T-cell fitness, exhaustion, and immune rejection of the product.
Regarding CAR T-cell fitness, clones derived from naïve populations (T naïve and T stem cell memory) are considered to play a critical role in long-term functional CAR T-cell persistence.31,93 Biasco et al31 showed that stem cell memory T-cell subpopulations contributed the most to the clonal pool at late time points of patients with long-term persisting CAR T cells. Some strategies to improve the functionality of the product include optimizing CAR design by reducing the affinity of CAR-T binding to antigens5; using CD3 zeta domains with fewer immunoreceptor tyrosine-based activation motifs (ITAMs)94; shortening the duration of ex vivo culture83,95; using AKT inhibitors96,97; or modifying the culture medium by including IL-21,98 increasing the potassium concentration,99 or adding N-acetylcysteine.100
Exhaustion has been suggested as a possible mechanism through methylation profiling of CD19 CAR T cells after infusion.34 Addition of checkpoint inhibitors in the B-NHL population has yielded mixed results. Reinfusion of CAR T cells followed by nivolumab is currently being investigated (NCT05310591), while there are preclinical studies on gene-edited CAR T cells with downregulation of DNMT3A101 or PRDM1.102
Finally, immunogenicity of the CAR product must be considered given that most CAR T cells use an antigen recognition domain derived from murine antibodies. Turtle et al32 observed no expansion or persistence after CD19-targeted CAR T-cell reinfusion in adult patients with B-cell ALL despite the use of lymphodepleting chemotherapy in 4 out of 5 patients. They were able to demonstrate CAR-specific cytotoxic T-cell responses in an in vitro model and define possible antigenic epitopes within the CAR construct. Immune-mediated rejection may explain the relatively low rate of long-term responses to reinfusion of tisa-cel for early B-cell recovery.103 Given that dual-targeting products incorporate 2 scFvs and are frequently given after single-antigen targeted CAR T-cell therapies with mostly the same constructs, there is an increased potential for immune-mediated rejection, and immunogenicity should be monitored. Humanization of CARs104 and optimizing exposure to fludarabine105,106 are being explored as strategies to reduce CAR T-cell rejection.
Importantly, although there is strong evidence that persistence is key for durable remissions in B-cell ALL,28,107-109 this is not as well established in B-NHL. Interestingly, most patients with LBCL still relapse with antigen-positive disease following CAR T-cell therapy, which warrants further investigation if products with longer persistence profiles could deliver more durable responses in LBCL.
Future directions
Although dual targeting has not yet fully eradicated CD19– relapse or improved outcomes, the studies to date have given important insights into the challenges to overcome. Building on these lessons, the next generation of dual-targeting CAR T-cell studies are well placed to fully achieve the potential of this approach. Subsequent studies should use CD22 CARs that recognize low antigen density targets and incorporate strategies to enhance CAR T-cell persistence. For example, in our next study in pediatric B-cell ALL, we plan to combine optimized lymphodepletion with fludarabine therapeutic drug monitoring with the use of CAR T cells transduced with CD19CAR and CD22CAR vectors separately generated with a rapid manufacturing protocol. Such approaches may increase the regulatory complexity and cost of CAR T cells; however, if they achieve sufficiently improved long-term outcomes relative to existing licensed products, this investment will be justified. Moreover, as we move forward, the lessons learned in dual targeting of B-lineage ALL and non-Hodgkin lymphoma may provide important insights on how to best deliver dual-targeting CAR T cells for other malignancies.
Authorship
Contribution: G.d.O.C. prepared the manuscript draft, tables, and figures; C.R. and P.J.A. reviewed and contributed to the final version of the manuscript; and P.J.A. supervised the writing process.
Conflict-of-interest disclosure: C.R. has served on advisory boards of and/or received honoraria from Kite/Gilead, Novartis, Autolus, Johnson & Johnson, Bristol Myers Squibb, Cellistic, and Kyverna. P.J.A. has received research funding and patent royalties from Autolus Therapeutics PLC. G.d.O.C. declares no competing financial interests.
Correspondence: Persis J. Amrolia, Molecular and Cellular Immunology Section, Great Ormond Street Institute of Child Health, 20c Guilford St, London WC1N 1DZ, United Kingdom; email: persis.amrolia@gosh.nhs.uk.