Abstract
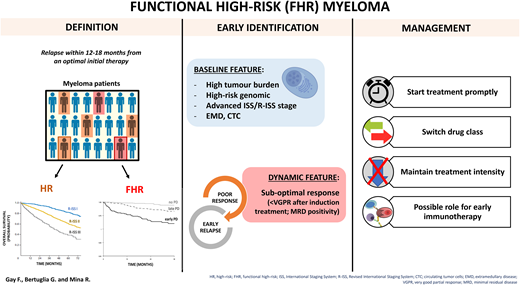
Multiple myeloma is a clinically and biologically highly heterogeneous disease, as the overall survival can vary from more than a decade in patients with standard risk disease treated with intensive chemotherapy to 2−3 years in patients with high-risk features. The current staging systems, which rely on baseline biological risk factors to stratify patients into groups with differing risks of progression or death, are sometimes suboptimal tools for identifying high-risk patients. This is particularly evident when considering the so-called functional high-risk patients—patients who do not necessarily display baseline high-risk features but typically show a suboptimal response to induction therapy or relapse early after treatment initiation: the survival of these patients is particularly poor even in the context of newer therapies. The prompt identification, as well as a consistent definition, of this subset of patients, as well as their management, currently represents an unmet medical need. In this review we explore the main characteristics of functional high-risk patients, the available known risk factors and scoring systems, and the possible management.
Learning Objectives
Identify the patients with functional high-risk multiple myeloma
Outline a possible therapeutic strategy for patients with functional high-risk multiple myeloma
Define possible risk factors of suboptimal response and early relapse
CLINICAL CASE
A 58-year-old man with newly diagnosed (ND), International Staging System (ISS) stage I, Revised ISS (R-ISS) stage II IgG-κ multiple myeloma (MM) was referred to our center. The patient was symptomatic for bone lesions (L3 vertebral fracture) and presented a paraskeletal plasmacytoma involving the right and left pedicles on magnetic resonance imaging. The bone marrow biopsy showed 30% plasma cell infiltration, and fluorescent in situ hybridization (FISH) analysis on bone marrow aspirate was negative for del(17p), t(4;14), t(14;16), and chromosome 1 abnormalities. The patient had no comorbidities and an Eastern Cooperative Oncology Group (ECOG) performance status (PS) of 1, related to the bone disease.
The patient started treatment with 4 cycles of daratumumab, bortezomib, thalidomide, and dexamethasone (DVTd), achieving a partial response (PR) after the first cycle, with no significant decrease in the monoclonal (M) component during the subsequent cycles. After the induction phase, the patient underwent stem cell mobilization and collection and high-dose melphalan and autologous stem cell transplantation (HDM-ASCT), without a further decrease in the M-component. Two months after ASCT, a sudden increase of the M-component was observed along with the onset of hypercalcemia. The FISH analysis carried out on bone marrow plasma cells at relapse showed the acquisition of del(17p). A second- line treatment with carfilzomib, lenalidomide, and dexamethasone (KRd) was started. The patient achieved a very good partial response (VGPR), which is currently ongoing 24 months after treatment initiation.
How do we define high risk in MM?
The prognosis of MM has greatly improved in the last 2 decades as a result of the introduction of new agents, their combinations into multidrug regimens, and the use of HDM-ASCT. However, the biological and clinical diversity of MM reflects its heterogeneous clinical courses and prognosis; therefore, the overall survival (OS) of a NDMM patient ranges from 2 to 3 years in the presence of high-risk features to more than 10 years in standard-risk disease.1
Several biological and clinical risk factors correlate with an aggressive disease, and risk models have been developed to predict the risk of relapse or death. High serum values of β2- microglobulin (B2M), a marker of tumor burden and renal insufficiency; high lactate dehydrogenase (LDH) serum values linked to plasma cell proliferation; and low albumin values, reflecting systemic inflammation, are validated risk factors that correlate with disease aggressiveness.2
Recurrent chromosomal abnormalities detected by FISH, including t(4;14), t(14;16), and del(17p), are detected in up to 15% to 20% of MM patients at diagnosis, and their presence is associated with shorter progression-free survival (PFS) and OS.2 Copy number alterations involving the long arm of chromosome 1 (1q), detected in up to 30% of patients at diagnosis, portend a worse survival.3 Del(1p32) is another adverse feature.4 The number of high-risk chromosomal abnormalities, or the co-occurrence of mutations such as TP53 inactivation,5 are additional prognostic factors, as patients with so-called double-hit or ultra-high-risk myeloma (two or more high-risk genetic lesions) consistently showed worse survival outcomes compared to those with 1 or no high-risk genetic alteration.6-8 In addition to cytogenetics, different gene expression profile (GEP) signatures have been demonstrated to be independent prognostic factors for both PFS and OS, thus providing an additional method to identify high risk.9-12 The spread of myeloma cells outside the bone marrow is another unfavorable prognostic factor. The presence of extramedullary plasmacytomas is an established risk factor for both PFS and OS.13 Several groups have demonstrated that circulating tumor cells (CTCs),14,15 even when the criteria for plasma-cell leukemia are not fulfilled, correlate with shorter survival. Furthermore, MM with plasma-cell leukemia– like status, identified by transcriptome profile, exhibits an aggressive disease course.16
The current risk-stratification model recommended by the International Myeloma Working Group, the R-ISS,17 stratifies patients into 3 risk groups with a different OS (stage I: not reached [NR]; stage II: 83 months; and stage III: 43 months); although the majority of patients (62%) fall into the intermediate- risk category. To account for this issue, while also including chromosome 1q alterations, the European Myeloma Network has recently proposed a second revision of the R-ISS (R2-ISS) that stratifies patients into 4 risk categories, with a more homogeneous repartition (Table 1).18
Risk factors and stratification models in patients with multiple myeloma
| ISS59 . | R-ISS17 . | R2-ISS18 . | Other risk factors . |
|---|---|---|---|
| Stage I: serum β2M < 3.5 µg/L and serum albumin ≥3.5 g/dL Stage II: not ISS stage I or III Stage III: serum β2M ≥ 5.5 µg/L | Stage I: ISS stage I, t(4;14), and/or t(14;16) and/or del(17p) negativity by FISH and normal serum LDH Stage II: not ISS stage I or III Stage III: ISS stage III and either elevated serum LDH or t(4;14) and/or t(14;16) and/or del(17p) positivity by FISH | Additive score: ISS II: 1 point ISS III: 1.5 points Del(17p): 1 point Elevated serum LDH: 1 point t(4;14): 1 point 1q+: 0.5 point Groups: Low risk: 0 Low intermediate: 0.5-1 Intermediate-high: 1.5-2.5 High: 3-5 | Genetic lesions: deletion and mutations of TP535 ; deletion chromosome 1p detected by FISH4 Extramedullary disease60 CTCs detected in the peripheral blood by flow cytometry14,15 Plasma cell leukemia and plasma cell leukemia–like disease16,61 GEP: high-risk signatures9-12 |
| ISS59 . | R-ISS17 . | R2-ISS18 . | Other risk factors . |
|---|---|---|---|
| Stage I: serum β2M < 3.5 µg/L and serum albumin ≥3.5 g/dL Stage II: not ISS stage I or III Stage III: serum β2M ≥ 5.5 µg/L | Stage I: ISS stage I, t(4;14), and/or t(14;16) and/or del(17p) negativity by FISH and normal serum LDH Stage II: not ISS stage I or III Stage III: ISS stage III and either elevated serum LDH or t(4;14) and/or t(14;16) and/or del(17p) positivity by FISH | Additive score: ISS II: 1 point ISS III: 1.5 points Del(17p): 1 point Elevated serum LDH: 1 point t(4;14): 1 point 1q+: 0.5 point Groups: Low risk: 0 Low intermediate: 0.5-1 Intermediate-high: 1.5-2.5 High: 3-5 | Genetic lesions: deletion and mutations of TP535 ; deletion chromosome 1p detected by FISH4 Extramedullary disease60 CTCs detected in the peripheral blood by flow cytometry14,15 Plasma cell leukemia and plasma cell leukemia–like disease16,61 GEP: high-risk signatures9-12 |
What is functional high risk?
Despite the improvement in baseline risk-stratification, a significant proportion of patients not classified as high-risk at diagnosis will progress within 12 to 18 months from treatment initiation despite an optimal initial therapy: these are considered functional high-risk (FHR) patients.19,20 Studies focusing on early relapse and associated risk features are heterogeneous. They include transplant-eligible and non-eligible patients, treated up front with immunomodulatory agents (IMiDs) and proteasome inhibitors (PIs) in most cases, while data in patients treated up front with anti-CD38 monoclonal antibodies (MoAbs) are so far lacking. Early relapse is commonly defined as occurring within 12 to 18 months from initial treatment,21,22 24 months in a few previous reports.23,24 Patients experiencing early relapse will display a short OS, ranging from 18 to 32 to 44 months (Table 2).
Studies evaluating functional high risk
| Reference . | Study population, N . | ER or FHR definition . | ER, N (%) . | First-line treatment, N (%) . | Median OS (early vs late relapse) . | Factors influencing ER . | ||
|---|---|---|---|---|---|---|---|---|
| Baseline factors . | Treatment related . | Impact of response . | ||||||
| Jimenez-Zepeda et al 201540 | Princess Margaret Cancer Center, N = 184 | ER: progressive disease within 12 months from transplant | 27 (14) | In overall population: • PI based: 119 (64.7) • IMiD based: 65 (35.3) • ASCT: 184 (100) | 20 mo vs 93 mo (P = . 001) | Favoring • Thalidomide induction regimens (P = .04) | Patients with ER showed a lower ≥ VGPR rate that those with non-ER | |
| Kumar et al 201823 | Center for International Blood and Marrow Transplant Research database, N = 3256 | ER: progressive disease within 24 months from transplant | 1239 (38) | In overall population: • Bort based: 748 (22) • Len based: 342 (10) • Len-Bort based: 545 (17) • ASCT: 3256 (100) | 44.7 mo vs 113.7 mo (P < .001) | Favoring: • DS/ISS III (P = .02) Protective: • Chemo sensitivity (P = .007) | Protective: • Transplant after 2008 (P = .02) • Post-ASCT maintenance with novel agent (P = .02) | |
| Spencer et al 201921 | Australian and New Zealand Myeloma and Related Diseases Registry, N = 1320 | FHR: ER + SOR ER: progressive disease within 12 months of commencing 1st line of therapy SOR: best response to 1st line minimal response or stable disease | FHR: 270 (20.4) ER: 118 (8.9) SOE: 152 (11.5) | N/A | ER, 20.2 mo vs 60.7 mo (P < .001) SOR, 57.8 mo vs 59.3 mo | ER, favoring: • Higher ISS (P < .001); • Higher R-ISS (P < .001); • Inferior ECOG (P = .007); • Hypercalcemia (P = .002); • Renal insufficiency (P < .001); • Anemia (P < .001) SOR, favoring: • Age >70 y (P = .01) | SOR, favoring: • Bort based (P = .001) | SOR (MR or SD) in early vs late relapse: 25% vs 11% (P < .001) |
| Kastritis et al 202024 | Department of Clinical Therapeutics, Athens (Greece), N = 297 | ER: progressive disease within 12 months from transplant | 43 (14.5) | In overall population: • Bort based: 139 (47) • Len based: 248 (6) • Bort + IMiD: 26 (9) ASCT: 297 (100) | mOS 18 mo (early relapse) vs 5-years OS 71% (late relapse) | Favoring: • LDH ≥ ULN (P = .018) • Hypercalcemia (P = .034) | Protective: • Consolidation therapy (P < .001) • Maintenance (P < .048) | Response rates and depth of response to induction therapy were not significantly different among those with early vs later relapse |
| Corre et al 202033 | Retrospective study, N = 2627 patients | ER: progressive disease within 18 months from initial therapy or within 12 months from transplant | 496 (18.9) | In overall population: • PI based: 1129 (43) • PI + IMiD: 1485 (57) ASCT: 2627 (100) | HR 4.40 (P < .0001) | Favoring: • ISS II/III (P < .001) • High-risk cytogenetics, including del(17p) or t(4;14) or gain 1q or del(1q32) (P < .001) Protective: • Trisomy 5 (P = .0024) | • Poor response to treatment (<VGPR) (P < .001) | |
| D'Agostino et al 202035 | CoMMpass data set, N = 926 | ER: progressive disease within 18 months from diagnosis | 191 (20.6) | In overall population • Bort based: 83 (9) • Len based: 63 (7) • Bort + Len based: 319 (34) • Carf based: 215 (23) ASCT: 440 (53) | 32.8 mo vs 54 mo (ISS III) vs 65 mo (cytogenetics high risk) | Favoring: • TP53 mutation (P < .001) • High LDH (P = .006) • L-chain translocation (P = .033) • IGLL5 mutation (P = .007) | Favoring: • Refractoriness to PIs (P < .001) or IMiDs + PIs (P < .001) Protective: • Carfilzomib-based induction (P = .01) | • Lower ORR (P < .001; • Poor response to treatment (<VGPR) (P < .001) |
| Bygrave et al 202122 | NCRI Myeloma XI, N = 1349 | ER: progressive disease within 12 months from transplant | 174 (12.9) | CTd vs CRd as induction treatment If ≤ VGPR prior ASCT: VTd ASCT = 1349 (100) | 26 mo vs 91 mo (P < .001) | Favoring: • Anemia (P < .0001) • Low platelet count (P = .0001) • Heavy plasma cell infiltration (P < .0001) • Advanced ISS stage (P = .0029) • High-risk genetic (P < .0001) | Protective: Len-based maintenance (P = .0005) | |
| Soekojo et al 202236 | CoMMpass data set, N = 512 | FHR: primary refractory to induction therapy plus progressive disease within early relapse within 12 months of starting induction therapy without high-risk cytogenetics (ER) | FHR: 61 (11) | In FHR population: • PI based: 43 (36) • IMiD based: 18 (15) • PI + IMiD: 50 (42.7) ASCT = N/A | 27.6 mo (FHR) vs 44.7 mo (GHR) vs NR (SR) (P < .001) | Favoring: mutations affecting the IL- 6/Jak/STAT3 pathway, associated with aberrant mitosis and DNA damage response | ||
| Reference . | Study population, N . | ER or FHR definition . | ER, N (%) . | First-line treatment, N (%) . | Median OS (early vs late relapse) . | Factors influencing ER . | ||
|---|---|---|---|---|---|---|---|---|
| Baseline factors . | Treatment related . | Impact of response . | ||||||
| Jimenez-Zepeda et al 201540 | Princess Margaret Cancer Center, N = 184 | ER: progressive disease within 12 months from transplant | 27 (14) | In overall population: • PI based: 119 (64.7) • IMiD based: 65 (35.3) • ASCT: 184 (100) | 20 mo vs 93 mo (P = . 001) | Favoring • Thalidomide induction regimens (P = .04) | Patients with ER showed a lower ≥ VGPR rate that those with non-ER | |
| Kumar et al 201823 | Center for International Blood and Marrow Transplant Research database, N = 3256 | ER: progressive disease within 24 months from transplant | 1239 (38) | In overall population: • Bort based: 748 (22) • Len based: 342 (10) • Len-Bort based: 545 (17) • ASCT: 3256 (100) | 44.7 mo vs 113.7 mo (P < .001) | Favoring: • DS/ISS III (P = .02) Protective: • Chemo sensitivity (P = .007) | Protective: • Transplant after 2008 (P = .02) • Post-ASCT maintenance with novel agent (P = .02) | |
| Spencer et al 201921 | Australian and New Zealand Myeloma and Related Diseases Registry, N = 1320 | FHR: ER + SOR ER: progressive disease within 12 months of commencing 1st line of therapy SOR: best response to 1st line minimal response or stable disease | FHR: 270 (20.4) ER: 118 (8.9) SOE: 152 (11.5) | N/A | ER, 20.2 mo vs 60.7 mo (P < .001) SOR, 57.8 mo vs 59.3 mo | ER, favoring: • Higher ISS (P < .001); • Higher R-ISS (P < .001); • Inferior ECOG (P = .007); • Hypercalcemia (P = .002); • Renal insufficiency (P < .001); • Anemia (P < .001) SOR, favoring: • Age >70 y (P = .01) | SOR, favoring: • Bort based (P = .001) | SOR (MR or SD) in early vs late relapse: 25% vs 11% (P < .001) |
| Kastritis et al 202024 | Department of Clinical Therapeutics, Athens (Greece), N = 297 | ER: progressive disease within 12 months from transplant | 43 (14.5) | In overall population: • Bort based: 139 (47) • Len based: 248 (6) • Bort + IMiD: 26 (9) ASCT: 297 (100) | mOS 18 mo (early relapse) vs 5-years OS 71% (late relapse) | Favoring: • LDH ≥ ULN (P = .018) • Hypercalcemia (P = .034) | Protective: • Consolidation therapy (P < .001) • Maintenance (P < .048) | Response rates and depth of response to induction therapy were not significantly different among those with early vs later relapse |
| Corre et al 202033 | Retrospective study, N = 2627 patients | ER: progressive disease within 18 months from initial therapy or within 12 months from transplant | 496 (18.9) | In overall population: • PI based: 1129 (43) • PI + IMiD: 1485 (57) ASCT: 2627 (100) | HR 4.40 (P < .0001) | Favoring: • ISS II/III (P < .001) • High-risk cytogenetics, including del(17p) or t(4;14) or gain 1q or del(1q32) (P < .001) Protective: • Trisomy 5 (P = .0024) | • Poor response to treatment (<VGPR) (P < .001) | |
| D'Agostino et al 202035 | CoMMpass data set, N = 926 | ER: progressive disease within 18 months from diagnosis | 191 (20.6) | In overall population • Bort based: 83 (9) • Len based: 63 (7) • Bort + Len based: 319 (34) • Carf based: 215 (23) ASCT: 440 (53) | 32.8 mo vs 54 mo (ISS III) vs 65 mo (cytogenetics high risk) | Favoring: • TP53 mutation (P < .001) • High LDH (P = .006) • L-chain translocation (P = .033) • IGLL5 mutation (P = .007) | Favoring: • Refractoriness to PIs (P < .001) or IMiDs + PIs (P < .001) Protective: • Carfilzomib-based induction (P = .01) | • Lower ORR (P < .001; • Poor response to treatment (<VGPR) (P < .001) |
| Bygrave et al 202122 | NCRI Myeloma XI, N = 1349 | ER: progressive disease within 12 months from transplant | 174 (12.9) | CTd vs CRd as induction treatment If ≤ VGPR prior ASCT: VTd ASCT = 1349 (100) | 26 mo vs 91 mo (P < .001) | Favoring: • Anemia (P < .0001) • Low platelet count (P = .0001) • Heavy plasma cell infiltration (P < .0001) • Advanced ISS stage (P = .0029) • High-risk genetic (P < .0001) | Protective: Len-based maintenance (P = .0005) | |
| Soekojo et al 202236 | CoMMpass data set, N = 512 | FHR: primary refractory to induction therapy plus progressive disease within early relapse within 12 months of starting induction therapy without high-risk cytogenetics (ER) | FHR: 61 (11) | In FHR population: • PI based: 43 (36) • IMiD based: 18 (15) • PI + IMiD: 50 (42.7) ASCT = N/A | 27.6 mo (FHR) vs 44.7 mo (GHR) vs NR (SR) (P < .001) | Favoring: mutations affecting the IL- 6/Jak/STAT3 pathway, associated with aberrant mitosis and DNA damage response | ||
Bort, bortezomib; Carf, carfilzomib; CTd, cyclophosphamide-thalidomide-dexamethasone; ER, early relapse; GHR, genomic high risk; IL-6, interleukin 6; Len, lenalidomide; mOS, median overall survival; MR, minimal response; N/A, not available; NCRI, National Cancer Research Institute; ORR, overall response rate; SOR, suboptimal response; SR, standard risk; STAT3, signal transducer and activator of transcription 3; ULN, upper limit of normal; VTd, bortezomib-thalidomide-dexamethasone.
Currently approved regimens incorporating up-front anti-CD38 MoAbs have significantly reduced the risk of early relapse at 12 to 24 months to approximately less than 10% in transplant-eligible and 20% in non–transplant-eligible patients compared to older regimens.25-27 Given these positive results, the design of specific clinical trials for these high-risk populations has become more challenging. The case presentation described a patient with FHR MM: despite the lack of a baseline high-risk feature, the disease relapsed early (12 months since initial diagnosis), thus indicating an aggressive clinical course.
How can we identify early FHR?
Several groups have made the effort to define risk factors for an early relapse and to incorporate them into a scoring system (Tables 2 and 3).28-32 Markers of high tumor burden and organ damage (anemia, thrombocytopenia, high plasma cell infiltration, hypercalcemia, renal insufficiency, high LDH),21,22,24 advanced myeloma stage (Durie and Salmon stage III,23 ISS stage III,21-23,33 R-ISS stage III21,34 ), and high-risk cytogenetic features are frequently observed in patients experiencing early relapse.22,33,35 Nevertheless, a proportion of “standard-risk” patients relapse early. As an example, ISS-I was reported in 22% of early-relapse patients and standard-risk cytogenetic in 12% to 28%.22,33 Studies are heterogeneous in terms of baseline features analyzed, and only the most recent reported a more comprehensive evaluation including R-ISS, extended cytogenetic evaluation (1q and 1p abnormalities), and mutational status (p53, IGLL5 mutation, interleukin 6/JaK/STAT3 pathway).35,36 Indeed, as both GEP and the presence of CTCs have been shown to complement and refine the prognostic information provided by commonly evaluated risk factors, the lack of access to such tools in the community setting limits our ability to properly identify high-risk patients at diagnosis.14,15,37,38 Their integrations in clinical practice could allow a more precise identification of patients at high risk of early relapse, although some patients with FHR will likely be identified only due to disease evolution. However, whether an early relapse is due to a treatment-induced clonal selection that leads to the early emergence of a highly resistant MM clone or simply to an inadequate risk evaluation at baseline remains to be determined.
Studies evaluating scoring systems to identify the risk of early relapse
| Score . | Variables . | Risk groups (sum) . | Clinical outcomes . |
|---|---|---|---|
| CIBMTR scoring system28 | • High-risk cytogeneticsa: +4 points • Pre-ASCT BMPCs ≥10%: +4 points • Albumin at diagnosis ≤3,5 g/dL: +2 points • Standard-risk cytogenetic: +1 point • No cytogenetic abnormality, BMPCs <10% at ASCT, and albumin ≥3.5 g/dL at diagnosis: +0 point | • Low risk (0-3) • Intermediate risk (4-8) • High risk (9-10) | 3-year PFS: 58% vs 49% vs 31% (P < .001) 3-year OS: 88% vs 81% vs 64% (P < .001) |
| S-ERMM(18) score29 | • LDH > ULN: +5 points • Presence of t(4;14): +5 points • Presence of del(17p): +3 points • Abnormal albumin: +3 points • BMPCs >60%: +3 points • FLC λ: +2 points | • Low risk (≤5) • Intermediate risk (6-10) • High risk (≥11) | Median OS: NR vs 59.5 mo vs 31.5 mo (P < .001) Median PFS2: 62.3 mo vs 40 vs 19.8 mo (P < .001) |
| DS-ERMM score29 | • S-ERMM score (0-21 points) • Achievement of at least VGPR: −4 points | • Low risk (≤0) • Intermediate risk (1-5) • High risk (≥6) | Median OS: NR vs NR vs 57.3 mo (P < .001) Median PFS2: NR vs 53.8 mo vs 40.2 mo (P < .001) |
| EBMT scoring system30 | • Disease status at ASCT: 0-3 points CR/VGPR: +0 point PR/SD/MR: +1 point Rel/prog: +3 points • ISS: ISS I: +0 point ISS II: +1 point ISS III: +2 points • Age (years): −1 to −3 points ≤55: −1 point; 55-75: −2 points ≥75: −3 points | Score −2 Score −1 Score 0 Score 1 Score 2 | 12-mo PFS2, score −2 vs score 2: 91% vs 65% |
| EBMT scoring system31 | • Disease status at auto-HSCT: 0-4 points CR/VGPR: +0 point PR: +1 point PR/SD/MR: +2 points Rel/prog: +3 points- ISS: 0-2 points ISS I: +0 point ISS II: +1 point ISS III: +2 points • Karnofsky performance status: +1 point | • Risk score 0 (0) • Risk score 1 (1) • Risk score 2 (2) • Risk score 3 (3) • Risk score 4 (≥4) | 12-mo PFS, risk score 0 vs risk score 4: 91.7% vs 57.1% |
| Score . | Variables . | Risk groups (sum) . | Clinical outcomes . |
|---|---|---|---|
| CIBMTR scoring system28 | • High-risk cytogeneticsa: +4 points • Pre-ASCT BMPCs ≥10%: +4 points • Albumin at diagnosis ≤3,5 g/dL: +2 points • Standard-risk cytogenetic: +1 point • No cytogenetic abnormality, BMPCs <10% at ASCT, and albumin ≥3.5 g/dL at diagnosis: +0 point | • Low risk (0-3) • Intermediate risk (4-8) • High risk (9-10) | 3-year PFS: 58% vs 49% vs 31% (P < .001) 3-year OS: 88% vs 81% vs 64% (P < .001) |
| S-ERMM(18) score29 | • LDH > ULN: +5 points • Presence of t(4;14): +5 points • Presence of del(17p): +3 points • Abnormal albumin: +3 points • BMPCs >60%: +3 points • FLC λ: +2 points | • Low risk (≤5) • Intermediate risk (6-10) • High risk (≥11) | Median OS: NR vs 59.5 mo vs 31.5 mo (P < .001) Median PFS2: 62.3 mo vs 40 vs 19.8 mo (P < .001) |
| DS-ERMM score29 | • S-ERMM score (0-21 points) • Achievement of at least VGPR: −4 points | • Low risk (≤0) • Intermediate risk (1-5) • High risk (≥6) | Median OS: NR vs NR vs 57.3 mo (P < .001) Median PFS2: NR vs 53.8 mo vs 40.2 mo (P < .001) |
| EBMT scoring system30 | • Disease status at ASCT: 0-3 points CR/VGPR: +0 point PR/SD/MR: +1 point Rel/prog: +3 points • ISS: ISS I: +0 point ISS II: +1 point ISS III: +2 points • Age (years): −1 to −3 points ≤55: −1 point; 55-75: −2 points ≥75: −3 points | Score −2 Score −1 Score 0 Score 1 Score 2 | 12-mo PFS2, score −2 vs score 2: 91% vs 65% |
| EBMT scoring system31 | • Disease status at auto-HSCT: 0-4 points CR/VGPR: +0 point PR: +1 point PR/SD/MR: +2 points Rel/prog: +3 points- ISS: 0-2 points ISS I: +0 point ISS II: +1 point ISS III: +2 points • Karnofsky performance status: +1 point | • Risk score 0 (0) • Risk score 1 (1) • Risk score 2 (2) • Risk score 3 (3) • Risk score 4 (≥4) | 12-mo PFS, risk score 0 vs risk score 4: 91.7% vs 57.1% |
t(4;14),t(14;16),t(14;20), del(13q/monosomy 13 on karyotype), del(17p),1q gain,1p del.
BMPCs, bone marrow plasma cells; CIBMTR, Center for Blood and Marrow Transplant Research; CR, complete response; DS-ERMM, dynamic simplified early relapse in multiple myeloma; EBMT, European Society for Blood and Marrow Transplantation; FLC, free light chain; MMRF, Multiple Myeloma Research Foundation; MR, minimal response; NR, not reached; PFS2, progression-free survival-2; Rel/prog, relapse/progression; SD, stable disease; S-ERMM18, simplified early relapse in multiple myeloma (18 months); ULN, upper limit of normal.
Many reports consistently highlight the potential impact on survival of response to therapy as a dynamic factor, particularly when considering minimal residual disease (MRD) negativity.39 Unfortunately, most of the studies focusing on the risk of early relapse included data on patients treated in the last 10 years with IMiDs and/or PI-based regimens and lack MRD data. In these studies the achievement of a suboptimal response (eg, less than VGPR) was more frequent in patients with early relapse.22,33,35,40 Similarly, a large metanalysis on 2190 patients showed that the incorporation of the response achieved (at least VGPR vs not) into the baseline risk score changed the risk status in 56% of patients, with the rate of patients at risk of an early relapse increasing from 7% to 20%.29
In today's clinical practice, the achievement of at least a VGPR could be an acceptable early dynamic prognostic factor, being a standard biochemical response evaluation achievable in a significant proportion of patients with most of the current therapies and supported by data from numerous reports. MRD status, which is a better predictor of outcome than VGPR, may replace the current response system and become a dynamic predictor of early relapse in the near future. In this regard both the incorporation of imaging techniques (eg, positron emission tography/computed tomography), demonstrated to be complementary to bone marrow MRD testing and possibly of particular importance in high-risk patients, where extramedullary disease is more common,41,42 and sustained MRD negativity may play a key role in modulating the risk of early relapse,6,43,44 thus impacting treatment strategies for standard-risk—and, more importantly, for high-risk— disease.
How can we manage FHR patients?
Patients with FHR currently represent an unmet medical need. In general, for patients with high-risk disease, up-front multiagent chemotherapy, single or tandem transplant, and single- or double- agent maintenance, when tolerated, are generally recommended.45,46 The treatment-free interval should be limited, as the disease may respond to therapy but rapidly relapse, especially if treatment is interrupted or de-escalated.44 Data from the MASTER trial showed that treatment interruption in very high-risk patients, even when MRD negativity is achieved, leads to a higher risk of MRD resurgence and suboptimal PFS.47 In addition, post hoc analysis of the FORTE study showed that doublet maintenance (carfilzomib-lenalidomide) compared with single-agent lenalidomide reduced the risk of MRD resurgence, but this is true only during doublet therapy, as after stopping carfilzomib the risk is equal to a patient receiving lenalidomide alone, and this is particularly evident in patients with high-risk disease.44
As FHR is currently defined by the pattern of relapse, specific considerations must be made. First, disease progression during treatment or soon after stopping therapy means the disease is refractory to that treatment; studies reported a high proportion of refractory patients in the early relapsed group.35 The patient discussed in our clinical case relapsed 2 months after HDM and less than 6 months after DVTd, meaning he can be considered refractory to HDM and to have a suboptimal duration of remission after DVTd, which would advise against retreatment with the same agents.48,49 A study analyzing the pattern of clonal evolution suggests that depth of response to treatment is the main determinant of the evolutionary pattern: patients relapsing early under treatment or with a suboptimal response mostly present a linear clonal evolution pattern, whereas patients achieving deep treatment response (complete response [CR] or MRD- negative status) are more likely to follow a branching evolutionary pattern.50 These data provide the rationale to investigate intensification strategies in patients with a suboptimal response to up-front therapy or to consider a class agent switch as salvage treatment with different targets and mechanisms of action.
The best combination to be administered in each patient is based on several factors, including refractoriness to prior regimens, expected tolerability, and drug availability.
Considerations can be made based on a post hoc analysis of randomized clinical trials that have established the current standards of care in the relapse setting (Table 4). Many of these trials analyzed the outcomes of patients with early vs late relapse. First, most of the 3-drug regimens currently recommended as salvage therapies also proved to be effective in patients with an early relapse, consistently improving CR and MRD- negativity rates and prolonging PFS. In the POLLUX study, the median PFS observed in patients with an early relapse increased from 12 months with lenalidomide and dexamethasone (Rd) to 37 months with daratumumab (DRd)51 ; in the ASPIRE study, the addition of carfilzomib to Rd prolonged the median PFS from 11 to 21 months in patients who progressed within 12 months from the start of the previous treatment.52 These regimens can both be considered valuable options in lenalidomide-naive patients who are also not refractory to either DRd or carfilzomib (KRd). Results in favor of a triplet regimen were also reported in the early relapse population treated with daratumumab, carfilzomib, and dexamethasone (DKd; hazard ratio [HR], 0.6, median PFS NR) in the CANDOR study and isatuximab, carfilzomib, and dexamethasone (IsaKd; HR, 0.6, median PFS 25 months) in the IKEMA study as compared to carfilzomib-dexamethasone (Kd) alone (median PFS of 23 months and 17 months, respectively).53,54 Based on these results, for patients relapsing early after a 3-drug regimen up front who are not daratumumab refractory, a triplet salvage combination based on an anti-CD38 MoAb in combination with either lenalidomide (DRd) or carfilzomib (DKd, IsaKd), if lenalidomide refractory, are the options of choice. Patients with an early relapse who are refractory to daratumumab have limited treatment options. In general, at first and second relapse a 3-drug combination of a proteasome inhibitor (bortezomib or carfilzomib) with pomalidomide (pomalidomide-bortezomib-dexamethasone [PVd], carfilzomib-pomalidomide-dexamethasone [KPd]), or alkylating agents (carfilzomib-cyclophosphamide-dexamethasone [KCd]/ bortezomib-cyclophosphamide-dexamethasone [VCd]) are viable treatment options, although efficacy data about these combinations in the early relapse are currently lacking. Similarly, pomalidomide-based regimens in combination with elotuzumab, a MoAb targeting SLAMF7, can also be considered as a third line.
Efficacy of approved regimens in patients with early vs late relapse
| Clinical trial . | Study design . | Definition of FHR . | Patients, n . | Clinical outcomes . |
|---|---|---|---|---|
| POLLUX51 | DRd vs Rd | Early relapse: progression within 18 months from the start of first-line treatment Late relapse: progression after 18 months from the start of first-line treatment | Early relapse, 99 DRd arm, 47 Rd arm, 52 Late relapse, 196 DRd arm, 102 Rd arm, 94 | DRd vs Rd PFS, median Early relapse: 37 vs 12 mo (HR, 0.41; P = .0002) Late relapse: 69 vs 28 months (HR, 0.53; P = .0007) CR rates Early relapse: 53% vs 12% Late relapse: 62 vs 38% MRD rates (10−5) Early relapse: 30% vs 4% Late relapse: 34 vs 14% |
| ASPIRE52 | KRd vs Rd | Early relapse: progression within 12 months from the start of the prior treatment line Late relapse: progression after 12 months from the start of the prior treatment line | Early relapse, 217 KRd arm, 113 Rd arm, 104 Late relapse, 520 KRd arm, 263 Rd arm, 267 | KRd vs Rd PFS, median Early relapse: 21 vs 11 mo (HR, 0.7; P = .0026) Late relapse: 30 vs 18 mo (HR, 0.68; P = .0005) |
| CASTOR51 | DVd vs Vd | Early relapse: progression within 18 months from the start of first-line treatment Late relapse: progression after 18 months from the start of first-line treatment | Early relapse, 49 DVd arm, 30 Vd arm, 19 Late relapse, 186 DVd arm, 92 Vd arm, 94 | DVd vs Vd PFS, median Early relapse: 15 vs 9 mo (HR, 0.51, P = .048) Late relapse: 28 vs 8 mo (HR, 0.2; P > .0001) CR rates Early relapse: 21% vs 17% Late relapse: 51% vs 14% MRD rates (10−5) Early relapse: 13% vs 0% Late relapse: 23% vs 13% |
| ENDEAVOR52 | Kd vs Vd | Early relapse: progression within 12 months from the start of the prior treatment line Late relapse: progression after 12 months from the start of the prior treatment line | Early relapse, 239 Kd arm, 123 Vd arm, 116 Late relapse, 675 Kd arm, 335 Vd arm, 340 | Kd vs Vd PFS, median Early relapse: 14 vs 6 mo (HR, 0.6; P = .0017) Late relapse: 22 vs 10 mo (HR, 0.5; P < .0001) |
| CANDOR53 | DKd vs Kd | Early relapse: progression within 18 months from the start of first-line treatment Late relapse: progression after 18 months from the start of first-line treatment | Early relapse, 92 DKd arm, 59 Kd arm, 33 Late relapse, 118 DKd arm, 82 Kd arm, 36 | DKd vs Kd PFS, median Early relapse: NR vs 13 months (HR, 0.6) Late relapse: NR vs NR (HR, 0.7) CR rates Early relapse: 29% vs 3% Late relapse: 39% vs 17% |
| IKEMA54 | IsaKd vs Kd | Early relapse: progression within 18 months (1 prior line of therapy), 12 months (2 or more prior treatments), or 12 months from ASCT Late relapse: progression after 18 months (1 prior line of therapy), 12 months (2 or more prior treatments), or 12 months from ASCT | Early relapse, 107 IsaKd arm, 61 Kd arm, 46 Late relapse, 176 IsaKd arm, 104 Kd arm, 72 | Isakd vs Kd PFS, median Early relapse: 25 vs 17 mo (HR, 0.6) Late relapse: 43 vs 22 mo (HR, 0.5) MRD rates (10−5) Early relapse: 25% vs 15% Late relapse: 39% vs 17% |
| Clinical trial . | Study design . | Definition of FHR . | Patients, n . | Clinical outcomes . |
|---|---|---|---|---|
| POLLUX51 | DRd vs Rd | Early relapse: progression within 18 months from the start of first-line treatment Late relapse: progression after 18 months from the start of first-line treatment | Early relapse, 99 DRd arm, 47 Rd arm, 52 Late relapse, 196 DRd arm, 102 Rd arm, 94 | DRd vs Rd PFS, median Early relapse: 37 vs 12 mo (HR, 0.41; P = .0002) Late relapse: 69 vs 28 months (HR, 0.53; P = .0007) CR rates Early relapse: 53% vs 12% Late relapse: 62 vs 38% MRD rates (10−5) Early relapse: 30% vs 4% Late relapse: 34 vs 14% |
| ASPIRE52 | KRd vs Rd | Early relapse: progression within 12 months from the start of the prior treatment line Late relapse: progression after 12 months from the start of the prior treatment line | Early relapse, 217 KRd arm, 113 Rd arm, 104 Late relapse, 520 KRd arm, 263 Rd arm, 267 | KRd vs Rd PFS, median Early relapse: 21 vs 11 mo (HR, 0.7; P = .0026) Late relapse: 30 vs 18 mo (HR, 0.68; P = .0005) |
| CASTOR51 | DVd vs Vd | Early relapse: progression within 18 months from the start of first-line treatment Late relapse: progression after 18 months from the start of first-line treatment | Early relapse, 49 DVd arm, 30 Vd arm, 19 Late relapse, 186 DVd arm, 92 Vd arm, 94 | DVd vs Vd PFS, median Early relapse: 15 vs 9 mo (HR, 0.51, P = .048) Late relapse: 28 vs 8 mo (HR, 0.2; P > .0001) CR rates Early relapse: 21% vs 17% Late relapse: 51% vs 14% MRD rates (10−5) Early relapse: 13% vs 0% Late relapse: 23% vs 13% |
| ENDEAVOR52 | Kd vs Vd | Early relapse: progression within 12 months from the start of the prior treatment line Late relapse: progression after 12 months from the start of the prior treatment line | Early relapse, 239 Kd arm, 123 Vd arm, 116 Late relapse, 675 Kd arm, 335 Vd arm, 340 | Kd vs Vd PFS, median Early relapse: 14 vs 6 mo (HR, 0.6; P = .0017) Late relapse: 22 vs 10 mo (HR, 0.5; P < .0001) |
| CANDOR53 | DKd vs Kd | Early relapse: progression within 18 months from the start of first-line treatment Late relapse: progression after 18 months from the start of first-line treatment | Early relapse, 92 DKd arm, 59 Kd arm, 33 Late relapse, 118 DKd arm, 82 Kd arm, 36 | DKd vs Kd PFS, median Early relapse: NR vs 13 months (HR, 0.6) Late relapse: NR vs NR (HR, 0.7) CR rates Early relapse: 29% vs 3% Late relapse: 39% vs 17% |
| IKEMA54 | IsaKd vs Kd | Early relapse: progression within 18 months (1 prior line of therapy), 12 months (2 or more prior treatments), or 12 months from ASCT Late relapse: progression after 18 months (1 prior line of therapy), 12 months (2 or more prior treatments), or 12 months from ASCT | Early relapse, 107 IsaKd arm, 61 Kd arm, 46 Late relapse, 176 IsaKd arm, 104 Kd arm, 72 | Isakd vs Kd PFS, median Early relapse: 25 vs 17 mo (HR, 0.6) Late relapse: 43 vs 22 mo (HR, 0.5) MRD rates (10−5) Early relapse: 25% vs 15% Late relapse: 39% vs 17% |
Despite the efficacy demonstrated by these regimens in a patient with an early relapse, the survival outcomes observed in this population are still significantly inferior to those reported in patients with a late relapse. Furthermore, as many patients experiencing an early relapse today will also be refractory to daratumumab and/or lenalidomide, since both drugs have become a mainstay of the induction and maintenance strategies, their treatment at the time of relapse poses important challenges. In this light, new salvage agents such as chimeric antigen receptor (CAR) T cells and bispecific antibodies, with different targets and mechanisms of action, represent an appealing option (Table 5). In cohort 2a of the KarMMa-2 study,55 idecabtagene vicleucel (ide-cel), a B-cell maturation antigen (BCMA)–directed CAR T-cell therapy currently approved for patients with at least 4 prior lines of therapy in the United States and 3 in Europe, is being investigated as a salvage treatment in patients who underwent ASCT and had an early relapse (89% of patients progressed within 12 months from ASCT). Ide-cel resulted in an overall response rate of 84%, with 46% of patients achieving at least a CR, an almost double rate compared to that (24%) reported with the first-line therapy in this patient population.55 While the median PFS reported in the overall cohort of patients was only 11.4 months, a longer duration of response (24 months) was observed in patients achieving a CR/stringent(s)CR,55 thus highlighting on one hand the challenges in the treatment of this functional high-risk population and on the other the importance of the depth of response. In a similar phase 2 study (CARTITUDE-2, cohort B) conducted in patients relapsing within 12 months since initial treatment or ASCT, ciltacabtagene autoleucel (cilta-cel), another approved anti-BCMA CAR T cell, induced at least a CR in 89% of treated patients, 75% of whom were also MRD-negative (next-generation sequencing, 10−5): these results translated into an 18-month PFS of 83%, thus already superseding the duration of the first remission for most patients.56
Prospective clinical studies with CAR T cells in patients with an early relapse
| Clinical trial . | Study design . | Definition of FHR . | Patients . | Clinical outcomes . |
|---|---|---|---|---|
| KarMMA-2, cohort 2a55 | Ide-cel | ER: progressive disease within 18 months from first-line treatment including induction, ASCT, and lenalidomide maintenance | n = 37 | ORR, 84% CR rate 46% PFS, median 11.4 mo 2-y OS, 85% DOR, median • Overall population, 16 mo • Patients in CR, 24 mo |
| KarMMA-2, cohort 2c57 | Ide-cel | Inadequate response (less than VGPR) after up-front ASCT | n = 31 | ORR, 87% CR rate, 74% MRD rates (10−5), 42% |
| CARTITUDE 2, cohort b56 | Cilta-cel | ER: progressive disease after initial therapy including PIs and IMiDs within 12 months since ASCT or start of first-line treatment | n = 19 | ORR, 100% CR or better rates, 90% MRD rates (10−5), 74% 18-mo PFS, 83% 18-mo OS, 83% |
| Clinical trial . | Study design . | Definition of FHR . | Patients . | Clinical outcomes . |
|---|---|---|---|---|
| KarMMA-2, cohort 2a55 | Ide-cel | ER: progressive disease within 18 months from first-line treatment including induction, ASCT, and lenalidomide maintenance | n = 37 | ORR, 84% CR rate 46% PFS, median 11.4 mo 2-y OS, 85% DOR, median • Overall population, 16 mo • Patients in CR, 24 mo |
| KarMMA-2, cohort 2c57 | Ide-cel | Inadequate response (less than VGPR) after up-front ASCT | n = 31 | ORR, 87% CR rate, 74% MRD rates (10−5), 42% |
| CARTITUDE 2, cohort b56 | Cilta-cel | ER: progressive disease after initial therapy including PIs and IMiDs within 12 months since ASCT or start of first-line treatment | n = 19 | ORR, 100% CR or better rates, 90% MRD rates (10−5), 74% 18-mo PFS, 83% 18-mo OS, 83% |
CR, complete response; DOR, duration of response; ER, early relapse; ORR, overall response rate.
Given the promising results of T-cell redirecting therapies also in patients with early relapse and aggressive disease, efforts should be made to grant access to bispecific antibodies and CAR T cells for this high-risk population; however, the current label for both bispecific antibodies and CAR T cells, after the third or fourth line of therapy rather than based on drug class refractoriness, is a clear limitation. Of even more interest is to build up on the correlation between the depth of response at first line and the risk of early relapse, thus looking at an early change of treatment approach in patients with suboptimal responses to first-line therapy. This led to the investigation of a treatment intensification strategy with ide-cel in NDMM patients achieving less than a VGPR after ASCT.57 Preliminary results in the 31 treated patients demonstrated a promising efficacy: 74% of patients achieved at least a CR, and the MRD negativity (next-generation flow, 10−5) in the overall population was 42%.57 Altogether, these results, though preliminary, suggest that CAR T cells, either used as salvage therapies after early relapse or as a treatment intensification in the presence of a suboptimal response after transplant, could be promising strategies. Ongoing phase 3 trials are currently investigating intensification in patients with a suboptimal response.
Finally, optimal timing to start therapy and the role of continuous treatment should be considered. Prospective and retrospective studies in relapse showed a potential benefit in patients who received therapy at biochemical rather than at clinical relapse.58 It is true that in patients with high-risk disease there is often a short interval between biochemical and clinical relapse, but if one may argue that we lack sufficient evidence for changing the treatment approach for suboptimal response, it could be reasonable to change therapy in early relapse at first signs of confirmed serological relapse. Continuous treatment proved to be effective up front and at relapse. This can suggest the potential importance of prolonged therapy even following newer anti-BCMA agents in the context of early relapse and to help prolong the duration of response.
Conclusions
FHR patients represent an unmet medical need even in the context of highly effective up-front and salvage multidrug regimens. Current challenges in managing FHR patients consist of a correct identification of patients at higher risk of early relapse through baseline and dynamic risk factors as well as the development of strategies that aim to prevent early relapse in high-risk patients together with effective salvage treatments. In this light, the use of the most effective regimen up front (quadruplets rather than triplets), incorporating response to treatment in dynamic risk stratification models, early treatment intensification in patients with a suboptimal response and class-drug/switch at relapse, as well as the early use of new immunotherapeutic approaches (CAR T cells and bispecific antibodies) and early treatment in case of MRD-resurgence or biochemical relapse are promising strategies to be validated in clinical studies.
Conflict-of-interest disclosure
Francesca Gay: honoraria: Janssen, Celgene/Bristol Myers Squibb, Takeda, Amgen, Sanofi, GSK, Roche, Abbvie; advisory board: Janssen, Celgene/Bristol Myers Squibb, Takeda, Amgen, Sanofi, GSK, Roche, Abbvie, Pfizer, Oncopeptides.
Giuseppe Bertuglia: no competing financial interests to declare.
Roberto Mina: honoraria: Janssen, Celgene/Bristol Myers Squibb, Takeda, Amgen; advisory board: Janssen, Celgene/Bristol Myers Squibb, Takeda, Amgen; consultancy: Janssen, Takeda, Sanofi.
Off-label drug use
Francesca Gay: nothing to disclose.
Giuseppe Bertuglia: nothing to disclose.
Roberto Mina: nothing to disclose.