TO THE EDITOR:
Patients with hematologic malignancies treated with autologous (auto) and allogeneic (allo) hematopoietic cell transplantation (HCT) are at high risk of developing adverse outcomes related to severe acute respiratory syndrome coronavirus 2 (SARS-CoV-2) infection due to immune dysregulation, prolonged immunosuppression, graft-versus-host disease (GVHD), and cytopenias.1 The estimated incidence of SARS-CoV-2 infection in auto- and allo-HCT is 5.5% and 11%, respectively, with a mortality rate of approximately 20% in the allo-HCT compared with the 1.8% observed in the general United States population.1,2 Vaccination remains the most effective tool in preventing severe COVID-19 disease, hospitalization, and death, and immunization with messenger RNA (mRNA) SARS-CoV-2 vaccines has been highly recommended and prioritized in fragile patients, including HCT.3,4 SARS-CoV-2 mRNA vaccination has shown to overall induce high levels of antibodies in the majority of HCT after 2 vaccine doses, but some patients do not mount an appreciable immune response to SARS-CoV-2 vaccination (Pettini et al; manuscript in preparation).5 Therefore, a third vaccine dose capable of effectively boosting the immune system is particularly critical for low responders who could have a weakened and/or slowed immune priming.6
It was recently shown by Redjoul et al that the third dose of BNT162b2 mRNA (Pfizer-BioNTech) vaccine significantly increases the anti-SARS-CoV-2 antibodies in recipients of allo-HCT, but they also highlight the crucial need for further data on induction of antigen-specific B cells and functional antibodies.7
To address these fundamental open questions, we profiled the immune response induced after the third dose of the mRNA-1273 (Moderna) vaccine in HCT recipients with limited antibody response after 2 vaccine doses, analyzing both the RBD-specific B cells and the functionality of spike-specific antibodies. The present study analyzes 9 HCT recipients identified as low responders in the context of a clinical study including 80 patients (auto-HCT n = 23, allo-HCT n = 57; 58% male and 42% female; mean age of 56.7 years) enrolled at the Cellular Therapy Unit, Azienda Ospedaliera Universitaria Senese (Protocol Code 19479 PATOVAC_COV). These 9 HCT recipients (8 allogeneic and 1 autologous) were identified as low responders after 2 doses of mRNA-1273 vaccine based on the following criteria: low spike-specific immunoglobulin G (IgG) titers (with an increase <4 with respect to baseline, threshold indicated by the World Health Organization for Middle East respiratory syndrome coronavirus and confirmed for SARS-CoV-2)8 and ACE2/RBD binding inhibition <30% (threshold indicated by the manufacturer protocol). For these 9 low responder patients, a mean of 4.4 years (range 0.4-11.8 years) elapsed from HCT and the administration of the first mRNA-1273 vaccine dose, compared with a mean of 3 years (range 0.3-13) for the high responder patients included in the study cohort (Table 1). As described in Table 1, 55% of low responder patients were receiving an immunosuppressive treatment at the time of the first dose, and no changes in the treatment were registered until the time of the third vaccine dose. The exact time elapsed from the HCT and the specific treatment for each of the 9 patients is reported in Table 1.
They received the third mRNA-1273 dose 6 months after the second, and spike-specific antibodies, ACE2/RBD binding inhibition and RBD-specific B cells, were analyzed before (day 180) and 7 days after (day 187) the third dose. The study was performed in compliance with all relevant ethical regulations, and the protocol was approved by the local Ethical Committee for Clinical Experimentation of Regione Toscana Area Vasta Sud Est (CEAVSE). The study was conducted in accordance with the Declaration of Helsinki.
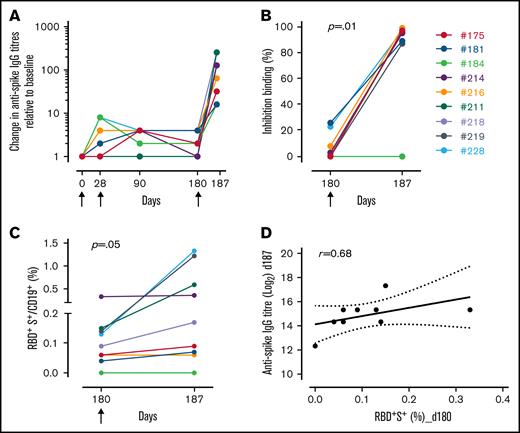
A significant increase of spike-specific IgG titers (assessed as previously detailed in Fiorino et al)6 is observed after the third dose in 100% of the subjects, with an average increase of 128 folds and a geometric mean titer of 32 509 (95% confidence interval [CI], 6583-1600; titers range 5120-163 840 at day 187) vs an average increase of 3 folds and a geometric mean titer of 806 detected in samples taken before the third dose (95% CI, 2575-252; titers range 80-5120; P = .02) (Figure 1A). To further assess whether the antibodies elicited by mRNA-1273 vaccination are capable of blocking the ACE2/RBD interaction, thus inhibiting the entrance mechanism of SARS-CoV-2 into human cells, plasma samples were tested using a SARS-CoV-2 surrogate virus neutralization test (cPass, Genscript). As shown in Figure 1B, the ACE2/RBD binding inhibition significantly increases after the third dose (84.1% ± 10.5% at day 187 vs 6.7% ± 3.4% at day 180; P = .01 with Wilcoxon test for paired samples). The only exception is patient #184, possibly due to chronic GVHD and the relative pharmacological therapy, including inhibitor of Bruton tyrosine kinase, that might have influenced the development of neutralizing antibodies, hampering germinal center reaction and B-cell maturation (as also suggested by Yi-Chou Hou and colleagues discussing the efficacy of COVID-19 vaccines in kidney transplanted patients).9
Immune response induced by the third dose of mRNA-1273 vaccine. Spike-specific IgG analyzed by ELISA in plasma collected 0, 28, 90, 180, and 187 days after the first dose of the mRNA-1273 vaccine (arrows) in each of the 9 low responder HCT recipients. Single HCT recipients were identified with a number and a color, as reported. Spike-specific IgG titers are expressed as fold increase compared with baseline (A). Surrogate virus neutralization test was performed before (day 180) and after (day 187) the third mRNA-1273 vaccine dose. Data are reported as ACE2/RBD binding inhibition percentage for each subject. A threshold (dotted line) was placed at 30% inhibition percentage to discriminate between positive and negative samples, according to the instructions of the manufacturer (B). Spike-specific B-cell response following mRNA-1273 vaccination. Percentages of RBD+Spike+ B cells among CD19+ cells were assessed in each subject immediately before (day 180) and after (day 187) the third dose (C). Statistical significance in (B) and (C) was assessed with the Wilcoxon test for paired samples. Bivariate analysis of the spike-specific IgG and RBD+Spike+ B cells. A linear model is fitted on the data (straight line), and 95% CI is reported (dashed lines); the correlation was performed with Spearman’s method (D).
Immune response induced by the third dose of mRNA-1273 vaccine. Spike-specific IgG analyzed by ELISA in plasma collected 0, 28, 90, 180, and 187 days after the first dose of the mRNA-1273 vaccine (arrows) in each of the 9 low responder HCT recipients. Single HCT recipients were identified with a number and a color, as reported. Spike-specific IgG titers are expressed as fold increase compared with baseline (A). Surrogate virus neutralization test was performed before (day 180) and after (day 187) the third mRNA-1273 vaccine dose. Data are reported as ACE2/RBD binding inhibition percentage for each subject. A threshold (dotted line) was placed at 30% inhibition percentage to discriminate between positive and negative samples, according to the instructions of the manufacturer (B). Spike-specific B-cell response following mRNA-1273 vaccination. Percentages of RBD+Spike+ B cells among CD19+ cells were assessed in each subject immediately before (day 180) and after (day 187) the third dose (C). Statistical significance in (B) and (C) was assessed with the Wilcoxon test for paired samples. Bivariate analysis of the spike-specific IgG and RBD+Spike+ B cells. A linear model is fitted on the data (straight line), and 95% CI is reported (dashed lines); the correlation was performed with Spearman’s method (D).
The RBD-specific B cells, identified as RBD and spike double-positive among CD19+ cells, have been characterized by flow cytometry. The third dose induces a slight increase of the RBD+Spike+ B-cell frequency from 0.11% ± 0.03% (of CD19+ cells; P = .05 with Wilcoxon test for paired samples) at day 180% to 0.43% ± 0.17% at day 187 (Figure 1C). Bivariate analysis shows a significant positive correlation between RBD+Spike+ B cells before the third dose (day 180) and spike-specific IgG 7 days after the third dose (Spearman’s correlation with r = 0.68; P = .04) (Figure 1D), suggesting RBD+Spike+ B cells are a critical biomarker for predicting the humoral response to repeated vaccine doses.10 Further studies will be necessary to monitor the permanence of the vaccine-induced immune response with particular attention to immune memory.
Our findings provide evidence that a third dose of mRNA-1273 vaccine considerably enhances SARS-CoV-2-specific antibody and B-cell response in low responder HCT recipients, highlighting the importance of an additional vaccine dose for those who may have achieved a limited response to the primary series of the COVID-19 vaccination. Therefore, a third vaccine dose capable of effectively boosting the immune system is particularly critical for low responders who could have a weakened and/or slowed immune priming.6 Our data also highlight that there may be patients that, due to prolonged pharmacological immunosuppression, develop a limited response also to the third dose, and they have to be protected by vaccinating the households and close contacts.
Taken together, these data are of critical importance to guide SARS-CoV-2 vaccination strategies and policies in HCT patients.
Acknowledgment: This study was supported by the Department of Medical Biotechnologies of the University of Siena (D.M.)
Contribution: A.C., G.P., F.M., E.P., and D.M. conceived and designed the study; G.P., A.B., M.T., G.M., and F.M. enrolled patients; E.P., J.P., and F.F. processed the samples; E.P., G.P., F.F., and J.P. carried out immunological analysis; E.P., A.C., J.P., S.L., A.B., and D.M. analyzed and interpreted data; E.P., A.C., A.B., and D.M. wrote the manuscript; D.M. provided financial support; and all authors have read and approved the final version of the manuscript.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Donata Medaglini, Laboratory of Molecular Microbiology and Biotechnology, Department of Medical Biotechnologies, University of Siena, 53100 Siena, Italy; e-mail: donata.medaglini@unisi.it.
References
Author notes
For data sharing, contact the corresponding author: donata.medaglini@unisi.it.