Key Points
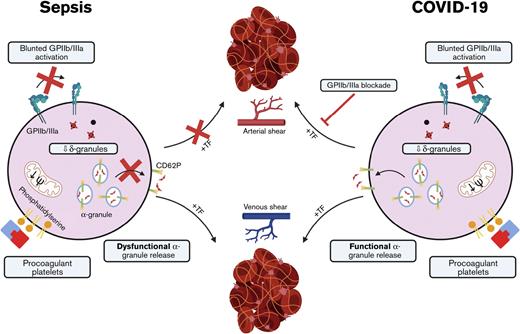
Blunted GPIIb/IIIa activation is uncoupled from functional α-granule release in patients with COVID-19, differing from bacterial sepsis.
Subthreshold doses of GPIIb/IIIa blockers prevent thrombus formation in COVID-19.
Abstract
Thromboembolic events are frequent and life-threating complications of COVID-19 but are also observed in patients with sepsis. Disseminated thrombosis can occur despite anticoagulation, suggesting that platelets play a direct but incompletely understood role. Several studies demonstrated altered platelet function in COVID-19 with some controversial findings, while underlying disease-specific mechanisms remain ill defined. We performed a comprehensive cohort study with 111 patients, comprising 37 with COVID-19, 46 with sepsis, and 28 with infection, compared with control participants. Platelet phenotype and function were assessed under static and flow conditions, revealing unexpected disease-specific differences. From hospital admission onward, platelets in COVID-19 failed to activate the integrin glycoprotein IIb/IIa (GPIIb/IIIa) in response to multiple agonists. Dense granule release was markedly impaired due to virtually missing granules, also demonstrated by whole-mount electron microscopy. By contrast, α-granule marker CD62P exposure was only mildly affected, revealing a subpopulation of PAC-1−/CD62P+ platelets, independently confirmed by automated clustering. This uncoupling of α-granule release was not observed in patients with sepsis, despite a similar disease severity. We found overall unaltered thrombus formation in COVID-19 and sepsis samples under venous shear rates, which was dependent on the presence of tissue factor. Unexpectedly, under arterial shear rates, thrombus formation was virtually abrogated in sepsis, whereas we detected overall normal-sized and stable thrombi in blood from patients with COVID-19. These thrombi were susceptible to subthreshold levels of GPIIb/IIIa blockers, eptifibatide, or tirofiban that had only a minor effect in control participants’ blood. We provide evidence that low-dose GPIIb/IIIa blockade could be a therapeutic approach in COVID-19.
Introduction
Severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) is a recently evolved Betacoronavirus and the trigger of the COVID-19 pandemic with >500 million confirmed infections and 6.2 million deaths worldwide as of April 2022.1,2 A subset of infected patients develops life-threatening pneumonia and acute respiratory distress syndrome and, despite frequently being on strict anticoagulation,3,4 also disseminated thrombosis, which was confirmed through postmortem studies. Platelets have thus been identified as a major contributor to disease burden, but their exact role in COVID-19–based thrombotic and thromboembolic events remains a matter of debate.5-7 The interaction between platelets and the immune system was shown to trigger thrombosis by antibody-mediated mechanisms or neutrophil extracellular trap formation in patients with COVID-19.8-10 This specific interplay, referred to as immunothrombosis, constitutes a hallmark of sepsis, a systemic inflammatory disease, which becomes aggravated by disseminated thrombotic events and can exacerbate to disseminated intravascular coagulation (DIC).11,12 Prevention and therapy of thrombosis are thus indispensable for patients with COVID-19 or sepsis. As most studies focused on anticoagulation, clinical data on the use of antiplatelet medication in both disorders are limited.13,14 Recent data from the REMAP-CAP trial suggest that critically ill patients with COVID-19, especially, might benefit from antiplatelet therapy.15 Furthermore, disease-specific differences regarding platelet dysfunction in COVID-19 and sepsis remain ill defined. Previous studies provided controversial and in part even contradictory results, describing that platelets are (or become) hyperreactive or hyporeactive, respectively.9,16-18
In this comprehensive platelet function study, we provide results from 111 patients, including 37 patients with confirmed diagnoses of COVID-19, 46 with sepsis, and 28 with infection at disease onset (t1). For patients who were critically ill, a 1-week follow-up (t2) was performed. We found, by flow cytometry, that patients with sepsis, compared with patients with COVID-19, showed a markedly reduced α-granule release upon stimulation. By contrast, glycoprotein IIb/IIIa (GPIIb/IIIa) activation and δ-granule secretion were profoundly deficient in patients who were critically ill with either COVID-19 or sepsis. In a microfluidic flow chamber model, thrombus formation was severely impaired only in patients with sepsis, whereas patients with COVID-19 showed numerous and overall stable thrombi. Our comprehensive data strongly imply that there is a SARS-CoV-2–specific dysfunctional platelet phenotype, which could be exploited as a therapeutic target. Subthreshold doses of tirofiban or eptifibatide, which had a minor effect in blood of healthy donors, prevented thrombus formation in blood derived from patients with COVID-19.
Material and methods
Study cohort and sample generation
Patients were recruited at the University Hospital Würzburg (UKW), Würzburg, Germany (supplemental Figure 1). The study was approved by the local ethics committee (92/19 and 63/20); additional ethics approval was obtained in the context of a broad consent for the COVID-19 cohort, and the study was conducted according to the Declaration of Helsinki and its current amendments. Informed consent was provided by patients or their legal guardian. SARS-CoV-2 diagnosis was confirmed by polymerase chain reaction testing. Sepsis was defined according to modified Sepsis 3 criteria by an increase of 2 points in the diagnostic sepsis-related organ failure assessment (SOFA) score.19 Exclusion criteria were pregnancy, aplasia, or extracorporeal membrane oxygenation (ECMO) therapy. Healthy control participants aged >18 years without self-reported antiplatelet medication, who were free from acute illness were recruited at the UKW at a routinely scheduled blood withdrawal by in-house physicians.
Additional methods are described in the supplemental data to this manuscript.
Results
In this study, we aimed to analyze platelet function in patients with COVID-19 in a direct comparison with sepsis. We recruited 37 patients with COVID-19 and 46 patients with sepsis or septic shock and compared them to 28 patients with infection without sepsis. These 111 patients (supplemental Figure 1) were recruited at the day of hospital or intensive care unit (ICU) admission (t1) and compared with 35 healthy control participants based on a normalization scheme (supplemental Table 1; supplemental Figure 2) to allow for comparison between cohorts. Blood of patients in ICUs was additionally analyzed after 4 to 7 days (t2). Including our follow-up analyses, a total of 159 patient samples were assessed. Most patients with COVID-19 (95%) and with sepsis (87%) were recruited at the ICU (n = 69), indicating critical illness in both cohorts. This was reflected by a similar median SOFA score (8; interquartile range [IQR], 4-9 vs 6; IQR, 4-8) and mortality (20% vs 16%) (Table 1).
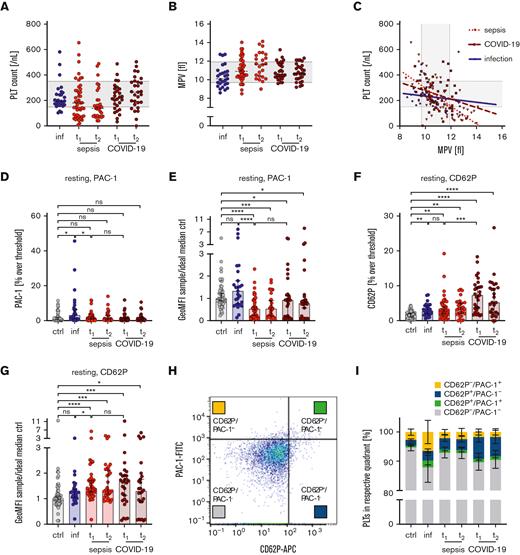
Uncoupled GPIIb/IIIa activation and α-granule release in COVID-19
Thrombocytopenia is a hallmark of sepsis and component of the diagnostic SOFA score.20 Accordingly, at t1, thrombocytopenia was more frequent in the sepsis cohort than in the infection cohort (47% vs 11%). By contrast, only 25% of the patients with COVID-19 in this study were thrombocytopenic (Figure 1A). This discrepancy was preserved at t2, with 59% of the patients having a low platelet count in the sepsis compared with 21% in the COVID-19 cohort. MPV inversely correlated with platelet counts, implying that larger-sized platelets are a direct consequence of thrombocytopenia-triggered thrombopoiesis (r2 sepsis, 0.43; P < .0001; r2 COVID-19, 0.07; P < .048) (Figure 1B-C). Plasma fibrinogen and D-dimer levels were increased throughout all cohorts (supplemental Figure 3A-B). The number of patients who had prolonged international normalized ratio was higher in the sepsis (n = 22) compared with the COVID-19 cohort (n = 3) (supplemental Figure 3C), which is also reflected by an increased sepsis-induced coagulopathy score in sepsis (supplemental Figure 3D).
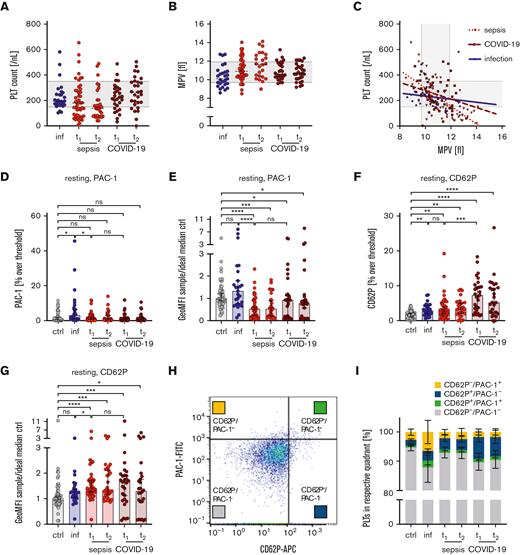
Increased GPIIb/IIIa activation and CD62P exposition in resting platelets in patients with sepsis or COVID-19. Characteristics of healthy control participants (ctrl) and patients with infection (inf), sepsis, or COVID-19 are displayed on hospital/ICU admission day (t1) and days 4 to 7 (t2).Platelet counts (A), mean platelet volume (MPV) (B), and platelet count vs MPV (C) are displayed. Platelet preactivation due to GPIIb/IIIa activation (D-E) or CD62P exposure (F-G) was assessed under resting conditions by flow cytometry. Events >2% threshold applied for healthy donors are displayed in panels D and F. Relative GeoMFI are shown in panels E and G. (H-I) Quadrant analysis of CD62P and PAC-1+ events under resting conditions. Panels A-C show reference ranges as dashed lines. Panels A and B display median, panels D-G show median ± 95% confidence interval (CI), and panel I shows mean ± 95 CI. Differences were analyzed using the Kruskal-Wallis test. ∗P < .05, ∗∗P < .01, ∗∗∗P < .001, ∗∗∗∗P < .0001. APC, allophycocyanin; FITC, fluorescein isothiocyanate; GeoMFI, geometric mean fluorescence intensity; ns, not significant; PLT, platelet.
Increased GPIIb/IIIa activation and CD62P exposition in resting platelets in patients with sepsis or COVID-19. Characteristics of healthy control participants (ctrl) and patients with infection (inf), sepsis, or COVID-19 are displayed on hospital/ICU admission day (t1) and days 4 to 7 (t2).Platelet counts (A), mean platelet volume (MPV) (B), and platelet count vs MPV (C) are displayed. Platelet preactivation due to GPIIb/IIIa activation (D-E) or CD62P exposure (F-G) was assessed under resting conditions by flow cytometry. Events >2% threshold applied for healthy donors are displayed in panels D and F. Relative GeoMFI are shown in panels E and G. (H-I) Quadrant analysis of CD62P and PAC-1+ events under resting conditions. Panels A-C show reference ranges as dashed lines. Panels A and B display median, panels D-G show median ± 95% confidence interval (CI), and panel I shows mean ± 95 CI. Differences were analyzed using the Kruskal-Wallis test. ∗P < .05, ∗∗P < .01, ∗∗∗P < .001, ∗∗∗∗P < .0001. APC, allophycocyanin; FITC, fluorescein isothiocyanate; GeoMFI, geometric mean fluorescence intensity; ns, not significant; PLT, platelet.
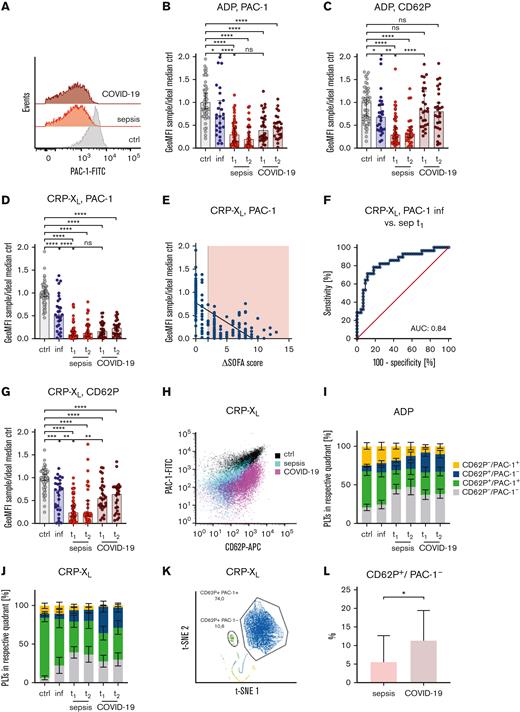
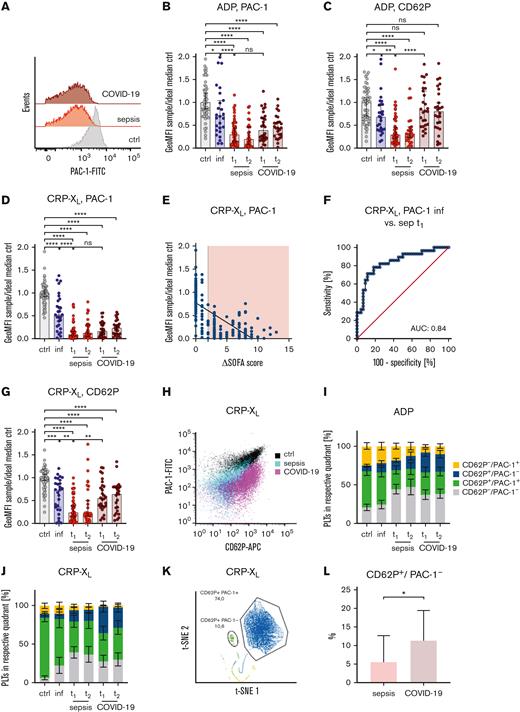
Platelet activation induces 2 main cellular responses: the release of internally stored granules (mostly α- and δ-granules) and activation of the integrin receptor GPIIb/IIIa. The latter results in a high affinity conformation for fibrinogen,21 which can be specifically detected by PAC-1 antibody binding. In order to assess whether any disease condition results in preactivated platelets, we have set resting platelets of healthy control participants to a 2% threshold but could not detect increased PAC-1 binding in any of the patient cohorts (Figure 1D). The same finding was observed when normalized GeoMFI values were compared (Figure 1E). CD62P is not expressed on resting platelets, and its exposure is thus a direct consequence of α-granule release. When applying the 2% threshold gate to healthy control participants, there was only a minor increase of CD62P in patients with COVID-19 (7.3%), sepsis (3%), or infection (2.8%) (Figure 1F). GeoMFI levels were slightly elevated in patients with COVID-19 or sepsis (Figure 1G) but far from the range observed for activated platelets (gray bar in supplemental Figure 4A), suggesting that circulating platelets in our patient cohorts are not fully activated. Integrin activation and granule release typically occur concomitantly but can also be uncoupled, as recently described for patients with COVID-19.16 We thus set up a quadrant analysis by gating on CD62P+ and PAC-1+ single- and double-positive subpopulations (Figure 1H). We found a shift toward CD62P+/PAC1− platelets (displayed in blue), which was more pronounced in patients with COVID-19 compared with those with sepsis (Figure 1I). Next, we assessed platelet function upon stimulation with adenosine 5′-diphosphate (ADP) (5 μM) or thrombin receptor-activating peptide 6 (TRAP-6) (5 μM), both binding to G protein–coupled receptors. GPIIb/IIIa activation in response to ADP was markedly downregulated in sepsis and COVID-19 platelets, whereas an intermediate pattern was observed in patients with infection (Figure 2A-B). Agonist-triggered CD62P exposure was also largely reduced in patients with sepsis (median relative GeoMFI, 0.29); however, unexpectedly, it was only minimally reduced in patients with COVID-19 (median relative GeoMFI, 0.83) (Figure 2C). Similar results were obtained for TRAP-6 (supplemental Figure 4B-C). Upon stimulation of the immunoreceptor GPVI with CRP-XL (0.01 μg/mL), platelets from the infection cohort showed a broad distribution of GPIIb/IIIa activation (median relative GeoMFI, 0.53 compared with 1.0 in healthy control participants), whereas PAC-1 binding was virtually abrogated in patients with COVID-19 (0.17) or sepsis (0.10) (Figure 2D). This degree of GPIIb/IIIa dysfunction correlated with disease severity, reflected by an increased SOFA score (Pearson correlation coefficient [r], −0.63; P < .0001) (Figure 2E), and robustly separated patients of the infection cohort from the sepsis cohort, already at disease onset (AUC, 0.84) (Figure 2F). GPIIb/IIIa activation upon stimulation was even more decreased in nonsurvivors compared with survivors, without being statistically significant (CRP-XL median relative GeoMFI sepsis survival, 0.20; deceased, 0.14 and COVID-19 survival, 0.11; deceased, 0.04) (supplemental Figure 4D-E). These results underline our previous findings that platelet dysfunction occurs already at sepsis onset, preceding the drop in platelet count and might help improve early diagnosis.22 Similar to ADP, CD62P exposure upon CRP-XL stimulation in patients with COVID-19 was far less affected (median relative GeoMFI, 0.55), which is in strong contrast to patients with sepsis (median relative GeoMFI, 0.24) (Figure 2G). In addition, in a small subgroup of patients with viral sepsis (Epstein-Barr virus or enterovirus), CD62P exposure after CRP-XL stimulation was significantly lower than in patients with COVID-19, which implies that the underlying pathomechanisms between sepsis and SARS-CoV-2 are distinct (supplemental Figure 4F). Quadrant analysis after CRP-XL stimulation unexpectedly revealed a clear separation of COVID-19 and sepsis (Figure 2H); we found 21% CD62P+/PAC-1− platelets in patients with COVID-19 after ADP stimulation, compared with only 12% in patients with sepsis (blue bars in Figure 2I). This difference was also observed upon stimulation with CRP-XL (27% vs 11%) (Figure 2J). As our analysis might be biased with respect to the choice of quadrants, we decided to corroborate our findings independently in a subcohort of patients, where we performed an unbiased automated clustering approach. By using FlowSOM software,23,24 we identified an increased subpopulation of CD62P+/PAC-1− platelets upon CRP-XL or ADP stimulation, predominantly in the COVID-19 cohort (Figure 2K-L). Taken together, the findings from our comprehensive function analysis provide several lines of evidence that platelets in patients with COVID-19 acquire a distinct, disease-specific dysfunctional pattern comprising an uncoupling between GPIIb/IIIa activation and α-granule release, which is different in patients with sepsis. Next, we asked whether there were differences with respect to a procoagulant platelet phenotype, characterized by breakdown of the mitochondrial membrane potential or increased phosphatidylserine (PS) exposure on the platelet surface that will trigger and finally boost the coagulation cascade.25 We assessed the mitochondrial membrane potential by tetramethylrhodamine ethyl ester staining and PS exposure by annexin V (AV) binding in a subset of participating patients with sepsis or COVID-19. The tetramethylrhodamine ethyl ester signal intensity was markedly reduced in patients with either COVID-19 or sepsis, accompanied by an increased fraction of AV+ platelets (supplemental Figure 5A-B), suggesting a procoagulant platelet phenotype in both disorders that contributes to the altered function observed.
Uncoupled GPIIb/IIIa activation and α-granule release in COVID-19. Characteristics of healthy control participants (ctrl), patients with infection (inf), sepsis, or COVID-19 are displayed on hospital/ICU admission day (t1) and days 4 to 7 (t2). Whole blood was preincubated with ADP (5 μM) (A-C) or CRP-XL (0.01 μg/mL) (D-G) for 5 minutes. Panels A, B, and D-F show GPIIb/IIIa activation, and panels C and G show CD62P exposition measured flow cytometrically. (E) CRP-XL–induced GPIIb/IIIa activation vs SOFA score, red area indicates patients fulfilling Sepsis 3 criteria. (F) Receiver operating characteristic curve analysis of GPIIb/IIIa activation between patients with infection and patients with sepsis at t1 upon CRP-XL stimulation. (H-J) Quadrant analysis of CD62P− and PAC-1+ events upon ADP (I) or CRP-XL (J) stimulation. (K-L) Automated clustering analysis of patients with sepsis (n = 9) and patients with COVID-19 (n = 9) upon CRP-XL stimulation. Representative curves are shown in panels A, H, and K. All graphs show median ± IQR except panels I and J that display mean ± 95% CI. Differences were analyzed using the Kruskal-Wallis test (B-J) or Kolmogorov-Smirnov test (L). ∗P < .05, ∗∗P < .01, ∗∗∗P < .001, ∗∗∗∗P < .0001. AUC, area under the curve; CRP-XL, collagen-related peptide cross-linked.
Uncoupled GPIIb/IIIa activation and α-granule release in COVID-19. Characteristics of healthy control participants (ctrl), patients with infection (inf), sepsis, or COVID-19 are displayed on hospital/ICU admission day (t1) and days 4 to 7 (t2). Whole blood was preincubated with ADP (5 μM) (A-C) or CRP-XL (0.01 μg/mL) (D-G) for 5 minutes. Panels A, B, and D-F show GPIIb/IIIa activation, and panels C and G show CD62P exposition measured flow cytometrically. (E) CRP-XL–induced GPIIb/IIIa activation vs SOFA score, red area indicates patients fulfilling Sepsis 3 criteria. (F) Receiver operating characteristic curve analysis of GPIIb/IIIa activation between patients with infection and patients with sepsis at t1 upon CRP-XL stimulation. (H-J) Quadrant analysis of CD62P− and PAC-1+ events upon ADP (I) or CRP-XL (J) stimulation. (K-L) Automated clustering analysis of patients with sepsis (n = 9) and patients with COVID-19 (n = 9) upon CRP-XL stimulation. Representative curves are shown in panels A, H, and K. All graphs show median ± IQR except panels I and J that display mean ± 95% CI. Differences were analyzed using the Kruskal-Wallis test (B-J) or Kolmogorov-Smirnov test (L). ∗P < .05, ∗∗P < .01, ∗∗∗P < .001, ∗∗∗∗P < .0001. AUC, area under the curve; CRP-XL, collagen-related peptide cross-linked.
Deficient δ-granule secretion in critical infection
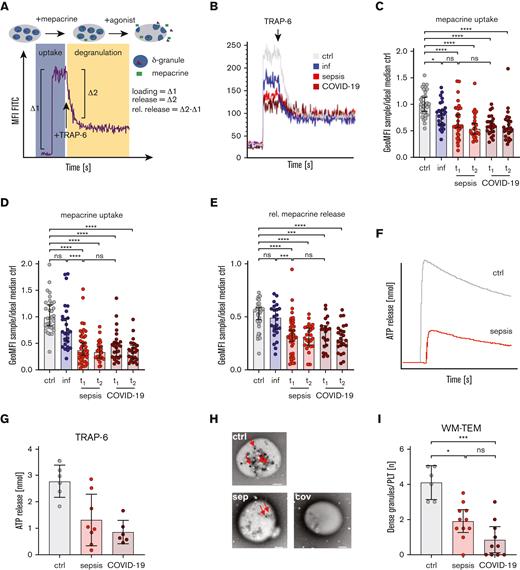
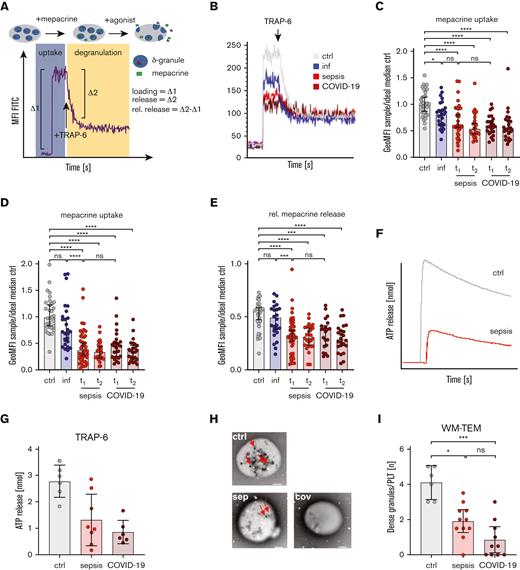
During the initial phase of platelet activation, δ-granules become exocytosed and release mediators including ADP, serotonin, and polyphosphates. ADP can induce further autocrine and paracrine activation, mediating the second wave of platelet aggregation. δ-granule function depends mainly on the number of granules, their contents, and finally the potential to release the cargo. We assessed δ-granule loading and release by a kinetically resolved flow cytometric assay using mepacrine, which selectively incorporates into δ-granules. We recorded the fluorescence of unstained and mepacrine-loaded platelets and calculated the difference as a surrogate marker for the number of δ-granules (Figure 3A). Most patients with sepsis or COVID-19 showed a markedly reduced mepacrine uptake (median relative MFI: control, 1.00; infection, 0.81; sepsis t1, 0.53; COVID-19 t1, 0.58) on the day of hospital admission (Figure 3B-C). Mepacrine release upon TRAP-6 (5 μM) stimulation was decreased in patients with infection compared with control participants but not to the same extent as in sepsis or COVID-19 (Figure 3B,D). The proportion of released to loaded mepacrine (“relative mepacrine release”) was reduced, suggesting a combined “uptake-and-release” defect (Figure 3B,E). In a subset of patients with COVID-19 or sepsis, we additionally performed lumiaggregometry, which monitors the release of δ-granule–derived ATP. Upon stimulation with either TRAP-6 or thrombin, ATP release was markedly reduced in patients with COVID-19 or sepsis compared with control participants (Figure 3F-G; supplemental Figure 5C). Next, we determined the number of δ-granules in critically ill patients by whole-mount transmission electron microscopy. We detected 3 to 5 δ-granules per platelet in the control sample (n = 6) but only 0 to 3 granules per platelet in patients with sepsis (n = 11) or COVID-19 (n = 10) (Figure 3H-I). Taken together, our data indicate an acquired, substantial δ-granule deficiency in critically ill patients with COVID-19 or sepsis, mainly due to a reduced number of δ-granules.
δ-granule deficiency in patients with sepsis or COVID-19. Characteristics of healthy control participants (ctrl), patients with infection (inf), sepsis, or COVID-19 are displayed on hospital/ICU admission day (t1) and days 4 to 7 (t2). (A-E) Schematic visualization of mepacrine assay depicted in panel A. Mepacrine uptake (C) and release (D) upon TRAP-6 stimulation (5 μM) were quantified in whole blood using flow cytometry. (E) Relative (rel.) mepacrine release was determined by calculating the relation of mepacrine uptake/release. (F-G) Adenosine triphosphate (ATP) release upon TRAP-6 stimulation (10 μM) was determined in platelet-rich plasma by lumiaggregometry (minimal platelet count > 150/nL). (H-I) Number of δ-granules was determined in platelet-rich plasma using WM-TEM. (H) Representative images are shown, red arrows indicate δ-granules. Scale bars indicate 1 μm. (I) Dots show median δ-granule number per platelet calculated in a 2 investigator–blinded approach. Representative figures are displayed in panels B, F, and H. All graphs show median ± 95% CI. Differences were analyzed using the Kruskal-Wallis test. ∗P < .05, ∗∗P < .01, ∗∗∗P < .001, ∗∗∗∗P < .0001.
δ-granule deficiency in patients with sepsis or COVID-19. Characteristics of healthy control participants (ctrl), patients with infection (inf), sepsis, or COVID-19 are displayed on hospital/ICU admission day (t1) and days 4 to 7 (t2). (A-E) Schematic visualization of mepacrine assay depicted in panel A. Mepacrine uptake (C) and release (D) upon TRAP-6 stimulation (5 μM) were quantified in whole blood using flow cytometry. (E) Relative (rel.) mepacrine release was determined by calculating the relation of mepacrine uptake/release. (F-G) Adenosine triphosphate (ATP) release upon TRAP-6 stimulation (10 μM) was determined in platelet-rich plasma by lumiaggregometry (minimal platelet count > 150/nL). (H-I) Number of δ-granules was determined in platelet-rich plasma using WM-TEM. (H) Representative images are shown, red arrows indicate δ-granules. Scale bars indicate 1 μm. (I) Dots show median δ-granule number per platelet calculated in a 2 investigator–blinded approach. Representative figures are displayed in panels B, F, and H. All graphs show median ± 95% CI. Differences were analyzed using the Kruskal-Wallis test. ∗P < .05, ∗∗P < .01, ∗∗∗P < .001, ∗∗∗∗P < .0001.
Low-dose GPIIb/IIIa blockade prevents thrombus formation in COVID-19
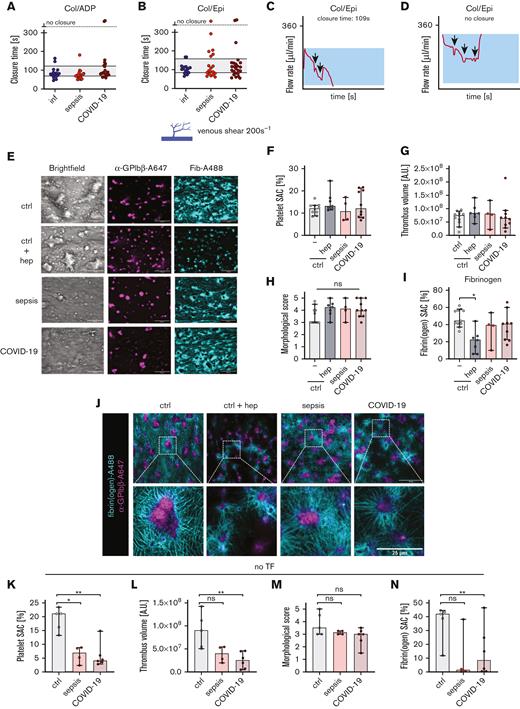
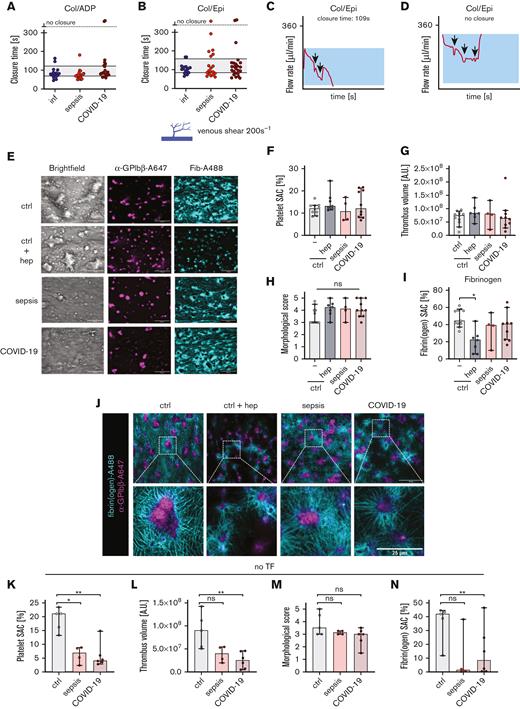
Next, we assessed the functional relevance of these defects under flow conditions by using the platelet function analyzer PFA-200. This point-of-care device is considered to provide a surrogate “in vitro bleeding time,” reflecting the time until a collagen/epinephrine- or collagen/ADP-coated aperture is closed under a standardized shear rate. Unexpectedly, sample from 18 out of 19 patients with sepsis and 23 out of 25 patients with COVID-19 revealed full closure of the collagen/epinephrine cartridge, mostly within the reference range (Figure 4A-B). In addition to the detected closure time as an end point analysis, the aggregation kinetics were further monitored until full closure and displayed as histograms. In healthy donors, the flow rate decreased linearly over time, whereas we often observed a sawtooth pattern in blood derived from patients with COVID-19 or sepsis (Figure 4C-D), reflecting possible embolization and thrombus rupture at the aperture. Thrombus formation depends on the interplay of platelet activation with the coagulation cascade.26,27 We thus evaluated platelet function in conjunction with fibrin formation on collagen- and TF-coated coverslips in a flow chamber using recalcified whole blood. Under venous shear rates, platelet aggregation (Figure 4E), indicated by platelet SAC (Figure 4F) as well as thrombus volume, morphology, and contraction score (Figure 4G-H; supplemental Figure 6A-C) were comparable between patients with COVID-19 or sepsis and healthy control participants. Thrombin-mediated fibrin formation was slightly reduced both in patients with COVID-19 and sepsis (Figure 4I), most likely owing to the anticoagulation therapy. In vitro–heparinized whole blood of healthy control participants reduced fibrin formation but did not impact platelet aggregation and thrombus formation (Figure 4E-I; supplemental Figure 6A-C). Unexpectedly, fibrin(ogen) deposition was higher in sepsis or COVID-19 samples compared with in vitro–heparinized control samples but not to the same extent as control samples, suggesting that hypercoagubility might occur under low shear, independent of heparin. Confocal imaging confirmed similar clot composition of these thrombi in patients and control participants (Figure 4J). Unexpectedly, when external TF was omitted, platelet aggregation, thrombus volume, and fibrin formation were markedly reduced both in sepsis and COVID-19 samples when compared with control samples. This implies that the TF-dependent interplay with the coagulation cascade could rescue the reduced platelet function we observed in patients (Figure 4K-N; supplemental Figure 6D-F). We monitored distinct activities of the coagulation cascade by rotational thromboelastometry and found a slightly increased coagulability in a subset of patients with sepsis and COVID-19 (supplemental Figure 7), especially in FIBTEM, when platelet function becomes blocked through cytochalasin D, reflecting a procoagulable state and increased fibrinogen plasma levels.
Unaltered in vitro bleeding time in sepsis or COVID-19. (A-D) In vitro bleeding time was mimicked using PFA-200 in whole blood (minimal platelet count > 150/nL). Representative figures are displayed in panels C and D. Arrows indicate sawtooth pattern–like events. Reference ranges are highlighted in panels A and B. (E-N) Thrombus and fibrin formation were assessed under venous shear (200 s−1) using recalcified whole blood on collagen/tissue factor (TF) (E-J) or collagen-coated spots (K-N). Samples were stained for platelets (α-GPIbβ-Alexa647, magenta) and fibrin(ogen) (cyan). Panels F and K show surface area coverage (SAC, %) of platelets, panels G and L show platelet fluorescence intensity in arbitrary units (AUs), panels H and M show the morphological score evaluated by 2 blinded investigators, and in panels I and N, fibrin(ogen) SAC are displayed. Representative images from 1 focal plane are depicted in panel E. Scale bars indicate 50 μm. In panel J, thrombi were imaged in 1 focal plane using confocal microscopy. Scale bar in upper images indicates 50 μm and lower images indicates 25 μm. All graphs show median ± 95% CI. Differences were analyzed using the Kruskal-Wallis test. Col/ADP, collagen/ADP; Col/Epi, collagen/epinephrine; hep, heparin.
Unaltered in vitro bleeding time in sepsis or COVID-19. (A-D) In vitro bleeding time was mimicked using PFA-200 in whole blood (minimal platelet count > 150/nL). Representative figures are displayed in panels C and D. Arrows indicate sawtooth pattern–like events. Reference ranges are highlighted in panels A and B. (E-N) Thrombus and fibrin formation were assessed under venous shear (200 s−1) using recalcified whole blood on collagen/tissue factor (TF) (E-J) or collagen-coated spots (K-N). Samples were stained for platelets (α-GPIbβ-Alexa647, magenta) and fibrin(ogen) (cyan). Panels F and K show surface area coverage (SAC, %) of platelets, panels G and L show platelet fluorescence intensity in arbitrary units (AUs), panels H and M show the morphological score evaluated by 2 blinded investigators, and in panels I and N, fibrin(ogen) SAC are displayed. Representative images from 1 focal plane are depicted in panel E. Scale bars indicate 50 μm. In panel J, thrombi were imaged in 1 focal plane using confocal microscopy. Scale bar in upper images indicates 50 μm and lower images indicates 25 μm. All graphs show median ± 95% CI. Differences were analyzed using the Kruskal-Wallis test. Col/ADP, collagen/ADP; Col/Epi, collagen/epinephrine; hep, heparin.
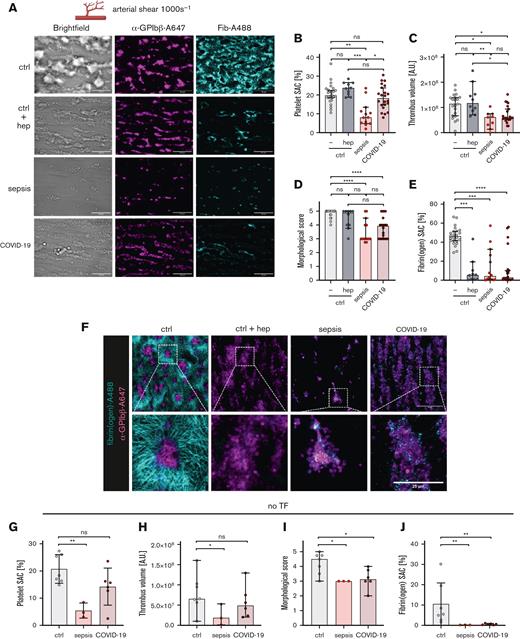
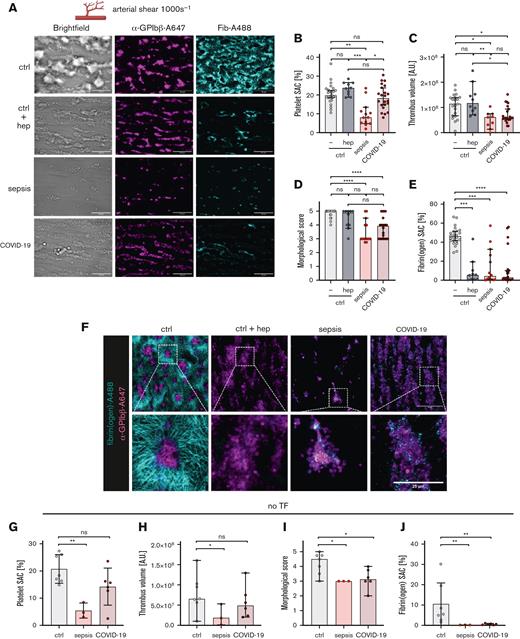
Under arterial shear rates (Figure 5A-F), platelet aggregate formation was markedly reduced in patients with sepsis (median platelet SAC, 8.2%; MS, 3%), whereas an overall stable thrombus formation (median platelet SAC, 18.3%; MS, 3.9%) was revealed in patients with COVID-19. Thrombi were increased in number but were smaller in individual size compared with control participants (Figure 5A-B). Quantitative imaging of formed thrombi revealed decreased thrombus volume, multilayer score (MLS), and contraction score (CS) scores both in patients with COVID-19 or sepsis (Figure 5C-D, supplemental Figure 8A-C). Fibrin formation was markedly reduced under arterial shear (Figure 5E). To evaluate whether the anticoagulation administered to patients in the ICU had any confounding effect in our assays, we added unfractionated heparin (final concentration, 2 U/mL) to whole blood of healthy control participants and repeated the flow chamber experiments. In line with our patient results, fibrin(ogen) SAC was abrogated upon heparinization (Figure 5A,E). We detected quantitatively more, but less contracted thrombi, comparable with COVID-19 samples (Figure 5A-E; supplemental Figure 8A-C), whereas thrombus volume remained unaltered (median, 1.2 × 108 AU). This implies that anticoagulation therapy led to altered aggregate morphology in COVID-19 but did not account for the reduced thrombus volume. This was confirmed in clots generated under arterial shear by a refined analysis using confocal microscopy; blood from healthy control participants formed a dense fibrin(ogen) network and roundish thrombi, whereas patients with COVID-19 exhibited reduced fibrin(ogen) formation and flat thrombi, corresponding to heparinized healthy control samples (Figure 5F). When thrombus formation was assessed without external TF, platelet aggregation and thrombus volume did not differ between patients with COVID-19 and control participants, which is in contrast to the measurements under venous shear rates (Figure 5G-J; supplemental Figure 8D-F). This observation suggests that robust thrombus formation in COVID-19 samples under arterial shear rates is not primarily mediated by TF. Taken together, our data provide evidence that platelets of patients with COVID-19 form stable but less 3-dimensional thrombi, despite the defective granule secretion and virtually absent GPIIb/IIIa activation.
Robust thrombus formation despite anticoagulation in COVID-19. (A-J) Thrombus and fibrin formation were assessed under arterial shear (1000 s−1) using recalcified whole blood on collagen/TF (A-F) or collagen-coated spots (G-J). Samples were stained for platelets (α-GPIbβ-Alexa647, magenta) and fibrin(ogen) (cyan). SAC (%) of platelets (B and G), platelet fluorescence intensity in AUs (C and H), morphological score evaluated by 2 blinded investigators (D and I), and fibrin(ogen) SAC (E and J) are displayed. Representative images from 1 focal plane are depicted in panel A and scale bars indicate 50 μm. (F) Thrombi were imaged in 1 focal plane using confocal microscopy, scale bar in upper images indicates 50 μm and lower images indicates 25 μm. All graphs show median ± 95% CI. Differences were analyzed using the Kruskal-Wallis test. ∗P < .05, ∗∗P < .01, ∗∗∗P < .001, ∗∗∗∗P < .0001.
Robust thrombus formation despite anticoagulation in COVID-19. (A-J) Thrombus and fibrin formation were assessed under arterial shear (1000 s−1) using recalcified whole blood on collagen/TF (A-F) or collagen-coated spots (G-J). Samples were stained for platelets (α-GPIbβ-Alexa647, magenta) and fibrin(ogen) (cyan). SAC (%) of platelets (B and G), platelet fluorescence intensity in AUs (C and H), morphological score evaluated by 2 blinded investigators (D and I), and fibrin(ogen) SAC (E and J) are displayed. Representative images from 1 focal plane are depicted in panel A and scale bars indicate 50 μm. (F) Thrombi were imaged in 1 focal plane using confocal microscopy, scale bar in upper images indicates 50 μm and lower images indicates 25 μm. All graphs show median ± 95% CI. Differences were analyzed using the Kruskal-Wallis test. ∗P < .05, ∗∗P < .01, ∗∗∗P < .001, ∗∗∗∗P < .0001.
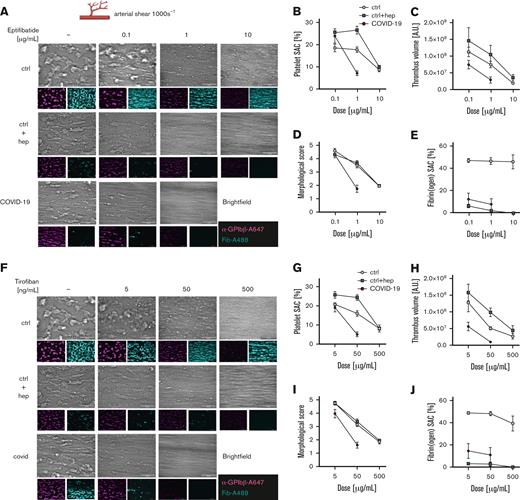
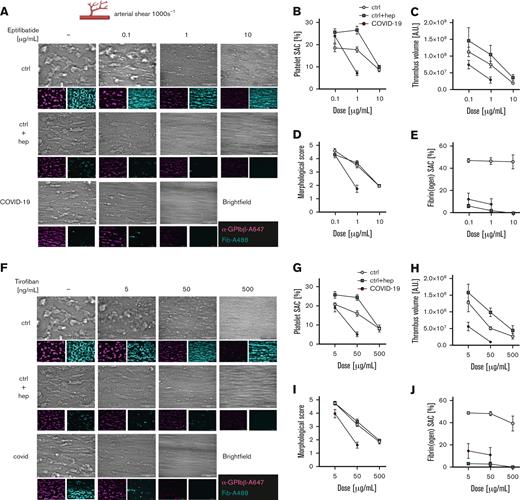
Because patients with COVID-19 often have thrombotic complications, we finally questioned whether the abrogated GPIIb/IIIa activation (Figure 2B,D; supplemental Figure 4B) in conjunction with an overall unaltered thrombus formation under flow conditions (Figure 5A-F) could be a therapeutic target to control thrombus formation. We preincubated whole blood of patients and control participants for 20 minutes with increasing doses of the clinically approved GPIIb/IIIa blocker eptifibatide and applied arterial flow conditions in our microfluidic chamber. In healthy and heparinized control samples, low doses of eptifibatide scarcely affected platelet SAC (mean 0.1 μg/mL, 19%; mean 1 μg/mL, 18%) and a dose of 10 μg/mL was required to fully reduce the platelet SAC (mean, 8%). We measured low thrombus volume (mean, 1.8 × 107 AU), CS, and MLS (both mean, 0), indicating loose aggregates of few platelets adhering to collagen fibers, whereas fibrin formation was unaffected. Intriguingly, 1 μg/mL eptifibatide was already sufficient to fully prevent thrombus formation in patients with COVID-19, 10-fold less compared with the dosage required to affect thrombus formation in heparinized control samples (Figure 6A-E; supplemental Figure 9A-C). This implies that the reduced dosage necessary to affect thrombus formation in COVID-19 is less likely due to anticoagulation but rather intrinsic to the disease condition. Finally, to exclude a specific effect of eptifibatide, we repeated the experiment with tirofiban. Again, a 10-fold reduced dosage (50 ng/mL) abrogated thrombus formation in patients with COVID-19, whereas 500 ng/mL was required in blood derived from healthy donors, independent of heparinization (Figure 6F-J; supplemental Figure 9D-F). This confirms our results obtained with eptifibatide. Taken together, our data suggest that low-dose GPIIb/IIIa blockade could be a promising target for antithrombotic therapy in patients with COVID-19.
Low-dose GPIIb/IIIa blockade reduces thrombus formation in patients with COVID-19. Characteristics of control participants (ctrl) (n = 9), in vitro–heparinized control samples (n = 8), and patients with COVID-19 (n = 10) are displayed. Thrombus and fibrin formation on collagen/TF spots were assessed under arterial shear (1000 s−1) in recalcified whole blood after preincubation with eptifibatide (A-E) or tirofiban (F-J). Platelets are displayed in magenta and fibrin(ogen) in cyan. SAC (%) of platelets (B and G), platelet fluorescence intensity in AUs (C and H), morphological score depicted by 2 blinded investigators (D and I), and fibrin(ogen) SAC (E and J) are displayed. Representative images from 1 focal plane are depicted in panels A and F; scale bars indicate 50 μm. All graphs show mean ± standard error of the mean. Differences were analyzed using the Kruskal-Wallis test. ∗P < .05, ∗∗P < .01, ∗∗∗P < .001, ∗∗∗∗P < .0001.
Low-dose GPIIb/IIIa blockade reduces thrombus formation in patients with COVID-19. Characteristics of control participants (ctrl) (n = 9), in vitro–heparinized control samples (n = 8), and patients with COVID-19 (n = 10) are displayed. Thrombus and fibrin formation on collagen/TF spots were assessed under arterial shear (1000 s−1) in recalcified whole blood after preincubation with eptifibatide (A-E) or tirofiban (F-J). Platelets are displayed in magenta and fibrin(ogen) in cyan. SAC (%) of platelets (B and G), platelet fluorescence intensity in AUs (C and H), morphological score depicted by 2 blinded investigators (D and I), and fibrin(ogen) SAC (E and J) are displayed. Representative images from 1 focal plane are depicted in panels A and F; scale bars indicate 50 μm. All graphs show mean ± standard error of the mean. Differences were analyzed using the Kruskal-Wallis test. ∗P < .05, ∗∗P < .01, ∗∗∗P < .001, ∗∗∗∗P < .0001.
Discussion
Patients with COVID-19 have an increased risk of thromboembolic events, including venous thromboembolism and venous or arterial thrombosis.28 The aim of our study was to perform a comprehensive analysis of altered platelet function in patients with COVID-19, especially in direct comparison with sepsis or infection. We provide experimental evidence that platelet responses to various agonists are selectively blunted or dimmed and that GPIIb/IIIa activation and δ-granule release become uncoupled from α-granule exocytosis. This separation has already been reported by Manne et al,16 where it was primarily attributed to virus-based disorders. Our data suggest that there might be a particular contribution by SARS-CoV-2 to this uncoupling, as patients with sepsis other than SARS-CoV-2–induced sepsis did not show this effect, but our numbers are yet too small. In patients with sepsis, the consumption of coagulation factors and platelets will result in thrombocytopenia and DIC.29 In the initial phase of COVID-19, however, DIC or thrombocytopenia are less frequently observed. Alterations in coagulation parameters have been broadly studied in both disorders, including differences among them.30,31 With respect to platelet function, however, a detailed comparison between COVID-19 and sepsis is missing. Moreover, seminal reports on platelet dysfunction in COVID-19 are somewhat controversial, concluding that platelets in COVID-19 are either hyporeactive9,17 or hyperreactive.16,18,32,33 The results of our study provide comprehensive evidence that these controversial results might be less contradicting; we found platelets of patients with COVID-19 or sepsis to be hyporeactive with respect to integrin GPIIb/IIIa activation when compared with healthy control participants or patients with infections. In 2 studies on platelet function in COVID-19, the authors found increased platelet aggregation in response to suboptimal agonist concentrations.32,33 In our study, we have mainly used optimal agonist concentrations, which might partly explain the differences. The data derived from our microfluidic flow chamber experiments further corroborate that COVID-19–derived platelets reveal an unexpectedly strong adhesion and thrombus formation, despite their defective integrin activation and despite the presence of heparin, which is in agreement with the increased platelet adhesion on collagen observed by Zaid et al.32 One possible mechanism of how platelets in patients with COVID-19 mediate thrombus formation despite an overall deficient GPIIb/IIIa activation could be an increased PS exposure on the outer membrane leaflet, which is the base for activation of the tenase and prothrombinase complexes, preceding full activation of the coagulation cascade. We found an increased fraction of procoagulant platelets in untreated whole blood of patients with sepsis or COVID-19 (supplemental Figure 5A) and observed AV+ platelets also in our coagulation flow chamber (supplemental Figure 10). Procoagulant platelets in samples from patients with COVID-19 have also been described by other groups;8,34,35 especially, purified immunoglobulin G fractions from patients with COVID-19 were reported to harbor this increased capacity in addition to the classical agonists used in this study.8 These immunoglobulin G–induced procoagulant platelets could thus partly compensate for a deficient platelet function. It is feasible that a consumption of more active platelets in vivo (ie, in platelet-rich thrombi) would ultimately result in an increased fraction of less reactive (“exhausted”) platelets subjected to in vitro studies, but the overall short platelet half-life makes this option unlikely. This might also be reflected in the only partially altered fraction of “secreted-only” CD62P+/PAC-1− platelet subpopulation that might play a role in the hyperaggregable platelet phenotype. Further work will be required to decipher the role of distinct platelet subpopulations in sepsis and COVID-19. In a recent work using a murine lipopolysaccharide–induced lung injury model, it was shown that especially GPVI and GPIIb/IIIa function are crucial for inducing a PS-exposing procoagulant phenotype.36 Nevertheless, the criteria defining a procoagulant platelet are yet not well standardized.
We speculate that thrombi in COVID-19 might be susceptible for antithrombotic therapy. In our study, we provide experimental evidence that especially GPIIb/IIIa blockade might be effective for prevention and therapy of (micro)thrombotic events in patients with COVID-19. These drugs are known to increase the bleeding risk in some patients, but very recent findings strongly indicate reconsideration of this antithrombotic approach in thromboinflammatory conditions. In a recent publication in which a murine model of immune-triggered cerebral venous thrombosis was used, the authors provided compelling data that especially GPIIb/IIIa blockade could prevent thrombus formation, ischemia, and neurological damage, whereas anticoagulation using heparin did not have any therapeutic effect.37 This observation was partly unexpected in its clear result, because GPIIb/IIIa as a target would probably not be the first choice owing to the expected increased risk of bleeding. Similar findings were made in a murine model of thrombotic thrombocytopenic purpura.38 Although data on the use of GPIIb/IIIa blockers in COVID-19 and sepsis are limited, recent case reports described the successful use of eptifibatide or tirofiban in critically ill patients with acute respiratory distress or myocardial infarction during COVID-19.39,40 Here, we provide data that platelets of critically ill patients with COVID-19 are 10-fold more susceptible toward GPIIb/IIIa blockade with respect to adhesion in our flow chamber. This suggests that the minimal dosage of GPIIb/IIIa blockers in COVID-19 might need to be adapted for future clinical trials. CD62P might be a further candidate to target, although a study with patients with COVID-19 using crizanlizumab did not find statistically significant differences in the overall clinical outcome compared with the placebo control cohort.41
We monitored platelet function in conjunction with clinical parameters during the course of disease and could demonstrate consistent platelet-based defects. Because patients with COVID-19 have been continuously recruited from the beginning of the pandemic until June 2022, our data reflect all SARS-CoV-2 variants predominant in Germany and Europe (Wuhan, Alpha, Delta, and Omicron) and did not reveal significant differences between these subtypes, suggesting that platelet dysfunction in COVID-19 is intrinsic to an infection with SARS-CoV-2. One mechanism might be the inflamed lung tissue,42 which could serve as an activation trigger each time the platelet passes the lung, possibly by direct interaction between platelets and the SARS-CoV-2 spike protein.43
Our study has several limitations: (1) the data were generated in a single study center at UKW and (2) a large fraction of participating patients was recruited from ICUs and had been receiving pharmacological and interventional therapy. Treatment regimens between sepsis and COVID-19 differed regarding mechanical ventilation, anticoagulation, antiplatelet therapy, or hemodialysis, which could have potentially skewed our findings. In a previous study on platelet function in sepsis, we could not find any effect of obvious confounders like antibiotic treatment or platelet-bacterial interactions.22 We evaluated the impact of ventilation or hemodialysis by univariate analysis, without detecting any statistically significant effect. Of note, we excluded patients who required ECMO therapy at any time because ECMO is known to trigger platelet dysfunction and can cause an acquired von Willebrand factor–deficiency.44,45 Nevertheless, we are fully aware that other confounders may have an impact on platelet function. (3) Increased plasma fibrinogen levels could possibly outcompete the PAC-1 antibody and reduce signal intensity. We thus performed a correlation of plasma fibrinogen contents with PAC-1 binding and could not find any association between both parameters throughout all patient cohorts (supplemental Figure 11). (4) Most study participants with COVID-19 were given low-molecular weight heparin from day 1 in the ICU. Although this might be less critical for flow cytometry–based platelet function assays, it has relevant impact on coagulation-based assays, although we could find differences in few patients on fondaparinux or unfractionated heparin. We have thus heparinized blood from healthy donors in vitro in our flow chamber experiments, which could phenocopy the reduced fibrin formation but could not explain the overall stable thrombi found in COVID-19 or sepsis. A subfraction of patients received low-dose acetylsalicylic acid (infection, n = 8; sepsis, n = 4; COVID-19, n = 19), which might affect platelet function in some of our assay systems. (5) We cannot exclude that the partly reduced platelet count or lower hematocrit found in some patients might have had an effect in our coagulation flow chamber. In pilot experiments with artificially reduced hematocrit or thrombocytopenia, we found only a minor effect on our readouts (data not shown). (6) In our in vitro studies we focused on GPIIb/IIIa inhibitors, because we found that GPIIb/IIIa integrin activation was markedly reduced upon stimulation with various agonists (ADP, TRAP-6, and CRP-XL), suggesting a generalized platelet activation defect. Furthermore, the amount of blood available for experiments for each patient was limited owing to ethical reasons, so we could not perform each experiment with every patient. We can also not exclude that procoagulant platelet- or megakaryocyte-derived microparticles contributed to our findings. Of note, circulating platelet-derived extracellular vesicles were also described to be a hallmark finding of COVID-1946 but have not been assessed in this study.
In summary, our study provides evidence that in COVID-19, platelet α-granule release is uncoupled from an acquired defective GPIIb/IIIa activation, in contrast to the extensive platelet function defect found in patients with sepsis. This correlated with a robust thrombus formation in flow-based assays, which was prevented by eptifibatide or tirofiban but not with heparin. Our findings suggest that low-dose GPIIb/IIIa blockade could be a promising therapeutic target for patients with COVID-19, which should be further investigated in clinical trials.
Acknowledgments
The authors thank Nadine Winter for excellent technical and logistic support and Daniela Naumann for her help with the whole-mount transmission electron microscopy (WM-TEM). The investigators thank Sabrina Krauss for her service as consulting physician.
This work was supported by the Deutsche Forschungsgemeinschaft (German Research Foundation), grant 374031971-TR 240 (B.N. and H.S.), project 453989101-SFB 1525 (L.J.W., B.N., and S.F.), equipment grant 426173797 (H.S. and D.W.), and grants from the Interdisciplinary Center for Clinical Research grant A-442 (H.S. and D.W.) and grant Z-02/84 (M.D.).
Authorship
Contribution: L.J.W. conceptualized the study, designed and performed the experiments, analyzed the data, and wrote the manuscript; M.D., G.M., M.Z., J.K., M.W., J.H., K.M., S.B., and P.B. designed and performed the experiments and analyzed the data; T.-T.L., K.A., T.B., S.F., P.M., and B.N. provided intellectual input and analyzed the data; and D.W. and H.S. conceptualized the study, designed the experiments, analyzed the data, and wrote the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Harald Schulze, Institute for Experimental Biomedicine, University Hospital Würzburg, Josef-Schneider-str. 2, Haus D15, 97080 Würzburg, Germany; e-mail: harald.schulze@uni-wuerzburg.de.
References
Author notes
∗D.W. and H.S. contributed equally to this study.
Data are available on request from the corresponding author, Harald Schulze (harald.schulze@uni-wuerzburg.de).
The full-text version of this article contains a data supplement.