Key Points
An unacceptably high 30% of the POEMS population has ≥1 thrombotic event, more commonly during the active phase of disease.
Arterial thromboses are more common than venous ones, necessitating a proactive management strategy.
Abstract
Arterial and venous thromboses occur in patients with POEMS (polyneuropathy, organomegaly, endocrinopathy, M-protein level, and skin changes) syndrome at a previously reported rate of 20%. We reviewed the University College London Hospitals (UCLH) POEMS Registry to determine the rate of venous thromboembolism (VTE), arterial events, and risk factors. This registry, established in 1999 and comprising 103 patients at the time of this study, is the largest single-center cohort in Europe. Of the 83 assessable patients, median age at presentation was 52 years (range, 31-84). Twenty-five patients experienced clinically apparent arterial or venous events, and 2 had concurrent arterial and venous thromboses. Eleven patients had VTEs, including deep vein thrombosis (DVT; 3 of 11), pulmonary embolism (4 of 11), and peripherally inserted central catheter–associated DVT, which occurred during autologous stem cell transplantation (3 of 11). Sixteen patients experienced arterial events: stroke (7 of 16), peripheral arterial occlusion (5 of 16), myocardial infarction (3 of 16), and microvascular disease (1 of 16), with no discernible relationship with thrombocytosis or polycythemia. Thirty percent of POEMS patients have arterial and venous thromboses, higher than previously reported. There were more arterial than venous events, and most occurred during active disease, before the start of chemotherapy, indicating the need for a preemptive approach to thromboprophylaxis.
Introduction
POEMS syndrome (an acronym for polyneuropathy, organomegaly, endocrinopathy, M-protein level, and skin changes) is a paraneoplastic phenomenon resulting from an underlying plasma cell neoplasm. Not all 5 features must be present to make the diagnosis, and there is a range of other features not captured in the acronym, including a tendency toward JAK2− myeloproliferation manifested by polycythemia/thrombocytosis during the phase of active disease.1 The exact incidence and prevalence are unknown.2 Disease activity largely correlates with vascular endothelial growth factor (VEGF) levels in the blood.3
Arterial and venous thromboses have been reported in up to 20% of POEMS patients in small studies and case reports.1 Arterial events occurred in 4 patients with POEMS syndrome in a cohort of 20.4 A retrospective observational study evaluated potential predictors of stroke in patients with POEMS syndrome and found an elevated platelet count; bone marrow plasmacytosis increased the risk of cerebral infarction.5
One study investigating coagulation abnormalities in 4 patients with POEMS syndrome identified increased markers of coagulation activation such as fibrinogen, fibrinopeptide A, and thrombin-antithrombin complexes during the active phase of disease.6
Treatment of POEMS is based on suppressing or ablating the underlying plasma cell neoplasm with treatment regimens adapted from the treatment of myeloma,1 in which there is a known risk of thrombosis associated with the use of steroids in combination with immunomodulatory (IMiD) drugs, such as thalidomide7 and lenalidomide.8 The UK Myeloma XI Chemotherapy trial reported the VTE rate in myeloma patients receiving IMiD-based chemotherapy to be 12%,9 indicating a lower risk than reported in POEMS syndrome. The guidelines for ambulatory patients with myeloma receiving prothrombotic agents comprise prophylactic low molecular weight heparin (pLMWH) or aspirin, taking account of patient, disease, and treatment-related risk factors.10,11 There is no such guideline for the treatment of POEMS patients despite the adoption of similar regimens on a background of superimposed immobility.
The University College London Hospitals (UCLH) POEMS Registry, established in 1999, is, de facto, the United Kingdom’s only and Europe’s largest single-center POEMS registry. It includes all patients referred to UCLH, a tertiary referral center where a joint-care, multidisciplinary approach to the management of POEMS patients includes peripheral nerve, hematology, and endocrinology specialists.
This retrospective observational cohort study was instigated after the observation of a significant number of clinically relevant vaso-occlusive events and in the absence of a coherent thromboprophylaxis (TP) strategy. This report is the first taken from registry data and focusing on arterial and venous thrombosis, in this field.
Methods
Patient characteristics and thrombosis risk factors were recorded. Biomarkers, including blood counts and serial serum VEGF levels, were collected and analyzed according to arterial or venous thrombotic event. Treatment of POEMS and TP prescriptions were reviewed.
All clinically apparent arterial and venous thromboses occurring after the onset of POEMS symptoms were reviewed. Particular note was made of the timing of thrombotic events with respect to disease activity (defined by the most recent serum VEGF), POEMS treatment, and TP in use around the time of the event.
Active disease was defined as a serum VEGF of >1000 pg/mL based on a deeply phenotyped cohort with pre- and posttreatment samples and univariate and multivariate statistical analyses that found 1000 pg/mL with a λ light chain and an appropriate neuropathy with almost 100% sensitivity to detect at diagnosis.3
Results and discussion
Of the 103 patients in the registry, 20 were excluded because of insufficient accessible data from referral centers regarding initial diagnosis (supplemental Figure 1). The baseline characteristics of the 83 included patients are described in Table 1. Median follow-up was 70 months (range, 2-282).
Radiotherapy was a treatment modality in 21 of 83 (25%), and 48 of 83 (52%) underwent autologous stem cell transplantation at some time in their treatment. Fifty-one outpatient-based chemotherapy regimens were prescribed. Lenalidomide-dexamethasone (LD) was most frequent (30 of 51), followed by cyclophosphamide-dexamethasone (CD; 10 of 51), cyclophosphamide-LD (3 of 51), melphalan-steroids (3 of 51), CD-thalidomide (2 of 51), ixazomib-LD (1 of 51), bortezomib-thalidomide-dexamethasone (1 of 51), and carfilzomib-dexamethasone (1 of 51).
Thirty patients received TP while undergoing treatment of POEMS. Prophylactic LMWH accounted for 17 of 30 prescriptions; 11 were for an IMiD-containing regimen. Other agents prescribed include aspirin (75 mg once daily; 6 of 30), treatment-dose LMWH (2 of 30), rivaroxaban (2 of 30), warfarin (2 of 30), and clopidogrel (1 of 30).
Arterial-only events occurred in 14 patients, venous-only events in 9, and arterial and venous thromboses in 2. Three patients had a prior history of VTE and developed a further thrombosis: 1 with a history of deep vein thrombosis (DVT) developed pulmonary emboli (PE), and 2 with a VTE history had arterial events.
Venous events included 4 DVTs, 3 PEs, 3 peripherally inserted central catheter-associated DVTs occurring during melphalan-based autologous stem cell transplantation and 1 portal vein thrombosis. Five patients had events while receiving chemotherapy (3 were prescribed pLMWH, and 2 treatments were unknown), the other 6 patients had not received TP. Most VTEs occurred during active disease with a median baseline serum VEGF level of 2560 pg/mL (range, 323-6845 pg/mL), platelets 436 × 109/L (range, 194-541 × 109/L), and hemoglobin 150 g/L (range, 137-156 g/L).
Sixteen patients experienced arterial events including stroke (7 of 16), peripheral arterial occlusion (5 of 16), myocardial infarction (3 of 16), and microvascular disease (1 of 16). Most events occurred during active disease with a median baseline serum VEGF level of 3890 pg/mL (range, 1 010-11 650 pg/mL). No arterial events occurred with a baseline VEGF <1000 pg/mL. Median platelet count was 366 × 109/L (range, 201-694 × 109/L), and hemoglobin 125 g/L (range, 89-160 g/L). Three arterial events occurred while the patients were receiving treatment for POEMS: 1 patient developed an arterial stroke during LD treatment and LMWH prophylaxis; 1 patient receiving LD and prophylactic rivaroxaban 10 mg developed a peripheral arterial occlusion, and another patient receiving melphalan-prednisolone and warfarin for atrial fibrillation (international normalized ratio range, 2.0-3.0) developed peripheral arterial occlusion. No events occurred on antiplatelet TP, as none was prescribed in those that experienced an arterial event.
Twenty-three events (16 arterial and 7 venous) occurred during active disease, from presentation and before commencement of treatment, in contrast to the myeloma cohort where treatment-related risk factors play an important role in the risk of thrombosis.7,8 Seven events (1 arterial and 6 venous) occurred during treatment of POEMS.
Thirty percent of the POEMS cohort experienced arterial and/or venous thrombotic event and the associated morbidity, which is unacceptably high. There were more arterial than venous events, and the highest risk period appeared to be during active disease, before treatment began, with an increase in baseline serum VEGF, indicating the importance of disease activity. As new events also occurred during the treatment phase, the risk of thrombosis was not immediately abrogated by the initiation of treatment, but took time to subside.
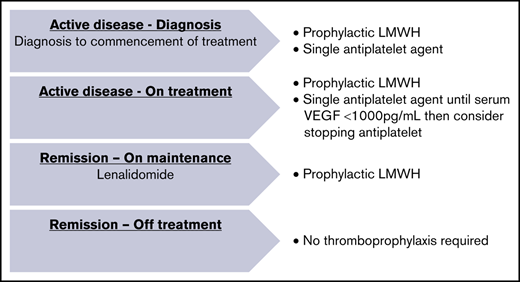
A pragmatic approach to risk reduction is necessary, given the lack of randomized controlled trials in this rare disease. Figure 1 illustrates the primary thromboprophylactic regimen implemented at UCLH to reduce risk of arterial and venous thromboses in POEMS patients. Before commencement of TP, a full assessment of additional bleeding risk, including falls and risk of thrombosis, such as immobility and previous VTE, should be undertaken.
After presentation and during commencement of treatment, pLMWH and a low-dose antiplatelet agent are prescribed concurrently and continued until the serum VEGF falls below 1000 pg/mL, at which point the antiplatelet agent is discontinued unless there are ongoing risk factors, because of all arterial events occurring with a baseline serum VEGF >1000 pg/mL.
Prophylactic LMWH continues while the patient is on maintenance treatment with prothrombotic agents such as lenalidomide. When in remission, with suppressed VEGF levels and chemotherapy discontinued, notwithstanding ability to ambulate, all TP can be stopped. This guidance is being prospectively audited to determine efficacy and ensure patient safety.
Original data are available by e-mail request to the corresponding author.
Acknowledgments
This work was supported by an ABN/Guarantors of Brain Clinical Training Research Fellowship (S.K.) and the National Institute for Health Research, University College London Hospitals, Biomedical Research Centre (M.P.L.).
Authorship
Contribution: Z.S. and A.W. collected data and wrote the paper; S.K. provided data collected from the POEMS registry; M.P.L. and S.D. run the clinical POEMS service; and all authors reviewed the manuscript and created the primary thromboprophylactic strategy being implemented.
Conflict-of-interest disclosure: The authors declare no competing financial interests.
Correspondence: Zara Sayar, Haemostasis Research Unit, Department of Haematology, University College London, 1st Floor, 51 Chenies Mews, London WC1E 6HX, United Kingdom; e-mail: zara.sayar@nhs.net.
References
Author notes
The full-text version of this article contains a data supplement.