Key Points
Both patients with sickle cell disease and ED providers strongly endorse IPPs.
Collaboration among specialties, including informatics and patients, is needed to successfully implement IPPs.
Visual Abstract
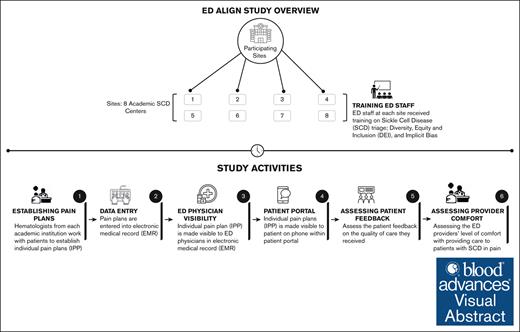
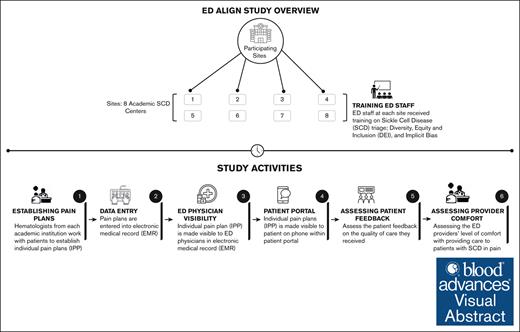
To address acute vaso-occlusive episodes (VOEs), the leading cause of emergency department (ED) visits among individuals with sickle cell disease (SCD), we conducted the clinical study, ALIGN (An Individualized Pain Plan with Patient and Provider Access for Emergency Department care of SCD), across 8 sites. We hypothesized an improvement of 0.5 standard deviations in perceived quality of ED pain treatment of a VOE after implementing individualized pain plans (IPPs) accessible to both patients and providers. Patients with SCD were aged 18 to 45 years, owned a cell phone, and had an ED VOE visit within 90 days prior. Patients completed the perceived quality of care surveys at baseline and within 96 hours after an ED VOE visit. Providers completed surveys regarding comfort managing VOEs at baseline and after managing an enrolled patient. Most of the 153 patients were African American (95.4%), female (64.7%), and had Hb SS/Sβ0 genotype (71.9%). The perceived quality of ED pain treatment was high at both baseline and after implementation of IPPs; our primary outcome hypothesis was not met, because no statistically significant change in the patient-perceived quality of ED treatment occurred. A total of 135 providers completed baseline and follow-up surveys. On a scale of 1 to 7, with 7 being extremely comfortable managing VOEs, 60.5% reported a score ≥6 after IPP implementation vs 57.8% at baseline. Almost all (97.6%) ordered the recommended medication, and 94.7% intended to use IPPs. In this implementation protocol, all sites successfully implemented IPPs. Patients and ED providers both endorsed the use of IPPs. This trial was registered at www.ClinicalTrials.gov as # NCT04584528.
Introduction
Sickle cell disease (SCD) is a common genetic hemoglobinopathy associated with several acute and chronic complications that affect multiple organ systems, leading to frequent hospitalizations, poor quality of life, and reduced life expectancy.1-3 The leading cause of emergency department (ED) visits for individuals with SCD is acute vaso-occlusive episodes (VOEs).4 VOEs occur suddenly and cause acute pain often requiring parenteral opioids, sometimes in high doses.5 Individuals with SCD report difficulty in obtaining opioid medication leading to dissatisfaction with ED care.2 Emergency health care providers are reluctant to treat VOEs with high doses of opioids due to the opioid epidemic and state or hospital policies restricting opioid administration.2 Individuals with SCD are often stigmatized as drug seeking, resulting in undertreatment of pain.2
In 2014, the National Heart, Lung, and Blood Institute published evidence-based recommendations to guide ED treatment of VOEs.6 One important recommendation is the implementation of individualized pain plans (IPPs), which can be written to include patient-specific drug and dose recommendations.6 Individuals treated with an IPP experienced greater reduction in pain than those treated with a weight-based opioid protocol.7 In 2020, the American Society of Hematology recommended using multidisciplinary teams to develop IPPs to treat VOEs and proposed embedding the IPPs in electronic medical records (EMRs).8
To foster implementation of these guidelines, the National Heart, Lung, and Blood Institute funded 8 centers across the United States to participate in the Sickle Cell Disease Implementation Consortium (SCDIC).9 We now report the results of 1 of the projects: ALIGN (An Individualized Pain Plan with Patient and Provider Access for Emergency Department care of Sickle Cell Disease).10 In ALIGN, the hematologist/SCD specialist at each center developed IPPs for the treatment of VOEs in the ED setting. IPPs were made available to ED providers via the EMR and to patients via their institution’s patient portal, which was accessible through a phone application. This was the first time that patients had access to IPPs through their EMR.
ALIGN aimed to detect changes in the following outcomes before and after the implementation of IPPs for enrolled participants: (1) patient-perceived quality (PPQ) of ED pain treatment of a VOEs; and (2) ED provider–perceived quality of ED pain treatment and comfort in treating VOEs. We hypothesized that among enrolled patients with at least 1 ED VOE visit during the intervention period, the perceived quality of ED pain treatment would increase by 0.5 standard deviation (SD) after an ED VOE visit compared with the last ED VOE visit made by these patients within 90 days before enrollment. We also assessed patient and provider willingness to use and prior experience using IPPs in the EMR and patient portal.
Methods
Design
The methods were previously published and are summarized here.10 An implementation science approach using a prepost design was used. Each site and the data coordinating center obtained approval from their institutional review board. Before obtaining data, patients provided written, electronic, or verbal consent, per the local institutional review board. ED provider consent was implied after being approached by research staff or study investigators and completing the baseline survey.
Conceptual framework
This study was guided by the Consolidated Framework for Implementation Research11 and RE-AIM frameworks (Reach, Effectiveness, Adoption, Implementation, and Maintenance).12 Consolidated Framework for Implementation Research provides a comprehensive, evidence-based, and standardized approach to understanding implementation determinants for intervention planning. The 5 dimensions of RE-AIM were used for evaluation appropriate for the patient, provider, or organizational and system levels. Examples of RE-AIM are noted in parentheses below.
Setting
The participating centers were part of the SCDIC. The sites included centers from the Northeast, Midwest, South, and West Coast. All centers were supported by a strong outpatient SCD team of multidisciplinary providers (Adoption). All ED sites were academic emergency medicine centers. Seven of the 8 centers were considered urban; 1 site was a designated children’s ED. Each site engaged hematologists or sickle cell providers, emergency physicians, and advanced practice providers, as well as key stakeholders from the hospital informatics department. Six of the 8 sites had already developed IPPs for most of their patients with SCD; these plans were accessible in the EMR for emergency providers. Before this study, there was variability in how the IPPs were constructed and housed in the EMR; no site had IPPs visible to the patient via the EMR patient portal.
Patient sample criteria
The following inclusion criteria applied: ages 18 to 45 years; the genotypes as verified in the EMR, including SS, Sβ0, SC, Sβ+, and other disease variants; access to a cell phone or Internet; and had an ED VOE visit to the outpatient center within the previous year, before IPP implementation in the EMR.
Patient recruitment and data collection
The study staff screened the EMR to identify patients who met the eligibility requirements. Patients were recruited in person in the clinic, via phone, or by messaging via their EMR. Patients completed a baseline survey including demographic and clinical characteristics, as well as their perception of the quality of care they received at the last ED VOE visit at the study site, within the past 90 days (reach). If patients had an ED visit after enrollment, they received a text message within 2 weeks with the same 3 questions to assess the perceived quality of care of that ED VOE visit. Patients responded to the text messaging application. If patients had >1 ED visit per month, they were sent a follow-up survey only after the first qualifying visit of that month. Patients could complete >1 survey over the study period if they had >1 visit over the span of >1 month. Only the first follow-up survey was included in the primary analysis.
Provider sample criteria
ED physicians, nurse practitioners, and physician assistants with access to the EMR in the ED at each study site were eligible for inclusion.
Provider recruitment and data collection
ED providers were recruited primarily during faculty meetings (reach). They were asked to complete a brief baseline survey via email regarding ED provider–perceived quality of ED pain treatment, provider self-efficacy in treating VOEs and their likelihood of using IPPs in the future. The survey included a waiver for written consent. Upon survey completion, they were asked to view a 2-minute video addressing stigma and the actual prevalence of opioid addiction in SCD, as well as an introduction to the EMR-embedded IPP and video demonstration of how to access it via the EMR. The research staff tracked subsequent ED visits for consented patient visits. After a qualifying patient ED visit (the patient was enrolled in the study, the ED visit was for VOE, and it was their first ED VOE visit of the month), research staff emailed providers a link to the follow-up survey for completion. Survey questions were identical to the baseline questions. The providers were sent the survey between 96 hours and 2 weeks of the ED visit. Only provider surveys that collected data on the patient's first ED visit of the month were included in the primary analysis. All responses were analyzed as a supplemental analysis.
Interventions
Design and accessibility of IPPs
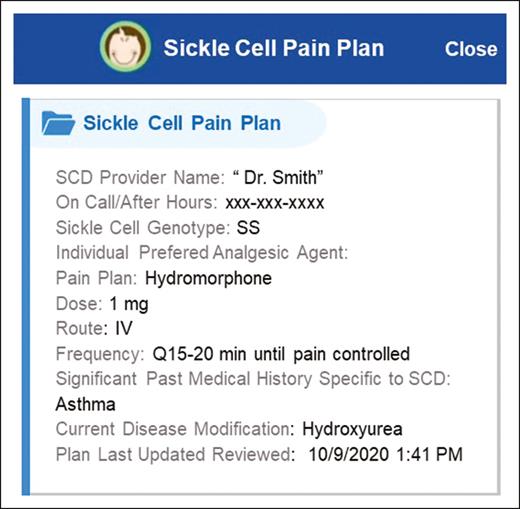
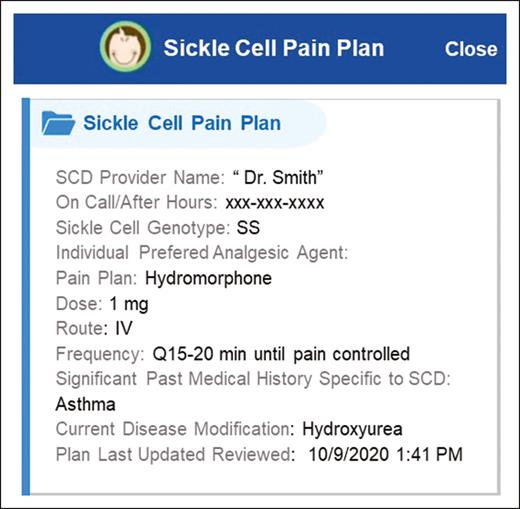
The study team developed a template that included the following information as a part of the IPP: analgesic drug, dose, route, genotype, SCD provider name and contact information, drug or food allergies, and significant past medical history specific to SCD or relevant to an ED visit (site-specific example; Figure 1). The IPP content was the same in both the provider- and patient-facing formats. The SCD provider was notified when 1 of their patients consented to participation and was asked them to write an IPP. The SCD provider met with the patient and asked what medication and dosage works best to treat their pain during previous ED visits for VOEs. To inform this discussion, the SCD provider reviewed previous doses administered in the ED and asked whether these doses were helpful. The study staff worked closely with the hospital informatics team to ensure that the plans were visible to the patient and the ED providers. Many sites transferred the plan into a letter format that was made visible in the “Communications” tab in their EMR patient portal (Implementation).
Each study team created a site-specific, short video for patients with instructions on how to access their IPP and reviewed this in person with the patient. The patient was notified of the IPP and instructed by the study staff on how to access the plan via their EMR patient portal. If a patient was not enrolled in their portal, research staff assisted with this. The study team used a teach back method that required the patients to demonstrate how to access their IPP in the patient portal. All patients were provided with a wallet card including instructions on how to access their IPP within their patient portal. The card did not include their actual analgesic dose.
Sites used the following additional optional strategies for patients and providers to remind them of the IPPs and how to access them (number of sites at which the strategy was offered): patient scripting on how to communicate with the ED providers about how to find their IPP (n = 6); EMR-embedded prompts to remind ED providers of the IPP (n = 5); EMR-embedded prompts to remind the ED providers of how to find their IPP (6), EMR-embedded prompts to remind ED providers of the IPP (5), EMR-embedded prompts to remind the nurses of the IPP (3), provider booster education sessions (2), and provider education via blogs, journal clubs, and/or staff meetings (6).
Measures (survey questions)
Patients
The study used the ASCQ-Me (Adult Sickle Cell Quality of Life Measurement Information System) Quality of Care measure to evaluate the primary study outcome, PPQ of ED pain treatment.13 The following 3 questions were used for patients at baseline and for ED visits after IPP implementation. Responses used a 5-point Likert scale (not at all, a little bit, somewhat, quite a bit, and very much) (Effectiveness):
Were you satisfied with the care you received?
How much were the emergency room doctors and nurses able to help your pain?
How much did the emergency room doctors and nurses believe that you had very bad sickle cell pain?
These 3 questions were combined and analyzed as a composite score and reported as perceived quality of ED pain treatment, the primary outcome.
At enrollment, patients were asked to rate their familiarity with using EMR to access their medical record on a scale of 1 to 7 (1 = does not know at all; 7 = extremely well).
After qualifying the ED visits, patients were asked the following questions using a 1 to 7 rating scale with 7 rating the highest:
How easy was it to find your pain plan in the portal?
How helpful was the pain plan in helping you get the pain treatment you need?
If you were to go to the ED again, how likely are you to show the doctors your pain plan? (Maintenance)
Patients were also asked the following yes/no questions when completing follow-up surveys:
Did the doctor pull their pain plan from the computer?
Did they remind the doctor that they had a pain plan in the system?
Did they show the doctor their pain plan on their phone?
ED providers
Providers completed a brief questionnaire at baseline, including demographics, and were asked to respond to the following 3 items on a 1 to 7 Likert scale, with 7 meaning best (Effectiveness):
I do a good job managing pain for patients with SCD
How comfortable are you with your ability to manage acute pain episodes experienced by patients with SCD?
How likely are you to use the individualized pain plan when a patient with SCD has an ED visit?
Providers were asked the following additional questions when completing follow-up surveys:
Did you find or see the pain plan for the patient? (multiple response options)
On a scale of 1 to 7, how easy was it to find the IPP?
Did you order the opioids suggested in the pain plan? (Yes/no)
Did you order the dose suggested in the IPP? (Yes/no)
On a scale of 1 to 7, how helpful was the IPP in providing care to the patient?
Assuming I have access to the system, I intend to use the IPP (all, most, half, or some of the time). (Maintenance)
Statistical analysis
Patients
Categorical variables including patient demographics and other characteristics and responses to questions related to PPQ of ED care and the pain plan were summarized as frequencies and percentages. The primary outcome analysis was conducted for unique patients who completed a baseline and 1 follow-up survey. The primary outcome of the study was PPQ of ED pain treatment, measured by the following 3 questions from the baseline and the first follow-up surveys:
Were you satisfied with the care you received?
How much were the emergency doctors and nurses able to help your pain?
How much did the emergency doctors and nurses believe that you had very bad sickle cell pain?
Responses to each of these 3 questions were scored 0 to 4 for “not at all” to “very much,” and the 3 responses were averaged to create a composite score of the overall PPQ of ED pain treatment. Change in PPQ of ED care in response to intervention (IPP implementation) was calculated for each subject by subtracting baseline PPQ score from PPQ score at the first postintervention survey. Our hypothesis was that there would be an increase of 0.5 SD in perceived the quality of ED pain treatment from baseline to an ED visit after implementation of IPPs in the EMR for both the ED provider and patient portal.
A 2-sided 1-sample t test was used to evaluate the overall mean change in PPQ. Predictors of change in PPQ, including sex, age group, site, prior IPP implementation, and SCD genotype, were evaluated using general linear models. A separate model was generated first with 1 predictor at a time, and then all predictors were entered into multivariable models. Because prior IPP was determined by site, we ran 2 separate multivariable models including each individual variable at a time. All models were adjusted for baseline patient satisfaction to account for the negative correlation expected between baseline score and change in score.
On follow-up surveys, patients were also asked questions about the use of their IPP in their patient portal during the ED visit.
Additional analysis was also conducted for all patient survey responses at baseline, including patients who did not have an ED visit, and for all ED visits, which included patients with multiple ED presentations (supplemental Table 1).
Providers
The provider analysis was conducted for unique providers who completed a baseline and at least 1 follow-up survey. Provider demographics and other characteristics, as well as responses to questions related to managing pain, comfort level when caring for patients with SCD, and the pain plan, were summarized as frequencies and percentages. If a provider completed >1 follow-up survey, only responses to the first follow-up survey were analyzed. Follow-up survey questions for providers included questions about the likelihood of using the IPP.
Additional analysis was also conducted for all provider survey responses at baseline, including providers who did not have a follow-up visit, and for all follow-up visits inclusive of providers who completed multiple follow-up surveys (supplemental Table 3).
Results
Participant demographics
One hundred fifty-three patients completed the baseline survey, returned for an ED visit, and completed a follow-up survey on PPQ of care after the ED visit. Demographics are reported in Table 1, with most being African American, female, and of genotype SS/Sβ0. One hundred thirty-five providers completed the baseline survey and at least 1 follow-up survey after managing a study patient in the ED. (Table 1). Most of the providers were attending physicians (78.5%), and resident physicians (14.8%).
Patient perceptions
A total of 276 unique patients signed a consent and completed a baseline survey. A total of 159 patients also completed a follow-up survey, but only 153 responded to the questions on PPQ of ED pain treatment. A total of 68 patients completed >1 follow-up survey over the course of the study for a total of 329 follow-up surveys. When limited to the 153 patients who responded to questions on quality of ED pain treatment, the total number of follow-up surveys was 318, with 63 patients completing >1 follow-up survey.
Table 2 reports baseline and follow-up quality of ED pain care for the 153 patients with both a baseline and a follow-up survey. More than half (57.6%) were quite a bit or very much satisfied with the care they received at baseline vs 62.7% after intervention. Similarly high levels of satisfaction were reported when asked about how ED physicians and nurses treated their pain (Table 2). The mean primary outcome, the composite measure of quality of ED pain treatment scores, were 2.66 (SD, 1.12) and 2.83 (SD, 1.07) at baseline and follow-up, respectively. Although not statistically significant, we found a mean change of 0.17 (SD, 1.41) in the perceived quality of ED pain treatment score after an ED VOE visit, after intervention, compared with the last ED VOE visits made by these patients within 90 days before enrollment. Our hypothesis was that we would find a 0.5 SD improvement, thus we did not achieve our target improvement. These findings were similar when assessing responses after subsequent ED visits (supplemental Table 1). We did not find a difference in perceived quality of care between sites that had previously implemented IPPs in the EMR compared with sites that had not (P = .87). When exploring potential predictors of change in PPQ, none of the covariates evaluated in the models showed a statistically significant relationship with change in PPQ, with exception to baseline PPQ (results are included as supplemental Table 2).
Table 3 displays patients' responses regarding ease of use and communication frequency with ED providers, as well as whether they had a plan in the EMR during the first and all following ED visits. Overall, patients reported high scores in ease of use of the plan. Table 3 indicates that most patients reminded the provider they had an IPP and reported a high likelihood they would show their IPP to an ED provider in future visits.
Provider perceptions
Table 4 includes 135 providers who completed both a baseline and a follow-up survey. Providers reported high ratings for all questions at baseline and follow-up with no change between baseline and after implementation. In total, 405 providers returned surveys at baseline and 207 surveys were returned from these providers after qualifying ED visits. Results were similar and are reported in supplemental Table 3.
More than half (62%) of the providers indicated they were able to see the pain plan in the EMR provider interface, and 52.4% found the IPPs extremely easy to use. Almost all (97.6%) reported ordering the medication suggested in the IPP, 92% reported ordering the suggested dose, and 95% reported an intention to use the IPP in the future.
Discussion
Despite national guidelines recommending the use of IPPs for years, adoption in the United States remains low.6,8 In a prospective, multicenter implementation study, we report the results from a multilevel strategy implementation study that targeted both patients and providers.
For the first time, to our knowledge, we measured change in patient satisfaction of ED pain management, before and after patients had access to their own pain plan in their patient portal. Previous research and quality improvement efforts have noted improvements with the use of IPPs in time to administration of first analgesic14-16 and ED length of stay.16,17 In a randomized controlled trial (RCT) comparing IPPs vs a weight-based dose, patients receiving an IPP achieved greater reductions in pain scores in the ED.7 Although these are all important outcomes, specific patient feedback is critically important, and there remains room for improvement.18 Although no statistically significant change in patient reported quality of ED pain treatment after IPP implementation was noted, this may be due to high patient reported baseline quality scores. Similar percentages of patients reporting satisfaction with ED care were found in earlier registry data from the SCDIC sites; 50% were satisfied with ED care in the registry cohort and 57% at baseline for ALIGN.19 These percentages are in contrast with what was found for the ASCQ-Me reference data (40%) that were collected almost a decade earlier and included patients with SCD seen in a range of community settings without SCD expertise.13
ED providers at our study sites rated their ability to manage VOE pain at baseline and after implementation of IPPs as moderately high; the high baseline score affected the ability to detect significant improvement. This is similar to prior work in which a national survey of ED physicians self-reported awareness of vaso-occlusive crisis (VOC) guidelines and adherence to opioid drug choices.20 In the same survey, ED physicians with more negative attitudes were less likely to redose opioids in 30 minutes for unrelieved pain.20 Conflicting research has found that although ED providers may be confident in their ability to provide good pain management, they are often unaware of the guidelines to do this.21
One of our most important findings was the high ease of use of IPPs by patients and ED providers. A high proportion of patients reported the protocols as relatively easy to find and use, and many showed the IPP to the ED provider. There was some discrepancy between how often the patients reported showing the plan to the ED provider and provider report of seeing the plan in the EMR. As mentioned, 6 of the 8 sites previously had IPPs in the EMR, and thus, patients most likely did not need to show the plan on their phone to the ED provider. The primary intervention of this protocol was demonstrating the ability to place IPPs in the patient portal and determine whether patients could find them. We demonstrated this was possible, and the primary benefit will be when patients visit EDs outside their home SCD facility.
ED providers reported high levels of adherence to the IPP dosing and intention to use in the future. Adherence to the drug and dose ordered has now been validated in 2 separate RCTs conducted in 8 different EDs. Adherence to the drug ordered by the hematologist ranged from 88% to 96% and dose within 0.1 to 0.4 mg of morphine sulfate equivalents.7,22 In a prior RCT, ED physicians and nurses were asked about their ability to find the IPP or weight-based protocol, clarity, and perception of ability to relieve pain compared with usual care. Both physicians and nurses felt the protocols were easy to find and physicians felt the orders were clear, whereas nurses did not. Nurses reported IPPs were more effective at relieving pain than usual care.25
We learned many lessons. A multidisciplinary team is essential to ensure success. Our teams included the patient, SCD specialist/hematologist, ED physician, nurses, and nursing leaders, as well as informatics team members from the institution who could work directly with the ED and hematology experts. An important first step was making the IPP visible to the patient, allowing patients to bring up their IPP from their EMR in any ED, thus making the plan appear more authentic from an ED provider’s perspective. In our implementation trial, some patients had never used the patient portal. Research staff were able to instruct the patient on how to download their portal application and how to find their IPP in their portal. We worked with all sites and their IT teams to identify the easiest way for the patient to find the IPP. For sites that used EPIC as their EMR, most placed the IPP in the “Communications” tab in the form of a letter. Other non-EPIC sites worked with their IT departments to create a point-and-click smart form that created a banner in the opening view of the ED patient chart. The IPP was also accessible under the “Menu” function in MyChart as a stand-alone document labeled “Sickle Cell Pain Plan.” Convenient access to their IPP was a motivator for patients to download their patient portal application.
The hematologist/SCD provider is a critical member of the team and must know the patient’s outpatient opioid used to be able to write the IPP. Importantly, the development of a pain plan for the ED should be collaborative with the patient.8 Since we conducted this implementation project, an online opioid calculator that has been developed to assist hematologists in determining a starting ED opioid dose based on chronic outpatient opioid use and past successful relief.23 ED providers are critical partners because they should be aware of the protocols and have the opportunity to discuss any concerns, particularly over high opioid doses. The informatics team members should work with the ED team to establish how to build the IPP within the EMR for easy viewing, addressing a well-known barrier to quick and easy access to IPPs.24,25
Limitations
The SCDIC included established SCD centers, which likely biased the baseline ratings. Six of the study sites already had implemented IPPs in the EMR for ED providers, thus limiting the ability to determine effectiveness of IPPs in improving patient satisfaction with ED care. Baseline patient satisfaction and provider quality of providing ED pain treatment at all sites were high. However, lessons learned can benefit future implementation of IPPs in academic and community settings. We did not report health care utilization. Similar to many implementation studies, our study was underpowered to evaluate the impact of the individual optional education strategies, and thus, we did not measure the differences. Sharing these approaches can inform future IPP implementation. We did not measure actual adherence to the IPP. However, in previous randomized controlled trials, adherence to IPPs was measured and found to be excellent.7,22 This was an implementation trial, and the primary purpose was to determine whether we could implement IPPs in the EMR for providers and in the patient portal for patients. The temporality between before and after implementation of IPPs to assess PPQ of ED pain treatment was different; 1 month (baseline) and within 96 hours of the last ED visit (after IPP implementation). Although the differences may affect scores, this decision was made to balance the ability to enroll a large enough sample and include better quality of data. The longer interval between ED visit and quality of pain care assessment threatens patient recall. We have no reason to believe the data may be more influenced in 1 direction. We did not collect data before the implementation of IPPs at the sites regarding whether the plans were routinely used. One of the sites did not have cell service in the ED; thus, patients were unable to show their IPP to the ED provider unless they joined the Wi-Fi network.
Conclusion
Implementation of IPPs did not reach the predetermined change of 0.5 SD improvement in PPQ of ED treatment from baseline to after implementation of IPPs. However, as an implementation study, we demonstrated for the first time, to our knowledge, the successful implementation of IPPs in the patient portal. All sites also implemented IPPs in the EMR for ED providers. Both patients and ED providers endorsed the use of IPPs, which can help guide management of VOE in any ED, regardless of the center.
Acknowledgments
The Sickle Cell Disease Implementation Consortium has been supported by the US Federal Government cooperative agreements (HL133948, HL133964, HL133990, HL133996, HL133994, HL133997, HL134004, HL134007, and HL134042) from the National Heart, Lung, and Blood Institute and the National Institute on Minority Health and Health Disparities of the National Institutes of Health (NIH; Bethesda, Maryland).
The content of this manuscript is solely the responsibility of the authors and does not necessarily represent the NIH.
Authorship
Contribution: A.K., P.T., L.S., C.R.C., J.S.H., J.S.C., L.P., L.L., L.C., and M.T. conceived the study and contributed to interpretation of data; L.P. conducted the analysis; A.K., L.S., P.T., and R.V.M. wrote the first draft of the manuscript; all authors critically commented on the manuscript and approved the final version; and L.S. is the guarantor of the manuscript.
Conflict-of-interest disclosure: C.R.C. is the deputy editor-in-chief of Academic Emergency Medicine, associate editor of Annals of Internal Medicine's ACP Journal Club, and associate editor of Journal of the American Geriatrics Society; and also serves on the American College of Emergency Physicians Clinical Policy Committee and the American Board of Emergency Medicine as an MyEMCert editor. M.T. is a consultant for Pfizer; and received royalties from Wolters Kluwer Health. P.T. is a consultant for CSL Behring; and received funding for salary support from the National Heart, Lung, and Blood Institute. The remaining authors declare no competing financial interests.
Cathy L. Melvin died on 13 September 2023.
A complete list of the members of the Sickle Cell Disease Implementation Consortium appears in “Appendix.”
Correspondence: Lauren Siewny, Duke University Medical Center, Box 3096, 2301 Erwin Rd, Durham, NC 27710; email: lauren.siewny@duke.edu.
Appendix
The members of the Sickle Cell Disease Implementation Consortium are Jane Hankins, Jason Hodges, Yvonne Carroll, Matthew Smeltzer, Chinonyelum Nwosu, James Gurney, Jerlym Potter, Sherif Badawy, Jeremie Estepp, Marsha Treadwell, Elliott Vichinsky, Ted Wun, Michael Potter, Danielle Hessler, Ward Hagar, Anne Marsh, Lynne Neumayr, Cathy Melvin, Julie Kanter, Shannon Phillips, Robert Adams, Martina Mueller, Caroline Davila, Sarah Bourne, Nirmish Shah, Paula Tanabe, Hayden Bosworth, George Jackson, Rachel Richesson, Janet Prvu-Bettger, Rita Masese, Terri DeMartino, Abdullah Kutlar, Robert Gibson, Angela Snyder, Maria Fernandez, Matthew Lyon, Richard Lottenberg, Raymona Lawrence, Sierra Gollan, Latanya Bowman, Lynne Richardson, Jeffrey Glassberg, Jena Simon, George T. Loo, Cindy Clesca, Elizabeth Linton, Gery Ryan, Victor Gordeuk, Jana Hirschtick, Lewis Hsu, Jerry Krishnan, Abe Wandersman, Joe Colla, Kim Erwin, Andrea Lamont, Sarah Norell, Kay Saving, Judith Nocek, Allison King, Ana Baumann, CeCe Calhoun, Lingzi Luo, Aimee James, Regina Abel, Taniya Varughese, Barbara Kroner, Lucia Rojas-Smith, Tabitha Hendershot, Lisa DiMartino, Sara Jacobs, Whitney Battestilli, Don Brambilla, Lisa Cox, Liliana Preiss, Norma Pugh, Joseph Telfair, Kathryn Hassell, Alexis Thompson, William Tompkins, Sharon Smith, Harvey Luksenberg, Marlene Peters-Lawrence, Cheryl Boyce, Whitney Barfield, and Ellen Werner.
References
Author notes
Data are available on request from the corresponding author, Lauren Siewny (lauren.siewny@duke.edu).
The full-text version of this article contains a data supplement.