Abstract
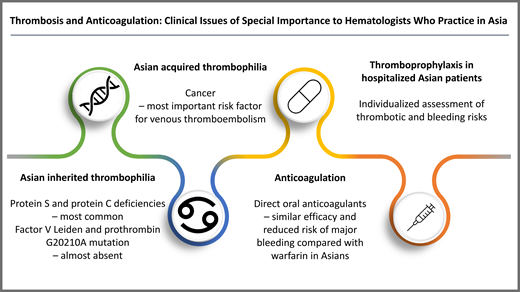
There are clinical issues of special importance and practice variation in the management of venous thromboembolism (VTE) and in the use of anticoagulants among hematologists who practice in Asia. In Asian-inherited thrombophilia, coagulation is disturbed due to loss-of-function mutations of protein S and protein C causing protein S and protein C deficiencies, whereas the gain-of-function factor V Leiden and prothrombin G20210A mutations are almost absent. Thrombophilia screening is not recommended in patients with VTE patients who have major provoking factors. However, it can be considered in unprovoked young patients with VTE who have a strong family history of VTE. Cancer is the most important acquired risk factor for VTE in Asians. Limited cancer screening at the initial presentation of unprovoked VTE is appropriate, especially in the elderly. Direct oral anticoagulants have been shown to have similar efficacy and reduce risk of major bleeding, including intracranial hemorrhage and bleeding requiring hospitalization, compared with warfarin. Most clinical trials evaluating therapies for treatment and prevention of VTE have included small numbers of Asian patients. Despite this lack of evidence, direct oral anticoagulants have been increasingly used in Asia for cancer-associated thrombosis. Individualized assessment of thrombotic and bleeding risks should be used for all hospitalized Asian patients when deciding on pharmacologic thromboprophylaxis. More research is needed to understand the factors that contribute to risks of VTE and anticoagulant-associated bleeding in Asian patients as these may differ from Western populations.
Learning Objectives
Describe the hereditary and acquired risk factors for venous thromboembolism in Asians, including appropriate screening for inherited thrombophilia and cancer in Asian patients presenting with venous thromboembolism
Understand the risk of bleeding associated with anticoagulants in Asian patients
Describe individualized assessment of thrombotic and bleeding risks when deciding on thromboprophylaxis in hospitalized Asian patients
Introduction
Venous thromboembolism (VTE), which includes deep vein thrombosis (DVT) and pulmonary embolism (PE), is a multifactorial condition that is associated with genetic and environmental risk factors. The incidence of VTE in the Asian population, particularly in the Far East, has been perceived to be lower than in other ethnic groups. Recent systematic review demonstrated that population-wide incidence estimates of VTE in Asia were 13.8 in Korea, 15.9 in Taiwan, and 19.9 per 100 000 people in Hong Kong.1 These rates equate to ~15% to 20% of the incidence in Western countries (which are about 100 per 100 000 of the population). However, the incidence of VTE in Asia has increased over time. For example, an almost 5-fold increase in the annual incidence of PE was recorded between 1997 and 2008 in the Chinese PE registry.2 This trend might be the result of more awareness among physicians toward the diagnosis of VTE. We present some of the special considerations in venous thrombosis and anticoagulant management in Thai patients seen at our institution using 4 illustrative patient case studies. The meaning of “Asian” throughout this article refers to persons living in the Far East (East Asians and Southeast Asians).
CLINICAL CASE 1
A 37-year-old Asian man had a history of unprovoked proximal DVT of the left leg 2 years previously. He was taking rivaroxaban for 6 months before being lost to follow-up. On this occasion, he presented with severe abdominal pain, and a diagnosis of superior mesenteric vein thrombosis was made on computed tomography (CT) scan. He denied any provoking factors but was aware of history of VTE in the family. Thrombophilia evaluation showed low plasma activity level of protein S (31%; normal range, 61%-127%), normal plasma activity levels of protein C (79%; normal range, 64%-141%), and antithrombin (91%; normal range, 80%-120%). He was started on a therapeutic dose of low-molecular-weight heparin (LWMH) and transitioned to warfarin with a target international normalized ratio (INR) of 2.0 to 3.0.
Hereditary thrombophilia in the Asian population differs from that in Western countries. Protein S and protein C deficiencies are the most prevalent, while factor V Leiden and prothrombin G20210A mutation are almost absent.3 Table 1 demonstrates the frequency of inherited thrombophilia among healthy participants and among unselected patients with VTE in Asians and Caucasians.3 Mutations in the protein S and the protein C genes in Asians also differ from Caucasians. Protein S Tokushima (p.Lys196Glu), protein C p.Arg189Trp, and protein C p.Lys193del are prevalent among East and Southeast Asians but are absent among Caucasians.4
Racial differences in the distribution of inherited thrombophilias3
| . | Healthy individuals, % . | Unselected patients with VTE, % . | ||
|---|---|---|---|---|
| Characteristic . | Asians . | Caucasians . | Asians . | Caucasians . |
| Protein S deficiency | 0.06-3.7 | 0.03-0.13 | 10.7-17.8 | 2.3 |
| Protein C deficiency | 0.3-1.1 | 0.2-0.4 | 8.9-10.7 | 2.3 |
| Antithrombin deficiency | 0-2.3 | 0.02 | 4.7-8.1 | 1.9 |
| Factor V Leiden mutation | 0-0.2 | 4.8 | 0 | 18.8 |
| Prothrombin G20210A mutation | 0-0.2 | 2.7 | 0 | 7.1 |
| . | Healthy individuals, % . | Unselected patients with VTE, % . | ||
|---|---|---|---|---|
| Characteristic . | Asians . | Caucasians . | Asians . | Caucasians . |
| Protein S deficiency | 0.06-3.7 | 0.03-0.13 | 10.7-17.8 | 2.3 |
| Protein C deficiency | 0.3-1.1 | 0.2-0.4 | 8.9-10.7 | 2.3 |
| Antithrombin deficiency | 0-2.3 | 0.02 | 4.7-8.1 | 1.9 |
| Factor V Leiden mutation | 0-0.2 | 4.8 | 0 | 18.8 |
| Prothrombin G20210A mutation | 0-0.2 | 2.7 | 0 | 7.1 |
The risk of first VTE increases with thrombophilia.5,6 Protein S and protein C deficiencies are reported to result in an increased relative risk of first VTE of 30.6 (95% confidence interval [CI], 26.9-55.3) and 24.1 (95% CI, 13.7-42.4), respectively, whereas factor V Leiden and prothrombin G20210A mutation are reported to result in an increased relative risk of first VTE of 7.5 (95% CI, 4.4-12.6) and 5.2 (95% CI, 2.8-9.7), respectively, compared with patients without an inherited thrombophilia.6 The risk of VTE recurrence is not influenced by factor V Leiden and prothrombin G20210A mutation. However, patients with protein S and protein C deficiencies had an increase in risk of recurrence.6-8 Despite lower VTE incidence, East Asians appear to have similar rates of recurrent VTE compared with Caucasians.7
A recent prospective study of PE in Chinese patients found that 7.1% of patients had inherited thrombophilia, and the risk of recurrence or death was similar between those with or without inherited thrombophilia receiving anticoagulant therapy.9 Regardless of the presence of thrombophilia, the risk of recurrence increases after stopping anticoagulant therapy in patients with unprovoked VTE.6 Therefore, indefinite duration of anticoagulant is generally recommended for those with unprovoked VTE who do not have a high risk for bleeding complications.10 Results of inherited thrombophilia do not alter the anticoagulant management.
Thrombophilia screening is not recommended in patients with VTE who have major provoking factors. However, it can be considered in unprovoked young patients with VTE (younger than 50 years) with a strong family history of VTE. Thrombophilia screening may potentially benefit family members of an index case as they have a higher risk of VTE.5,6 Any recommendation to perform thrombophilia screening should be discussed with patients and their families.
CLINICAL CASE 1 (Continued)
The patient was ultimately diagnosed with protein S deficiency. Protein S levels were checked while not on anticoagulant. Testing for deficiencies of natural anticoagulants should be performed only after 3 months of anticoagulation for acute thrombosis. Checking levels of regulatory proteins is helpful if the levels are normal (thus ruling out a deficiency state). Due to his history of recurrent unprovoked VTE, he was instructed to be on long-term anticoagulant therapy. Although direct oral anticoagulants (DOACs) are not contraindicated in protein S deficiency, he was restarted on warfarin due to financial issues.
CLINICAL CASE 2
A 67-year-old Asian woman with no pertinent medical history presented with left leg swelling of 2 months' duration. She had experienced an unintentional 4-kg weight loss in the past 2 months. Physical examination showed marked swelling of the left leg with redness and warmth. Physical examination was otherwise unremarkable. Doppler ultrasound revealed acute DVT in the left common femoral vein extending to the popliteal vein. She was evaluated for underlying malignancy. Tumor marker screening revealed a markedly elevated CA-125 level. Ultrasound of the abdomen showed a large ovarian mass suggestive of ovarian cancer. She was initially prescribed rivaroxaban 15 mg twice daily and was referred to the hematology service regarding further anticoagulant management.
Cancer is the most important acquired risk factor for VTE in the Asian population. Many observational studies have reported that cancer is the most common risk factor associated with VTE in Asians.11,12 Recent data from the GARFIELD VTE registry, a prospective observational study of patients with symptomatic VTE that included 1822 Asians, confirmed that active cancer was the most common risk factor for VTE (19.8%). This proportion is significantly greater than non-Asian populations (8.1%).13 The most common site of VTE was also different in this study. While lymphoma, gynecologic cancer, and lung cancer are the most common types of cancer associated with VTE in Asia, lung, breast, and colorectal cancers are the most common in non-Asian populations.
Patients with unprovoked VTE may also subsequently develop cancer. Among Asian patients with unprovoked VTE, 7% had a subsequent cancer diagnosis within 2 years.14 In the Western population, this rate is 3.9% in 1 year.15 Limited cancer screening at the initial presentation of seemingly “unprovoked” VTE is appropriate, especially in the elderly. This should include thorough history taking, physical examination (including pelvic examination), routine laboratory investigations (complete blood count, calcium, urinalysis, and liver function tests), and chest x-ray. In addition, cancer screening appropriate for age and sex (breast, cervix, colon, and prostate) is recommended as per national guidelines. Routine CT scan of the whole abdomen and pelvis and tumor markers are not recommended. However, these investigations are frequently performed in clinical practice. The recent National Institute for Health and Care Excellence guideline from 2020 recommends against extensive investigations for cancer in patients with unprovoked VTE unless they have relevant clinical symptoms or signs.16 A previous study in Caucasians demonstrated that extensive cancer screening, including CT whole abdomen and pelvis plus limited screening, did not result in significant early detection of cancer or improve cancer-related survival than limited screening.15 However, it should be noted that data regarding cancer screening in unprovoked VTE in Asian patients are limited. Furthermore, national guidelines regarding cancer screening are not available in many Asian countries. Therefore, cancer screening recommendations from Western guidelines are usually applied. The clinical benefit of extensive cancer screening, including tumor marker screening, needs to be elucidated in Asian populations. We summarize in Table 2 the proposed cancer screening algorithm in unprovoked VTE as per Asian guidelines adapted from Western guidelines.17-19
Recommendation for cancer screening in patients with unprovoked venous thromboembolism
| All cancers . | All patients . | Thorough history and physical examination (complete blood count, calcium, urine analysis, liver function tests, and chest x-ray) . |
|---|---|---|
| Breast cancer | Women aged 50-69 years (in countries with medium to high incidence of breast cancer) Women aged 40-49 and 70-74 years | Mammogram regularly annual or every 2 years Regular mammography may also be done |
| Cervical cancer | Women aged 20-65 years | Pelvic examination and Pap smear if had not been performed in 2 years |
| Prostate cancer | Men aged 45-79 years | Serum prostate-specific antigen |
| Colorectal cancer | All aged >45 years | Fecal immunochemical test or colonoscope |
| All cancers . | All patients . | Thorough history and physical examination (complete blood count, calcium, urine analysis, liver function tests, and chest x-ray) . |
|---|---|---|
| Breast cancer | Women aged 50-69 years (in countries with medium to high incidence of breast cancer) Women aged 40-49 and 70-74 years | Mammogram regularly annual or every 2 years Regular mammography may also be done |
| Cervical cancer | Women aged 20-65 years | Pelvic examination and Pap smear if had not been performed in 2 years |
| Prostate cancer | Men aged 45-79 years | Serum prostate-specific antigen |
| Colorectal cancer | All aged >45 years | Fecal immunochemical test or colonoscope |
Although cancer is the most important acquired risk factor for VTE in Asia, the rate of VTE prophylaxis in patients with cancer is low. One of the reasons for the difficulties in VTE prophylaxis for patients with cancer in Asia is that the VTE risk assessment scores are not validated in Asians and may not be applicable for Asian patients. The average body mass index (BMI) of persons in many Asian countries is lower than the countries in which the Khorana risk score was developed and validated, and so the BMI component of this score (35 kg/m2 or more) may not be as broadly applicable in these countries. Asians tend to have a lower BMI in comparison to Caucasians due to differences in body build and muscularity.20 For the treatment of cancer- associated VTE, LMWH or DOACs can be used. The efficacy of DOACs in cancer-associated thrombosis has been demonstrated in randomized trials. However, those trials included only a small number of Asian patients. A retrospective study from a Taiwanese database showed that DOACs are associated with similar risk of recurrent VTE and bleeding compared with LMWH in the Asian population.21 DOACs should be used with caution in those with gastrointestinal or urogenital cancer.
CLINICAL CASE 2 (Continued)
Because of an elevated clinical suspicion for underlying malignancy, abdominal CT scan revealed a large ovarian mass compressing the left external iliac vein. The patient was diagnosed with DVT associated with ovarian cancer. Two weeks after rivaroxaban was started, her swollen leg persisted. She was switched to therapeutic-dose enoxaparin and underwent tumor removal surgery. After the tumor was removed, her left leg was much improved, and she was switched back to rivaroxaban without further incident. It is important to recognize that acquired risk factors for VTE, including cancer, affect individuals of all racial groups.
CLINICAL CASE 3
An 86-year-old Asian man presented with a sudden onset of left hemiparesis. His underlying history included atrial fibrillation (AF), for which he was on warfarin for stroke prevention (CHA2DS2-VASc score = 4), as well as a previous unprovoked proximal DVT. He also had hypertension. CT brain revealed intracerebral hemorrhage in the right basal ganglia. His INR was 3.2. Warfarin was held, and reversal agents (vitamin K and prothrombin complex concentrates) were given.
Bleeding associated with anticoagulant use remains a significant concern. In patients with AF treated with warfarin, the risk of intracranial hemorrhage is higher in Asians than in non-Asians (1.8% vs 0.4%).22 The risk of major bleeding or clinically relevant nonmajor bleeding is also numerically higher in Asian patients with VTE treated with warfarin compared with non-Asians (11.7% vs 9.4%).23 Low body weight resulting in low creatinine clearance as well as multiple comorbidities could contribute to an increased risk of bleeding.12 In addition, older age, poor nutritional status, uncontrolled hypertension, and concurrent antiplatelet agents increase the bleeding risk in patients treated with warfarin. Herbal medicines that could interact with warfarin should be sought. In Asians, there are lower frequencies of polymorphisms in CYP2C9 and VKORC1 genes that lead to either reduced metabolic activity or attenuated sensitivity to warfarin compared with Caucasians. The median warfarin dose required was significantly higher in Caucasians than in Asian patients.24 Initial warfarin starting dose of 3 or 5 mg in Asians is more appropriate than 5 to 10 mg warfarin recommended in Western guidelines.25
Although warfarin has been a major anticoagulant for stroke prevention in AF and VTE treatment for decades, DOACs have been increasingly used in Asian countries.13 DOACs have demonstrated their efficacy and safety in the subgroup analysis of pivotal randomized controlled trials and in real-world studies. DOACs have similar efficacy and reduce risk of major bleeding, including intracranial hemorrhage and bleeding requiring hospitalization compared with warfarin in patients with AF and VTE (Tables 3 and 4).23,26-35 However, special attention to DOAC use in Asians includes patients with extremely low body weight. Patients with body weight less than 40 kg were rarely included in the randomized controlled trials. Potential drug interaction, including herbal medicines or traditional Chinese medicines, could increase risk of bleeding.36 Availability of specific reversal agents also varies by country. Thus, cost-effectiveness of DOACs compared with warfarin should be considered in each country. Balancing thrombotic and bleeding risks is essential in the consideration of anticoagulant management. Factors that could increase risk of bleeding should be minimized as much as possible.
The efficacy and safety of DOACs and warfarin in pivotal atrial fibrillation randomized controlled trials in Asians
| Study . | Type of DOACs and doses . | Stroke and systemic embolism, n/N (% patient years) . | Major bleeding, n/N (% patient years) . | ||
|---|---|---|---|---|---|
| DOACs . | Warfarin . | DOACs . | Warfarin . | ||
| RELY30 | Dabigatran 150 mg po twice daily | 25/933 (1.4) | 53/926 (3.1) | 39/933 (2.2) | 66/926 (3.8) |
| Dabigatran 110 mg po twice daily | 44/923 (2.5) | 39/923 (2.2) | |||
| ROCKET AF31 | Rivaroxaban 20 mg po once daily | 21/932 (2.6) | 27/464 (3.4) | 23/932 (3.4) | 35/464 (5.1) |
| ARISTOTLE32 | Apixaban 5 mg po twice daily | 44/988 (2.5) | 60/1005 (3.4) | 33/988 (2.0) | 63/1005 (3.8) |
| ENGAGE TIMI33 | Edoxaban 60 mg po once daily | 20/642 (1.3) | 38/641 (2.6) | 42/642 (2.9) | 68/641 (4.8) |
| Edoxaban 30 mg po once daily | 38/652 (2.5) | 24/652 (1.6) | |||
| Study . | Type of DOACs and doses . | Stroke and systemic embolism, n/N (% patient years) . | Major bleeding, n/N (% patient years) . | ||
|---|---|---|---|---|---|
| DOACs . | Warfarin . | DOACs . | Warfarin . | ||
| RELY30 | Dabigatran 150 mg po twice daily | 25/933 (1.4) | 53/926 (3.1) | 39/933 (2.2) | 66/926 (3.8) |
| Dabigatran 110 mg po twice daily | 44/923 (2.5) | 39/923 (2.2) | |||
| ROCKET AF31 | Rivaroxaban 20 mg po once daily | 21/932 (2.6) | 27/464 (3.4) | 23/932 (3.4) | 35/464 (5.1) |
| ARISTOTLE32 | Apixaban 5 mg po twice daily | 44/988 (2.5) | 60/1005 (3.4) | 33/988 (2.0) | 63/1005 (3.8) |
| ENGAGE TIMI33 | Edoxaban 60 mg po once daily | 20/642 (1.3) | 38/641 (2.6) | 42/642 (2.9) | 68/641 (4.8) |
| Edoxaban 30 mg po once daily | 38/652 (2.5) | 24/652 (1.6) | |||
po, per os.
The efficacy and safety of DOACs and warfarin in pivotal venous thromboembolism randomized controlled trials in Asians
| Study . | Type of DOACs and dose . | Recurrent VTE or VTE-related death, n/N (%) . | Major bleeding or clinically relevant bleeding, n/N (%) . | ||
|---|---|---|---|---|---|
| DOACs . | Warfarin . | DOACs . | Warfarin . | ||
| RECOVER I and II | Dabigatran 150 mg po twice daily | 7/292 (2.4) | 3/310 (1.0) | 22/292 (7.5) | 26/310 (8.4) |
| EINSTEIN-DVT | Rivaroxaban 15 mg twice daily 21 days, then 20 mg once daily | 3/229 (1.3) | 8/219 (3.7) | 19/227 (8.4) | 25/217 (11.5) |
| EINSTEIN-PE | Rivaroxaban 15 mg twice daily 21 days, then 20 mg once daily | 8/163 (4.9) | 5/156 (3.2) | 16/161 (9.9) | 17/154 (11.0) |
| AMPLIFY | Apixaban 10 mg twice daily 7 days, then 5 mg twice daily | 7/223 (3.1) | 9/223 (4.0) | 7/223 (3.1) | 15/223 (6.7) |
| Hokusai-VTE | Edoxaban 60 mg or 30 mg once daily | 27/866 (3.1) | 34/861 (3.9) | 75/866 (8.7) | 125/861 (14.5) |
| AMPLIFY-J34 | Apixaban 10 mg twice daily 7 days, then 5 mg twice daily | 0/40 (0) | 1/40 (2.5) | 3/40 (7.5) | 11/39 (28.2) |
| J-EINSTEIN DVT and PE35 | Rivaroxaban 10 mg twice daily or 15 mg twice daily for 3 weeks followed by 15 mg once daily | 1/78 (1.3) | 1/19 (5.3) | 6/77 (7.8) | 1/19 (5.3) |
| Study . | Type of DOACs and dose . | Recurrent VTE or VTE-related death, n/N (%) . | Major bleeding or clinically relevant bleeding, n/N (%) . | ||
|---|---|---|---|---|---|
| DOACs . | Warfarin . | DOACs . | Warfarin . | ||
| RECOVER I and II | Dabigatran 150 mg po twice daily | 7/292 (2.4) | 3/310 (1.0) | 22/292 (7.5) | 26/310 (8.4) |
| EINSTEIN-DVT | Rivaroxaban 15 mg twice daily 21 days, then 20 mg once daily | 3/229 (1.3) | 8/219 (3.7) | 19/227 (8.4) | 25/217 (11.5) |
| EINSTEIN-PE | Rivaroxaban 15 mg twice daily 21 days, then 20 mg once daily | 8/163 (4.9) | 5/156 (3.2) | 16/161 (9.9) | 17/154 (11.0) |
| AMPLIFY | Apixaban 10 mg twice daily 7 days, then 5 mg twice daily | 7/223 (3.1) | 9/223 (4.0) | 7/223 (3.1) | 15/223 (6.7) |
| Hokusai-VTE | Edoxaban 60 mg or 30 mg once daily | 27/866 (3.1) | 34/861 (3.9) | 75/866 (8.7) | 125/861 (14.5) |
| AMPLIFY-J34 | Apixaban 10 mg twice daily 7 days, then 5 mg twice daily | 0/40 (0) | 1/40 (2.5) | 3/40 (7.5) | 11/39 (28.2) |
| J-EINSTEIN DVT and PE35 | Rivaroxaban 10 mg twice daily or 15 mg twice daily for 3 weeks followed by 15 mg once daily | 1/78 (1.3) | 1/19 (5.3) | 6/77 (7.8) | 1/19 (5.3) |
CLINICAL CASE 3 (Continued)
The patient had a high risk of both thrombosis and bleeding. After discussion with the patient and his family, anticoagulation was resumed with apixaban 4 weeks after the bleeding. His blood pressure was strictly controlled. Fortunately, he achieved full neurologic recovery with conservative management. Modifiable risk factors for bleeding (such as hypertension, labile INRs, anemia, thrombocytopenia, use of drugs and alcohol) should be strictly controlled in Asian patients on anticoagulants in order to reduce the risk of bleeding complications.
Due to the concern of bleeding in Asians, low-intensity anticoagulation has been practiced for both AF and VTE. The use of a lower dose of DOACs might be due to higher proportion of elderly patients and higher frequency of renal impairment. Real-world data in Asian studies showed that underdosing was observed in 27% to 36% of patients with AF who have suboptimal outcomes.37 For VTE treatment, low-intensity anticoagulant for the treatment of VTE has been recommended by the Japanese guideline for VTE, for which the recommended target INR is 1.5 to 2.5 rather than 2.0 to 3.0, due to increased risk of bleeding.38 In addition, a rivaroxaban dose of 15 mg (instead of 20 mg) once daily is recommended for the treatment of VTE during the first 3 months.35 Although these goals have not been adopted in many Asian countries, data from the GARFIELD registry confirmed that Asians were more likely to receive a reduced daily dose than non-Asian populations.13 For now, using a reduced dose of DOACs or low-intensity anticoagulation in AF and VTE treatment should be limited to countries where its efficacy and safety have been established.37,38
CLINICAL CASE 4
A 65-year-old Asian man was hospitalized in the intensive care unit (ICU) due to sepsis with severe thrombocytopenia. He was on mechanical ventilation with sedation due to hemodynamic instability. Three days later, he developed a sudden decrease in oxygenation. CT pulmonary angiogram revealed acute PE.
The rate of thromboprophylaxis in the medical ward and in the ICU in Asians is low.39 This is likely from the perception of low thrombotic risk and concern over the risk of bleeding. The incidence of all VTE in intensive care settings in Asian patients is ~6.6% to 10%.1 The incidence of symptomatic VTE in medical hospitalization is ~0.2% to 0.9%.40 These numbers are lower than those in Western countries. The American Society of Hematology guideline panel states that acutely ill and critically ill medical patients should receive pharmacologic VTE prophylaxis.41 With a lower rate of VTE and high bleeding risk, whether these recommendations can be applied to Asian patients needs further validation. Moreover, prediction tools that have been investigated to assess VTE risk, including the Padua score and the International Medical Prevention Registry on Venous Thromboembolism (IMPROVE) VTE score, and to assess bleeding risk, including the IMPROVE bleeding score in medical hospitalized patients, have not been extensively validated in Asian patients. One Chinese study validated the IMPROVE bleeding score in medical hospitalized patients. Scores of ≥7 and <7 had clinically relevant bleeding rates of 11% and 2%, respectively.42
In critically ill patients, routine pharmacologic thromboprophylaxis could increase the risk of bleeding. Until more robust evidence specific to Asians is available, individualized patient risk assessment for thrombosis and bleeding should be used for all hospitalized medically ill patients.43 History of VTE, active cancer, immobilization, and known thrombophilia are important risk factors for VTE. Patients with these risk factors should receive pharmacologic thromboprophylaxis if the risk of bleeding is judged to be acceptable. In those with high bleeding risk or with active bleeding, mechanical thromboprophylaxis should be considered.
In surgical patients, the incidence of symptomatic VTE after general and gynecologic surgeries and major joint arthroplasties in Asians ranges from 0.2% to 0.9% and 1.0% to 1.9%, respectively.1 There is a high variability in the method of studies and diagnostic modalities of VTE. These rates of VTE approach those in Western countries. However, perioperative VTE prophylactic practices are still suboptimal in Asia. Only half of the clinicians routinely use thromboprophylaxis in high-risk surgeries.44 The Caprini score, which is commonly used for assessment of thrombotic risk in surgical patients, has not been well validated in Asians. The Asian VTE guideline recommends that all surgical patients receive individual VTE risk assessment to ensure that all patients are given appropriate thromboprophylaxis.43 Thromboprophylaxis with anticoagulants or mechanical prophylaxis is recommended based on patients' risk of thrombosis and bleeding. Early mobilization is recommended in all surgical patients. Surveillance ultrasound in asymptomatic patients and prophylactic inferior vena cava filters should be avoided.
CLINICAL CASE 4 (Continued)
The patient was not initially placed on thromboprophylaxis due to severe thrombocytopenia related to sepsis. After the diagnosis of PE, therapeutic LMWH and platelet transfusion to keep his platelet count above 50 × 109/L were administered. Three days later, sepsis was controlled and his oxygenation improved. Individualized assessment of thrombotic and bleeding risks should be applied when deciding on thromboprophylaxis in hospitalized Asian patients.
Acknowledgments
We sincerely thank Professor Nigel Key (University of North Carolina at Chapel Hill, USA) for reviewing the manuscript and offering comments.
Conflict-of-interest disclosure
Kochawan Boonyawat: no competing financial interests to declare.
Pantep Angchaisuksiri: no competing financial interests to declare.
Off-label drug use
Kochawan Boonyawat: nothing to disclose.
Pantep Angchaisuksiri: nothing to disclose.