Key Points
Donor age should be prioritized over HLA-DPB1 matching in patients undergoing 10/10-HLA matched unrelated donor HCT.
HLA-DPB1 matching is associated with relapse and nonrelapse mortality within younger, but not older, donor groups.
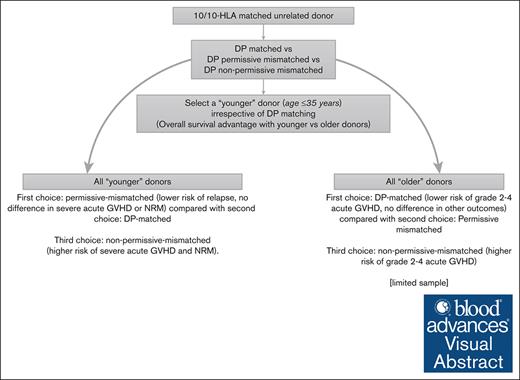
Visual Abstract
In 10/10 HLA-matched unrelated donor (MUD) hematopoietic cell transplantation (HCT) with calcineurin-inhibitor (CNI)-based prophylaxis, T-cell epitope DP-matched and permissive mismatched donors are associated with similar overall survival (OS) whereas donors with nonpermissive mismatches should be avoided. Younger unrelated donors are also favored over older donors. We explored outcomes associated with different combinations of DP-matching and donor age (dichotomized at 35 years) to further guide donor selection. Using a Center for International Blood and Marrow Transplant Research data set, we categorized 10 783 patients into 6 groups: DP-matched/younger donor (n = 1591), DP-matched/older donor (n = 526), permissive-mismatched/younger donor (n = 3845), permissive-mismatched/older donor (n = 1184), nonpermissive mismatched/younger donor (n = 2659), and nonpermissive mismatched/older donor (n = 978). We noted that younger donor age, rather than DP matching, was associated with better OS. Younger donors with permissive mismatches were associated with improved OS compared with older matched donors. Furthermore, younger donors with nonpermissive mismatches were associated with improved OS compared with older donors with permissive mismatches. Our study adds further information about the association of DP matching and donor age with HCT outcomes. Donor age should be prioritized over DP matching in patients undergoing 10/10 HLA-MUD with CNI prophylaxis. Among those with younger donors, permissive-mismatched or DP-matched donors are preferred over nonpermissive mismatched donors.
Introduction
For patients undergoing HLA-matched unrelated donor (MUD) hematopoietic cell transplantation (HCT), additional matching at the HLA-DPB1 (major histocompatibility complex, class II, DP beta 1) has further prognostic implications.1-4 Although prior studies indicated a lower relapse risk for both permissive and nonpermissive T-cell epitope (TCE) mismatches compared with DPB1-matched transplants, only nonpermissive mismatches were associated with a significantly increased risk of nonrelapse mortality (NRM).1,2 Consequently, nonpermissive mismatches resulted in poorer overall survival (OS) compared with DPB1-matched recipients, whereas OS was similar between DPB1-matched and permissive-mismatched cases. Therefore, guidelines from the National Marrow Donor Program and the Center for International Blood and Marrow Transplant Research suggest avoiding nonpermissive mismatched donors and selecting either DPB1-matched or permissive-mismatched donors, with no preference for either.5
Donor age is also, however, a significant predictor of survival.6-12 When multiple donors with different combinations of donor age and DP-matching are available, 1 factor may be favorable and the other unfavorable. Donor selection in such situations becomes a matter of clinical judgment to weigh the favorable and unfavorable donor characteristics to select a final donor. Therefore, we undertook this study to analyze the outcomes of 10/10-HLA MUD taking both DP matching and donor age into consideration. Considering the hierarchy of DP matching from the “best” to the “worst” as DP matched, followed by permissive mismatched, and then nonpermissive mismatched, we hypothesized that the “better” matched category with older donor group would be associated with an inferior OS than the “lesser” matched younger donor group. Hence, a younger DP-matched or permissive-mismatched MUD would be associated with the best OS of all groups and should be favored.
Methods
We performed a secondary analysis of data from the referenced publication13 using a publicly available Center for International Blood and Marrow Transplant Research data set.14 The local institutional review board (FHIRB0020181) approved the study, which was conducted in accordance with the Declaration of Helsinki. The study population included patients with acute myeloid leukemia, acute lymphoblastic leukemia, or myelodysplastic neoplasm who underwent a 10/10-HLA MUD between 2008 and 2018. All patients received calcineurin inhibitor (CNI)-based prophylaxis. Posttransplant cyclophosphamide (PTCy)-based prophylaxis was not included in the data set. Following the categorization scheme of the original study,1 HLA-DPB1 matching was classified into 3 groups: matched, permissive mismatched, and nonpermissive mismatched. This classification is based on the TCE model.3 Specifically, donor–recipient pairs that were matched at HLA-DPB1 were labeled “DP-matched,” whereas those with HLA-DPB1 permissive mismatches were labeled as “permissive mismatched.” Those with HLA-DPB1 nonpermissive mismatches were labeled as “nonpermissive mismatched” regardless of whether the mismatch was in the host-versus-graft (HVG) or graft-versus-host (GVH) direction because the directionality does not significantly affect the outcomes.15
Baseline characteristics were summarized using descriptive statistics, with median and interquartile range for continuous variables and numbers/percentages for categorical variables (Table 1). These were compared between the groups using the χ2 test for categorical variables and the Mann-Whitney U test for continuous variables. Our primary outcome of interest was OS. Secondary outcomes included grade 2 to 4 and grade 3/4 acute GVH disease (GVHD), chronic GVHD, relapse, and NRM. In univariate analysis, the Kaplan-Meier method was used to estimate OS probability. The cumulative incidence method accounting for competing risks was used to estimate the incidences of GVHD, NRM, and relapse. Competing risks considered were death for GVHD; disease relapse for NRM; and death before relapse (NRM) for relapse. The probabilities of outcomes at 48 months are reported, except for acute GVHD (reported at day 100) and chronic GVHD (reported at 24 months). Multivariable analysis (Table 2) was performed using Cox proportional hazards models. Cause-specific hazards are reported for all outcomes with competing events. An overall 2-sided P value <.05 was considered significant for the main models. Additionally, we performed direct pairwise comparisons to compare each DP-match level with 1 another in the entire population and within both the younger and older donor groups. This led to 9 predetermined pairwise comparisons (outlined in Table 3). However, to account for multiple comparisons across all 15 potential combinations, a Bonferroni corrected P value of ≤.05/15 (≤.0033) was considered significant for these analyses. All variables were tested to affirm the proportional hazards assumption by including a time interaction of the variable(s) in the model and assessing graphically. No significant interaction effects were noted between the main effect and other statistically significant covariates in multivariable regression analyses.
Results
Of 14 147 patients, 3364 (23.8%) were excluded because of missing DP-matching data. Donor age data were available for all. First, we investigated the independent effects of DP-matching (matched [n = 2117], permissive mismatched [n = 5029], nonpermissive mismatched [n = 3637]) and donor age on outcomes in multivariate models. Both donor age and DP match were significant predictors of relapse and NRM. Patients with permissive or nonpermissive mismatches had a lower risk of relapse compared with the DP-matched cases. For NRM, only nonpermissive mismatches were associated with a higher risk compared with DP-matched cases (supplemental Table 1). In contrast, for OS, donor age as a continuous variable was a significant predictor (hazard ratio [HR], 1.01; 95% confidence interval [CI], 1.007-1.012; P < .001) whereas DP matching was not. When donor age was categorized by 5-year increments (<25 years, 25-29.9 years, 30-34.9 years, and so forth), there was no difference in OS in the first 3 groups, whereas it increased in the subsequent groups. Moreover, donor age as a continuous variable had no significant impact on OS in patients with donors aged ≤35 years. Also, several previous publications that showed a survival advantage with generally younger donors particularly, between the ages of 30 and 36 years, compared with older donors.7-12 After the categorization of donor age, the independent effects of donor age and DP matching were examined, and similar findings were noted. There was no significant interaction between DP matching and donor age (supplemental Table 1).
Next, of 10 783 patients with available DP data, 6 groups were created as follows: DP-matched/younger donor (n = 1591), DP-matched/older donor (n = 526), permissive-mismatched/younger donor (n = 3845), permissive-mismatched/older donor (n = 1184), nonpermissive mismatched/younger donor (n = 2659), and nonpermissive mismatched/older donor (n = 978). The median patient age at the time of HCT varied from 53 to 57 years. Most patients had acute myeloid leukemia (55%-58%) and early-intermediate risk disease (65%-67%). The use of myeloablative conditioning varied from 58% (DP-matched/younger donor) to 66% (DP-matched/older donor). Approximately 80% of patients in all groups received peripheral blood grafts. Most patients (85%-88%) received tacrolimus-based GVHD prophylaxis without in vivo T-cell depletion (62%-65%). Most patients had Karnofsky performance scale scores of ≥90 (58%-62%) and HCT-specific comorbidity index scores of ≥2 (58%-64%). The median follow-up among survivors ranged from ∼40 to 62 months (Table 1). Univariate analyses of outcomes are shown in supplemental Table 2.
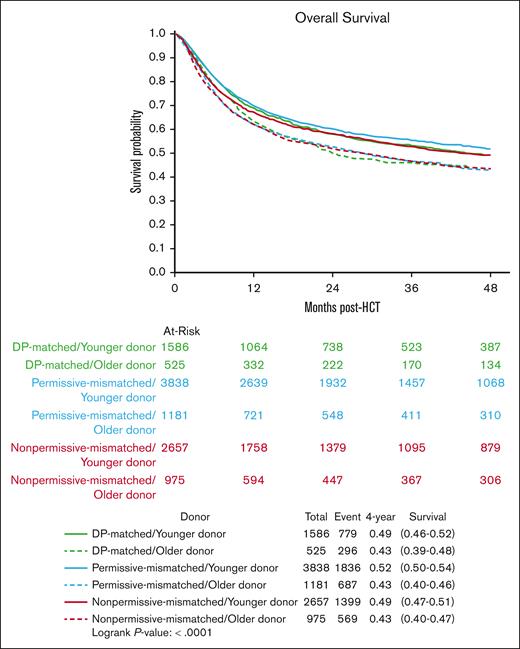
OS
The 4-year estimates of OS with younger donors were 49%, 52%, and 49% in the DP-matched, permissive-mismatched, and nonpermissive-mismatched groups, respectively, whereas with older donors it was ∼43% in all 3 HLA-DPB1–matching groups (Figure 1). In multivariate analysis, when compared with the DP-matched/younger donor (reference), the OS did not differ significantly in other groups of younger donors irrespective of DP matching. In contrast, all older donor groups had significantly inferior OS (Table 2; supplemental Table 3). In the direct pairwise comparisons, the “better-matched” older donors had ∼14% to 21% increased hazards of overall mortality than “lesser-matched” younger donors. Older donors had significantly inferior OS within each DP-match category. Among those with older donors, DP matching did not have a significant impact on OS. However, among those with younger donors, the nonpermissive-mismatched group appeared to have slightly worse OS (HR, 1.09; 95% CI, 1.02-1.17; P = .02) than the permissive mismatched group (reference), albeit with a borderline statistical significance (Table 3).
Kaplan Meier estimates of overall survival in DP-matched/younger donor (green), DP-matched/older donor (dashed green), permissive-mismatched/younger donor (blue), permissive-mismatched/older donor (dashed blue), non-permissive mismatched/younger donor (red), and non-permissive mismatched/older donor (dashed red).
Kaplan Meier estimates of overall survival in DP-matched/younger donor (green), DP-matched/older donor (dashed green), permissive-mismatched/younger donor (blue), permissive-mismatched/older donor (dashed blue), non-permissive mismatched/younger donor (red), and non-permissive mismatched/older donor (dashed red).
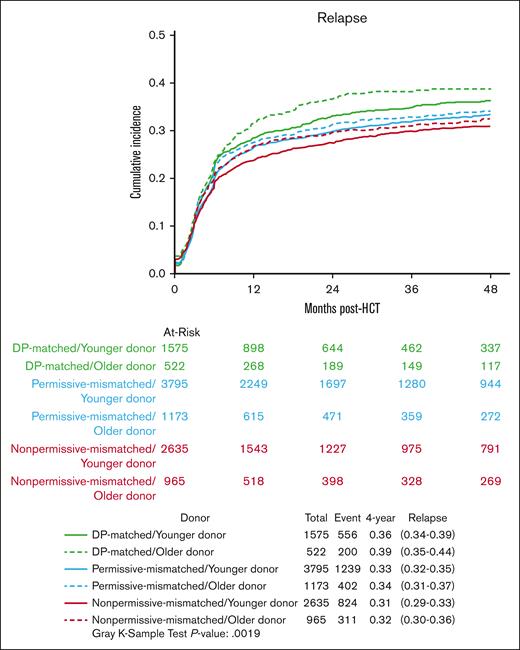
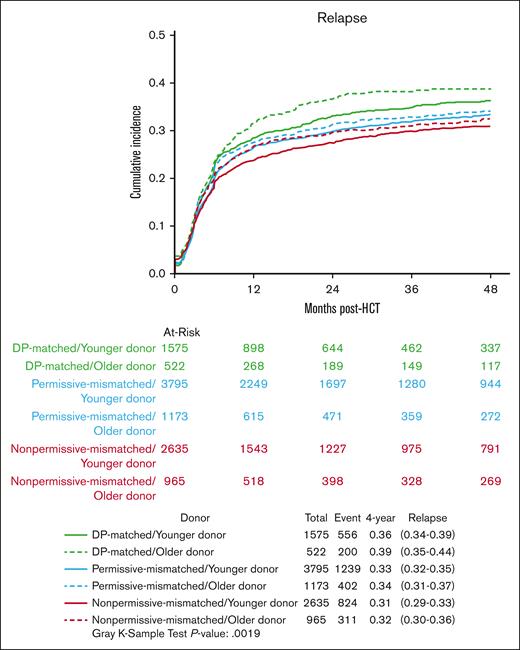
Relapse
Compared with the DP-matched/younger donor group (reference), both the permissive- and nonpermissive-mismatched groups with younger donors had a significantly lower hazard of relapse. However, this difference was not statistically significant in the permissive- and nonpermissive-mismatched groups with older donors (Table 2; Figure 2). Direct pairwise comparisons revealed 16% to 26% lower hazards of relapse in the lesser-matched younger donor groups than in better-matched older donor groups (Table 3). There was no significant impact of donor age on the risk of relapse within the individual DP-match categories. Moreover, DP-matching did not significantly influence outcomes in recipients with older donors. Conversely, recipients of grafts from younger donors demonstrated a reduction in relapse risk in both mismatched groups (permissive and nonpermissive) compared with DP-matched recipients. This effect reached statistical significance in the nonpermissive group, with borderline significance in the permissive group.
Cumulative incidence curves for relapse in DP-matched/younger donor (green), DP-matched/older donor (dashed green), permissive-mismatched/younger donor (blue), permissive-mismatched/older donor (dashed blue), non-permissive mismatched/younger donor (red), and non-permissive mismatched/older donor (dashed red).
Cumulative incidence curves for relapse in DP-matched/younger donor (green), DP-matched/older donor (dashed green), permissive-mismatched/younger donor (blue), permissive-mismatched/older donor (dashed blue), non-permissive mismatched/younger donor (red), and non-permissive mismatched/older donor (dashed red).
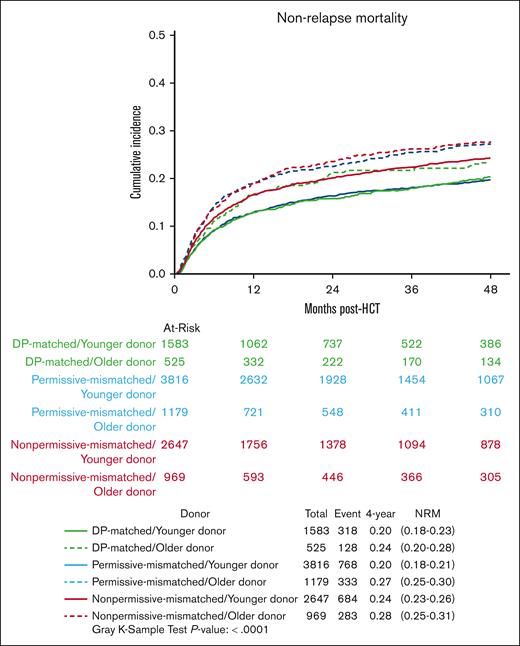
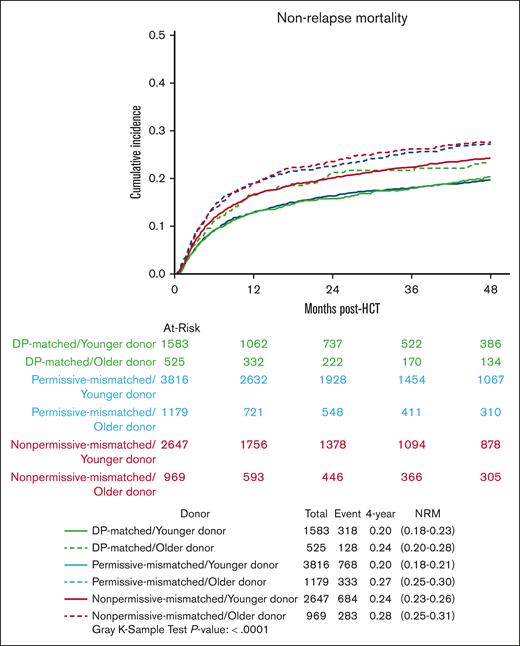
NRM
As compared with the DP-matched/younger donor group (reference), NRM did not differ significantly in the permissive-mismatched/younger donor group (HR, 0.95; 95% CI, 0.84-1.08; P = .45). All other groups had a significantly higher risk of NRM (Table 2; Figure 3).
Cumulative incidence curves for non-relapse mortality, in DP-matched/younger donor (green), DP-matched/older donor (dashed green), permissive-mismatched/younger donor (blue), permissive-mismatched/older donor (dashed blue), non-permissive mismatched/younger donor (red), and non-permissive mismatched/older donor (dashed red).
Cumulative incidence curves for non-relapse mortality, in DP-matched/younger donor (green), DP-matched/older donor (dashed green), permissive-mismatched/younger donor (blue), permissive-mismatched/older donor (dashed blue), non-permissive mismatched/younger donor (red), and non-permissive mismatched/older donor (dashed red).
In the direct pairwise comparisons, lesser-matched younger donors were not associated with an increased risk of NRM compared with better-matched older donors (Table 3). Conversely, the permissive mismatched/younger donor group had a lower risk of NRM than the DP-matched/older donor group (HR, 0.77; 95% CI, 0.64-0.93; P = .006) with borderline statistical significance. Among those with younger donors, the nonpermissive-mismatched group had a higher risk of NRM compared with the permissive-mismatched group, whereas no difference was noted between the permissive mismatched and matched groups. Among those with older donors, no significant differences were noted between the DP-match groups.
GVHD
Donor age did not influence the risk of acute GVHD in the DP-matched group. However, compared with the DP-matched/younger donor (reference), all mismatched groups had a significantly increased risk of grade 2 to 4 acute GVHD. Moreover, all mismatched groups, except the permissive-mismatched/younger donor group, had a higher risk of grade 3/4 acute GVHD (Table 2). Regarding chronic GVHD, the permissive-mismatched/younger donor group had a similar risk as the DP-matched/younger donor (reference group). However, all other groups, including the DP-matched/older donor group had a significantly higher risk of chronic GVHD.
Analysis of patients with missing DP data
To assess whether excluding patients with missing DP data (n = 3364) from the analyses may have inadvertently introduced selection bias, we compared the excluded patients with the study population (supplemental Table 4). The association of donor age with OS was similar in the excluded patients vs the study population. In multivariate analysis, there was no significant difference in OS between the excluded patients/younger donor (HR, 1.05; 95% CI, 0.98-1.12; P = .18) vs the study population/younger donor group, and between the excluded patients/older donor (HR, 0.96; 95% CI, 0.85-1.09; P = 1.00) vs the study population/older donor group (data not shown).
Discussion
We observed a marked improvement in OS with permissive mismatched/younger donors compared with DP-matched/older donors. This survival advantage was related to a lower risk of relapse and a trend toward lower NRM. Also, although previous studies suggested avoiding nonpermissive-mismatched donors in general,1,2 we noted that nonpermissive-mismatched/younger donors led to significantly improved OS compared with permissive-mismatched/older donors. Furthermore, nonpermissive mismatched/younger donors had a significantly lower risk of relapse with no significant difference in NRM compared with DP-matched/older donor. Overall, our data suggest that priority should be given to donor age over HLA-DP matching for donor selection among 10/10-HLA MUDs.
If all donor options include “younger” donors, the nonpermissive mismatched donor would be the least preferred choice because of a significantly higher risk of severe acute GVHD and NRM than other groups. When choosing between a permissive-mismatched donor and a DP-matched donor, either option is acceptable because they both result in similar OS. However, the former might be preferred because of a lower risk of relapse and no increased risk of severe acute GVHD, chronic GVHD, or NRM.
If all donors being considered are “older,” the findings of donor selection based on DP-matching should be interpreted with caution because of the relatively smaller sample size than the “younger” donor group. Nevertheless, DP-matching did not appear to have any significant impact on OS, relapse, NRM, or chronic GVHD. However, both permissive and nonpermissive mismatches were associated with a significantly higher risk of grade 2 to 4 acute GVHD; nonpermissive mismatches had a somewhat higher risk than permissive mismatches. Whether a younger mismatched unrelated donor16 may be considered in such cases requires further investigation.
Collectively, these findings suggest that DP matching may be more important for selection decisions within the context of younger donors, who constituted the majority. Nonpermissive mismatches are characterized by the DPB1-specific alloreactivity in the GVH and/or HVG direction, whereas permissive mismatches are generally not associated with a vector of mismatch.1,17,18 We grouped patients with GVH or HVG nonpermissive mismatches together because their OS was not significantly different (data not shown) and previous studies indicated no significant differences in outcomes based on the directionality.15 Whether the inclusion of donor age with the mismatch vector could influence outcomes was not assessed in our analysis. A recent study revealed that the extent of immunopeptidome divergence between the donor and recipient plays a crucial role in determining permissiveness, shedding more light on the mechanism behind permissiveness.19 Moreover, the TCE model was refined, further segregating permissive mismatches into “core” and “noncore” groups.20 The interaction between donor age and DP matching using this classification system remains unclear.
Our study has the limitations of a retrospective registry analysis. We lacked data on the molecular classification of diseases, measurable residual disease status, and ABO matching. Also, because of a lack of data about systemic therapy-requiring chronic GVHD, we were unable to compute GVHD-free relapse-free survival. Lastly, our findings apply to only CNI-based GVHD prophylaxis. Although the use of PTCy is increasing (31%), CNI-based prophylaxis remains the most commonly used GVHD prophylaxis regimen among MUD recipients in the United States (66%).21 Whether similar findings would be seen with PTCy-based or other novel GVHD prophylaxis regimens remains unknown, and needs further investigation. With numerous HLA and non-HLA factors that predict outcomes, donor selection remains a complex clinical challenge. How to best integrate donor age and DP matching with other variables, such as donor/recipient sex mismatch, cytomegalovirus serostatus,22 and ABO compatibility,23 remains unclear. Our study adds to the literature by presenting further granularity of the interaction between DP matching and donor age on outcomes of 10/10 HLA MUD HCT and may help guide unrelated-donor selection.
Conclusion
The distinction between DP-matched, permissive-mismatched, and nonpermissive-matched cases should take donor age into consideration. A “younger” donor should be prioritized over DP matching. Future studies with independent data sets and with novel GVHD prophylaxis regimens are needed.
Acknowledgments
The authors are grateful to the Center for International Blood and Marrow Transplant Research staff for providing the data sets publicly. The authors acknowledge that European Union patient-level data are redacted.
This data set was collected by the Center for International Blood and Marrow Transplant Research, which is supported primarily by the Public Health Service U24CA076518 from the National Cancer Institute; the National Heart, Lung, and Blood Institute; the National Institute of Allergy and Infectious Diseases; 75R60222C00011 from the Health Resources and Services Administration; N00014-23-1-2057 and N00014-24-1-2057 from the Office of Naval Research; the National Marrow Donor Program; and the Medical College of Wisconsin. E.W.P. is supported by grants AI069197, CA218285, CA100019, and CA231838 from the National Institutes of Health.
Authorship
Contribution: R.S.M. conceptualized the study, performed the statistical analysis, interpreted data, wrote the manuscript, had full access to the raw data, which is publicly available, and had the final responsibility to submit for publication; E.W.P., T.W., S.R.S., and S.J.L. reviewed and interpreted the data, reviewed the manuscript, and provided critical feedback; and all authors approved the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Rohtesh S. Mehta, Clinical Research Division, Fred Hutchinson Cancer Center, 1100 Fairview Ave N, Seattle, WA 98109; email: rmehta@fredhutch.org.
References
Author notes
The data are publicly available and accessible at https://cibmtr.org/CIBMTR/Resources/Publicly-Available-Datasets.
The full-text version of this article contains a data supplement.