Abstract
Long-term survivors of pediatric hematologic malignancies are at elevated risk for neurocognitive impairment. Such impairment manifests in different ways at different times during survivorship, with deficits in processing speed, attention, and memory often appearing before deficits in executive function, intelligence, and academics. Survivors exposed to therapies that directly target the central nervous system (CNS), as is the case in acute lymphoblastic leukemia, may demonstrate subtle deficits during frontline therapy, and these deficits may grow and evolve over time. Survivors who do not receive CNS-directed therapies (eg, Hodgkin lymphoma) are also at elevated risk for neurocognitive impairment, although the influence on brain function is indirect through cancer therapy impact on systemic organ function vital to brain health (eg, cardiopulmonary morbidity). Over the course of the survivor's life span, the presence and impact of neurocognitive deficits will be determined by a complex interaction between premorbid development and environment, cancer therapy and clinical care, and posttreatment recovery and health. The timing and type of these treatment and health events will dictate the approach to screening and monitoring for neurocognitive impairment.
Learning Objectives
Identify the neurocognitive functions most often affected by cancer therapy in long-term survivors of pediatric acute lymphoblastic leukemia and Hodgkin lymphoma
Review direct and indirect risk factors associated with neurocognitive impairment in long-term survivors of pediatric acute lymphoblastic leukemia and Hodgkin lymphoma
Present recommendations for screening and monitoring of neurocognitive function in long-term survivors of pediatric acute lymphoblastic leukemia and Hodgkin lymphoma
Introduction
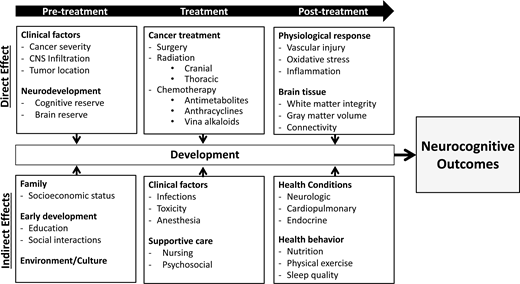
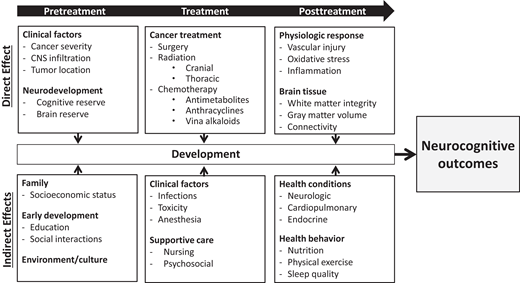
Neurocognitive impairment is a relatively common late effect in survivors of pediatric hematologic malignancies. Impairment manifests in different ways at different times during long-term survival due to a complex interaction between direct and indirect factors (Figure 1). This article defines types of neurocognitive impairment, discusses acute changes during frontline therapy, reviews disease-specific risk factors, and presents a model for screening and monitoring over the health span. Focus is placed on the 2 most common pediatric hematologic malignancies: acute lymphoblastic leukemia and Hodgkin lymphoma.
Visual abstract of common direct and indirect effects on neurocognitive development with onsets that occur prior to treatment, during treatment, and following treatment.
Visual abstract of common direct and indirect effects on neurocognitive development with onsets that occur prior to treatment, during treatment, and following treatment.
CLINICAL CASE
Lisa is a 22-year-old woman diagnosed with acute lymphoblastic leukemia, pre-B, at 3 years of age. She was treated on a standard-risk arm of a chemotherapy-only protocol and received high-dose intravenous methotrexate (cumulative doses of 11.5 g/m2) and intrathecal methotrexate (cumulative dose of 203 mg), in addition to doxorubicin, dexamethasone, cytarabine, vincristine, and L-asparaginase over 30 months of therapy. She developed subclinical osteonecrosis and leukoencephalopathy during therapy. During long-term survivorship, she experienced neuropathy and chronic pain, which limited her physical activity and was associated with frequent sleep disturbance. Family history is negative for cognitive, learning, or behavioral problems, and both parents have college degrees. Lisa is currently enrolled in community college.
Key questions include the following:
Is Lisa at risk for development of neurocognitive problems?
If so, what types of problems are likely to emerge?
What are the risk factors for her development of neurocognitive problems?
Characterization of neurocognitive impairment
Neurocognitive function refers to cognitive abilities that are associated with specific brain regions and/or neural networks. Assessment of such function provides insight into the relative health and integrity of the brain, which can predict brain development and future cognitive function. Neuropsychological testing is the primary method to assess these functions and involves the use of discrete tests that have well-established reliability and validity (Table 1), as well as age-referenced normative data, and can be linked to specific brain regions. Performance on a neuropsychological test leads to a norm-referenced standard score that can identify strengths and weaknesses of the individual in relation to the general population of similar age.
Domains and subdomains of neurocognitive function affected in long-term survivors of pediatric hematologic malignancies and cognitive functions encompassed by the domains
| Domain . | Subdomain . | Cognitive function . |
|---|---|---|
| Attention | Focused | Target selection |
| Sustained | Omissions and variability over time | |
| Shifting | Alternating focus | |
| Processing speed | Visual | Rapid detection |
| Motor | Rapid response | |
| Memory | Span | Immediate recall |
| Encoding | Storage for delayed recall | |
| Retrieval | Delayed recall | |
| Executive function | Working memory | Manipulating information in memory span |
| Fluency | Rapid generation of solutions | |
| Flexibility | Alternating response sets | |
| Planning and organization | Logical, sequential solution generation | |
| Global cognition | Verbal intelligence | Acquired knowledge |
| Spatial intelligence | Spatial judgment and visualization | |
| Academic | Reading | Decoding and comprehension |
| Mathematics | Calculation and problem solving | |
| Writing language | Spelling and composition |
| Domain . | Subdomain . | Cognitive function . |
|---|---|---|
| Attention | Focused | Target selection |
| Sustained | Omissions and variability over time | |
| Shifting | Alternating focus | |
| Processing speed | Visual | Rapid detection |
| Motor | Rapid response | |
| Memory | Span | Immediate recall |
| Encoding | Storage for delayed recall | |
| Retrieval | Delayed recall | |
| Executive function | Working memory | Manipulating information in memory span |
| Fluency | Rapid generation of solutions | |
| Flexibility | Alternating response sets | |
| Planning and organization | Logical, sequential solution generation | |
| Global cognition | Verbal intelligence | Acquired knowledge |
| Spatial intelligence | Spatial judgment and visualization | |
| Academic | Reading | Decoding and comprehension |
| Mathematics | Calculation and problem solving | |
| Writing language | Spelling and composition |
Increased specificity of neurocognitive function and linkage to brain health comes with specific measures of neurocognitive function rather than global measures of cognitive abilities. Specific measures include assessment of visual and motor processing speed, focused and sustained attention, memory encoding and retrieval, cognitive flexibility, and set-shifting, to name a few. Global measures of cognitive abilities include assessment of intelligence and academic skills. Assessment of these general abilities is often useful to predict educational and/or vocational success but is not particularly sensitive to change or useful at linkage to underlying neuropathology. General abilities are dependent on specific abilities, particularly over the course of brain development. For examine, injury to the hippocampus may not immediately affect vocabulary, but the resulting specific memory encoding deficit will limit the rate of new learning over time, and vocabulary performance will decline over many years in relation to rate of growth in age-matched unimpaired peers.1
Acute changes in pediatric hematologic malignancies
Neurocognitive functions affected during the acute phases of cancer therapy often include basic or foundational abilities, including processing speed, attention, and memory.2 Processing speed is heavily dependent on efficiency of neural network connectivity, which is substantially enhanced with integrity of brain myelin (ie, oligodendrocytes).3 White matter disease, leukoencephalopathy, is associated with cranial irradiation and intrathecal methotrexate.4 This leukoencephalopathy may be a consequence of direct injury to the oligodendrocytes, injury to the underlying axons, or injury to the microvascular supply to either oligodendrocytes or axons. The end result is disruption of communication along axonal pathways, often reflected through slowed processing speed. Attention is often mistakenly referred to as a single entity when, in fact, it comprises multiple cognitive skills. Focused attention involves the ability to filter distractions while attending to a specific target of interest. Sustained attention, on the other hand, involves attending to a single stream of information over time. Since sustained attention is more heavily time based, it is highly correlated to processing speed (ie, the faster the processing speed, the less time one needs to sustain effort to process the information). As such, sustained attention also appears to be affected by white matter integrity and efficiency of neural connectivity.5 Memory functions can often be segmented in 3 primary components of span, encoding, and retrieval. Span refers to a buffer for immediate recall of information that may not necessarily be encoded. Encoding involves the conversion of information from memory span into a memory engram (storage), which can be retrieved at a later date. This process of encoding requires structures in the medial temporal lobe, including the hippocampus and fornix, while new memories are stored in dispersed cortical regions, particularly in frontal and parietal nonsensory and nonmotor areas. The medial temporal lobe structures are supported by a rich microvascular network, which appears particularly sensitive to radiation exposure.6 The hippocampus itself also has a higher density of glucocorticoid receptors compared with many other regions of the brain,7 which may make it vulnerable to excessive levels of corticosteroids.
Chronic effects in pediatric hematologic malignancies
Chronic effects of cancer and cancer therapy on neurocognitive function tend to involve disruption of neural activity/connectivity,3 which prove more difficult, but not impossible, from which to recover. In addition to neuronal structures involved in memory function, abilities such as executive functions and intellectual, academic, and social attainment tend to be heavily dependent on complex neural network connectivity. Executive function involves processes such as flexibility and fluency, reasoning and problem solving, and organization and planning. These functions involve multiple integrated neural networks and are prone to disruption in multiple localized regions in the dorsolateral prefrontal and anterior frontal lobes, lateral and medical parietal lobes, and lateral temporal lobes.8 Executive functions are often dependent on efficiency in the integration of these networks and, thus, can also be affected by diffuse white matter injury. Intellectual function involves the integration of executive functions with prior learning and experiences such as vocabulary and general knowledge and facts. Academic functions generally reflect an interaction between executive function and intellectual abilities, with environmental exposures and resources, both formal (school) and informal (home environmental and community resources). Social attainment often refers to the level of educational or vocational attainment during young adulthood and frequently predicts future adult function and success. In the general population, social attainment is heavily influenced by community and family resources as well as intellectual potential. From the perspective of pediatric hematologic disease, social attainment is also strongly influenced by acute and chronic neurotoxicity, which, as pointed out above, can affect attention and memory skills that influence problem solving and academic skills, leading to lower educational performance when uncorrected.9
Disease-specific risk factors
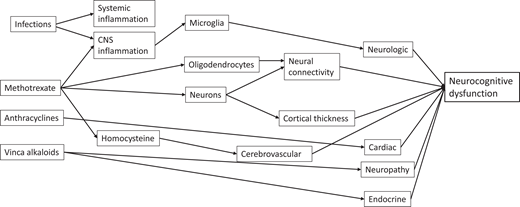
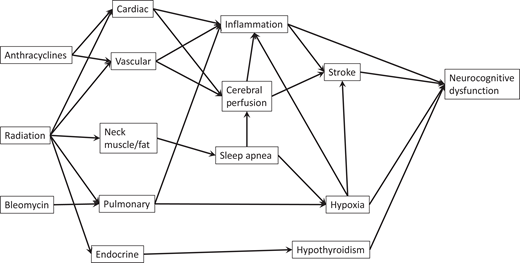
Risk factors for neurocognitive impairment in pediatric hematologic malignancies are generally associated with specific treatments, which are driven by specific diagnoses. Neurocognitive impairment in survivors of acute lymphoblastic leukemia (ALL) is associated with direct effects of neurotoxic therapies and indirect effects of therapy on systemic organ dysfunction (Figure 2),10 while neurocognitive impairment in survivors of Hodgkin lymphoma (HL) is typically associated only with the indirect effects of therapy on systemic organ dysfunction (Figure 3).11
Schema of common contributions and pathways from treatment to neurocognitive outcome in survivors of acute lymphoblastic leukemia treated on chemotherapy-only protocols. Chemotherapy agents affect vascular and central nervous system neurons and glia, which influence brain development. Neurocognitive dysfunction results from altered brain development as well as contributions from chronic health conditions.
Schema of common contributions and pathways from treatment to neurocognitive outcome in survivors of acute lymphoblastic leukemia treated on chemotherapy-only protocols. Chemotherapy agents affect vascular and central nervous system neurons and glia, which influence brain development. Neurocognitive dysfunction results from altered brain development as well as contributions from chronic health conditions.
Schema of common contributions and pathways from treatment to neurocognitive outcome in survivors of Hodgkin lymphoma. Radiation and chemotherapy treatment affects cardiac, pulmonary, and endocrine function, as well as vascular and muscle development. This impact, in turn, influences cerebrovascular perfusion, which can result in neurocognitive dysfunction.
Schema of common contributions and pathways from treatment to neurocognitive outcome in survivors of Hodgkin lymphoma. Radiation and chemotherapy treatment affects cardiac, pulmonary, and endocrine function, as well as vascular and muscle development. This impact, in turn, influences cerebrovascular perfusion, which can result in neurocognitive dysfunction.
Direct neurotoxicity
Cranial irradiation was a common approach for prophylactic treatment of the central nervous system (CNS) to prevent secondary relapse in ALL. The radiation involved whole-brain exposure at doses of 24 then 18 Gy, which were identified to affect multiple cognitive abilities, including processing speed, attention, memory, executive functions, intellect, and academics.12 The impact of treatment often occurred early in brain development and was demonstrated to limit growth of multiple brain regions and connectivity.13 Fortunately, cranial irradiation is now used infrequently for ALL, occurring at lower cumulative doses when used. It has been replaced in most circumstances by intrathecal methotrexate chemotherapy; methotrexate is also now given through high-dose intravenous injections. Intrathecal and high-dose intravenous methotrexate appears to have a more focused impact on white matter integrity and less of an impact on the integrity of brain cortical regions.14 However, at this time, it is unclear whether the white matter changes are due to direct injury of the oligodendrocytes or reflect the oligodendrocyte response to injury in the underlying axon of the neuron. Nonfebrile seizures and cerebrovascular stroke can occur during frontline therapy for pediatric hematologic malignancies and further affect neurocognitive function.15,16 The impact from these events is in addition to the risks associated with treatment exposures discussed above. It has been reported that severe infection and sepsis confer additional risk for neurocognitive impairment on top of the known risk associated with CNS treatment.17 As many inflammatory cytokines can readily cross the blood-brain barrier, severe systemic inflammation may contribute to the onset of neuroinflammation, a process known to be associated with cognitive impairment in the general aging population.18 General anesthesia has also recently been demonstrated to be associated with brain white matter injury and processing speed deficits in ALL survivors.19 General anesthesia is a risk factor for cognitive impairment in the general population for children under 3 years of age,20 and when added to the neurotoxic impacts from specific cancer therapy, the consequences may be particularly troublesome in ALL survivors who are often treated at a young age.
Indirect effects of systemic disease
Roughly 95% of long-term survivors of childhood cancer develop chronic health conditions, and 80% experience serious or life-threatening conditions.21 These conditions often develop over many years of adult survivorship and appear directly related to prior cancer and/or cancer therapy. Once they develop, chronic health conditions can independently increase risk for neurocognitive deficits.22 Many long-term ALL and HL survivors develop sensory and motor neuropathy, frequently associated with use of vinca alkaloid chemotherapy agents.23 Neuropathy is associated with increased symptoms of pain, which itself is associated with neurocognitive impairment likely through physiologic mechanisms of systemic and central inflammation.24 Neuropathy and pain are also related to lower physical activity, and higher consistent physical activity has been demonstrated to improve long-term cognitive function.25
Elevated risk for cardiopulmonary dysfunction is seen in survivors of ALL and HL due primarily to anthracycline exposure in the former and anthracyclines and thoracic radiation in the latter.26 In the general population, cardiopulmonary disease is associated with neurocognitive impairment, including attention and memory deficits.27 Attention and memory problems occur at a higher frequency in long-term survivors of HL compared with siblings and community controls, and these problems are related to cardiac and pulmonary morbidity.11,28 The threshold for impact from cardiac and pulmonary morbidity may be lower in survivors with prior direct neurotoxicity.22 In addition, the effects of cardiac and pulmonary toxic therapies may lower the threshold for cognitive impact from other factors, such as smoking and systemic inflammation.11 Long-term survivors of HL have been demonstrated to be at elevated risk for overt ischemic stroke, with a roughly 4-fold higher risk than sibling controls.29 Although the specific etiology of the stroke is still under investigation (eg, hypertension vs radiation-induced vascular disease vs obstructive sleep apnea), the occurrence of stroke does increase risk for neurocognitive impairment in long-term survivors.
Sleep disturbances are also associated with neurocognitive impairment. Long-term survivors of ALL who also demonstrate insomnia have higher risk for neurocognitive impairment compared with ALL survivors without insomnia.30 This observation may be associated with lowered cognitive reserve associated with altered brain development. Long-term survivors of HL are at elevated risk for obstructive sleep apnea. In fact, we have recently presented preliminary data from an ongoing study that suggest roughly 50% of HL survivors treated with thoracic radiation develop clinically significant obstructive sleep apnea.31 In the general population, obstructive sleep apnea increases the risk for cardiomyopathy and cerebrovascular accidents.32
It has been well known for many decades years that socioeconomic factors, including parent education and income, are associated with cognitive development in the general population. There has been renewed interest in these factors in cancer survivors as well. Although it is highly likely that cancer survivors also experience impact from limited socioeconomic resources, similar to children in the general population, at least 2 factors unique to cancer survivors may cause them to experience a stronger impact from limited resources. The first deals with the concept of cognitive and brain reserve. Limited socioeconomic factors such as poor early childhood nutrition, education, and environmental stimulation could limit development of brain and cognitive reserve, such that CNS-directed cancer therapy could have a stronger impact on neurocognitive outcomes. Although this point is currently theoretical, it has recently been demonstrated that reduced cognitive and brain reserve from early CNS-directed cancer therapy is associated with higher risk for neurocognitive impairment following the onset of chronic health conditions in long-term survivors.22 The second potentially unique interaction with socioeconomic factors in childhood cancer survivors centers on limited resources for recovery and rehabilitation. As noted above, following cancer diagnosis and therapy, many survivors experience acute cognitive and behavioral impacts. These impacts could benefit from enhanced cognitive, behavioral, and physical stimulation. Such stimulation will not only directly facilitate cognitive growth but also facilitate recovery of biological mechanisms that may interfere with cognitive function. For example, proper nutrition and physical activity reduce systemic inflammation and oxidative stress while enhancing metabolic function.33 Cancer survivors who have a lower family income, have limited educational resources, and reside in “food deserts” or in a neighborhood with limited greenspace or “safe spaces” will be at significant disadvantage in achieving proper nutrition, physical activity, and cognitive stimulation to promote such recovery.
Screening and monitoring neurocognitive outcomes
Assessment for neurocognitive impairment in survivors of pediatric hematologic malignancies can be broken down into initial screening and long-term monitoring schedules.
According to current Long-term Follow-up Guidelines of the Children's Oncology Group (COG), survivors treated with cranial irradiation, intrathecal methotrexate, or high-dose intravenous methotrexate or cytarabine should undergo neurocognitive assessment 5 years postdiagnosis or 2 years following the end of therapy.34 In addition, survivors who do not have a treatment history consistent with these current COG guidelines should undergo comprehensive neurocognitive assessment if they develop any Common Terminology Criteria for Adverse Event Grade 2 (moderate, intervention indicated or limiting age- appropriate instrumental activities of daily living)35 or higher chronic health condition identified as being associated with cognitive impairment, including cardiac disease, pulmonary disease, metabolic dysfunction, hypothyroidism, neuropathy, stroke, or persistent sleep disturbance. A revision to the COG guidelines is currently being released that will add neurocognitive assessment for survivors who develop these health conditions. Based on the discussion above, it would also be prudent to conduct comprehensive assessment of survivors who develop acute neurotoxicity, including leukoencephalopathy or nonfebrile seizures, regardless of whether these conditions continue into long-term survivorship. The initial assessment should include neuropsychological testing of processing speed, attention, memory, executive function, and intellectual and academic abilities. Testing should include objective performance-based measures and parent- or patient-reported outcomes.
Those survivors who do not demonstrate problems on the comprehensive assessment should then undergo regular monitoring of neurocognitive function on an annual basis.36 This is typically accomplished though parent/patient report of academic/vocational problems or specific symptoms. Recent research demonstrates that survivors can develop new onset of neurocognitive problems more than 10 years after diagnosis.37 As such, some survivors may need comprehensive assessments in the future, even if their initial assessment reveals no problems.
Survivors who do demonstrate neurocognitive impairment on initial testing should undergo comprehensive reevaluations every 3 to 5 years. Given that younger survivors develop more rapidly, shorter intervals may be required for them. Neurocognitive problems appear to be persistent over time and may actually worsen as a survivors age. Reassessment of cognitive status may help identify those in need of early interventions to prevent further decline.
The schedule of neurocognitive assessment outlined above will assist not only with identifying those survivors in need of neurocognitive interventions for academic problems but also those who are struggling with vocational endeavors. Neurocognitive problems have been identified as a source of unemployment in adult survivors of childhood cancer.38 As such, neurocognitive monitoring should not be limited to children and adolescents but also adults throughout the life span.
CLINICAL CASE (Continued)
Addressing the questions:
Is Lisa at risk for development of neurocognitive problems?
If so, what types of problems are likely to emerge?
What are the risk factors for her development of neurocognitive problems?
Despite the fact that Lisa comes from a high-functioning environment, she has several risk factors for the development of neurocognitive problems, including being treated with intrathecal and high-dose intravenous methotrexate, as well as developing neuropathy, chronic pain, and frequent sleep disturbance. Per COG guidelines, she underwent neurocognitive testing at 8 years of age when she entered long-term follow-up. Lisa demonstrated problems in attention and processing speed, which were addressed with classroom accommodations in school. She was diagnosed in her community as having attention-deficit/hyperactivity disorder, which was treated with Concerta (ie, methylphenidate), followed by Focalin (ie, dexmethylphenidate) and then Adderall (ie, amphetamine and dextroamphetamine). At 12 years postdiagnosis, Lisa began demonstrating deficits in memory and executive function, despite continued treatment with Adderall.
Conflict-of-interest disclosure
Kevin R. Krull: no competing financial interests to declare.
Off-label drug use
Kevin R. Krull: nothing to disclose.