Abstract
The diagnosis and management of the BCR-ABL–negative myeloproliferative disorders (MPDs) of polycythemia vera (PV), essential thrombocythemia (ET), and primary myelofibrosis (PMF) are at an explosive crossroads of scientific investigation and evolving paradigms since the discovery of the tyrosine kinase–activating JAK2V617F mutation in 2005. Additional discovery of relevant molecular lesions (JAK2 exon 12 mutations and c-MplW515L/K) have only further enriched our understanding of MPD pathogenesis. The improved diagnostic certainty these molecular markers provide have resulted in the modification, and simplification, of the World Health Organization (WHO) diagnostic algorithms for MPDs. Despite these scientific advances, however, the initial management of MPDs continues to rely upon a risk-based strategy to minimize the risk of vascular events with control of erythrocytosis, targeted antiplatelet therapy, and risk-based myelosuppressive therapy. No current medical therapy has altered the natural trend of the MPDs to lead to overt severe myelofibrosis or acute leukemia. Investigations into targeted therapies for MPDs are proceeding at a brisk pace with agents aimed at immunomodulation, decreasing marrow stromal reaction to the aberrant clone, DNA hypomethylation, or the inhibition of tyrosine kinases. Specific inhibition of JAK2 itself appears promising by in vitro investigations, and clinical trials with multiple agents are planned to commence enrollment in 2007. The potential impact of JAK2 inhibitors on the manifestations of the MPDs is unclear, but is awaited with great interest.
From Dameshek to WHO: What Constitutes an MPD Today?
The BCR-ABL–negative chronic myeloproliferative disorders (MPDs), first described by William Dameshek in 1951,1 are currently in a period of rapid discovery regarding their pathogenetic mechanisms. This period of rapid improvement of mechanistic understanding is likewise leading to similar changes in diagnostic criteria and hopefully improved targeted therapies. The MPDs have classically included the disorders of polycythemia vera (PV), essential thrombocythemia (ET), and primary myelofibrosis (PMF), yet even our preconceived understanding of the diagnostic and therapeutic differences between these disorders are evolving rapidly. This manuscript will try to outline the effect the evolving understanding of MPD pathogenesis is having the clinical care of patients with MPD.
The watershed moment for MPDs occurred in 2005 with the heavily publicized discovery of the JAK2V617F mutation.2–5 This point mutation, in the pseudokinase domain of JAK2 (a key component of the cell growth and differentiation JAK-STAT pathway), leads to constitutive activation of the pathway. This mutation joined the pantheon of constitutively active tyrosine kinases identified as playing a role in myeloid neoplasms, including BCR-ABL in chronic myeloid leukemia, FIP1L1-PDGFRA for chronic eosinophilic leukemia and systemic mastocytosis, and KITD816V for systemic mastocytosis, among many others.6 The impact has been such that a search of PubMed for the 24 months prior to the JAK2V617F discovery reveals 520 manuscripts for “myeloproliferative disorder” and 380 manuscripts for “JAK2,” whereas 715 and 682 manuscripts were identified in the subsequent 24 months for myeloproliferative disorder and JAK2, respectively. This flurry of investigative activity has lead to the discovery of additional genetic mutations with potential pathogenetic implications including the c-MplW515L/K (in 5% of PMF and 1% of ET)7 and alternative mutations in the exon 12 of JAK2 in some of those patients with PV previously identified as wild type for JAK2.8 So, what is the effect of our improved understanding of MPD biology on the diagnostic process?
The diagnosis of the BCR-ABL–negative MPDs has always been limited by the absence of a gold standard, an absolute molecular marker. This latter deficiency has led to a series of clinico-pathologic diagnostic criteria relying upon features helpful in distinguishing an MPD from (1) a reactive state; (2) an alternative myeloid malignancy; and (3) an alternative MPD diagnosis. These criteria usually were the easiest to apply to overt MPD cases, but not uncommonly would leave others with uncertainty. The World Health Organization (WHO) has taken a lead role in diagnostic criteria for MPDs, and the current WHO criteria9 for PV, ET, and PMF are undergoing a revision10 to incorporate the diagnostic implications of the new wave of mutations (such as the JAK2V617F) (Figure 1 ).
Polycythemia vera
PV is the MPD in which the presence of the JAK2V617F is of greatest diagnostic importance because it is seen well in excess of 90% of afflicted individuals.2–5 Many of the patients who clinically have PV yet have wild-type JAK2 may have an alternative mutation that similarly activates the JAK-STAT pathway, such as mutations in the exon 12 of the JAK2 gene. In aggregate, these described mutations are present in 98% of PV and not in secondary forms of erythrocytosis.
The current WHO diagnostic criteria for PV have been updated with proposed criteria (Figure 1 ) that establish the diagnosis of PV by both the presence of clear erythrocytosis or increased red cell mass and the presence of a known PV molecular lesion (JAK2V617F or JAK2 exon 12 mutation).10 If both the latter features are present, a diagnosis of PV is highly likely and can be confirmed by the presence of one of the minor criteria, such as bone marrow biopsy consistent with PV (hypercellularity and panmyelosis with prominent trilineage proliferation). In the rare circumstance of patients with PV lacking the known PV molecular lesion, the diagnosis can still be established if two of the minor criteria are reached. The updated WHO criteria have the practical advantage of greatly simplifying the diagnosis of those with erythrocytosis who are JAK2V167F- positive who are highly likely to have PV.
Essential thrombocythemia
The negative predictive value of a wild-type JAK2V617F mutation is significantly more limited in ET, given that only about 50% of afflicted individuals express the mutation;2,3,5 however, its presence is diagnostically helpful. In the revised WHO criteria for ET10 (Figure 2 ), sustained unexplained thrombocytosis has been lowered from 600 × 109/L to any sustained value greater than normal (> 450 × 109/L) given the fact that many patients with ET, even with thrombosis, can present with platelet counts between 450 and 600 × 109/L. Second, if the JAK2V617F is present (or another marker of clonality by karyotype is met), the burden of clinical investigations to exclude secondary causes is diminished. The need to exclude other potential myeloid disorders, and bone marrow morphology (proliferation of the megakaryocytic lineage) with increased numbers of enlarged, mature megakaryocytes (without significant increases in other myeloid lineages) consistent with ET remains largely unchanged.
Primary myelofibrosis
PMF has been known by a wide range of synonyms, including chronic idiopathic myelofibrosis, agnogenic myeloid metaplasia, and myelofibrosis with myeloid metaplasia. Given that the disorder is neither idiopathic nor always accompanied by myeloid metaplasia, the International Working Group for Myelofibrosis Research and Treatment (IWG-MRT; an international ad hoc collaborative group of more than 40 dedicated myelofibrosis and MPD experts) reached the consensus that PMF would be the most accurate and appropriate diagnostic term.11 PMF is the term used for patients who present with de novo disease; patients who progress to a myelofibrotic stage from previous PV or ET are designated post-PV myelofibrosis (post-PV MF) and post-ET myelofibrosis (post-ET MF), respectively.11
The proposed new WHO criteria10 attempt to bridge the spectrum across the phenotypic variability in the disorder by requiring that three main features must be present to diagnose PMF (Figure 1 ):
Bone marrow histologic changes consistent with the disorder, specifically the presence of megakaryocyte proliferation and atypia (small to large megakaryocytes with an aberrant nuclear cytoplasmic ratio and hyperchromatic, bulbous, or irregularly folded nuclei and dense clustering), which are usually accompanied by either reticulin and/or collagen fibrosis. However, in the absence of significant reticulin fibrosis, the megakaryocyte changes must be accompanied by an increased bone marrow cellularity characterized by granulocytic proliferation and often decreased erythropoiesis (this substitutes for the previous pre-fibrotic/cellular-phase disease).
Absence of criteria suggesting an alternative myeloid disorder.
Either a marker of clonality (such as JAK2V617F or c-MPLW515L/K) or, if such a clonal marker is absent, no evidence of the fibrosis being related to an inflammatory or reactive state. Two out of four minor criteria are required to secure the diagnosis of PMF, including peripheral blood manifestations (anemia, leukoerythroblastosis, or increased lactate dehydrogenase) or splenomegaly (presumably from extramedullary hematopoiesis).
Although the updated WHO diagnostic criteria should provide a simplified and clearer diagnostic algorithm (especially in those with a clear MPD clonal molecular marker), further evolution of diagnostic criteria can be anticipated in the future. Indeed, as the biological underpinnings of the MPDs become further elucidated, we may be able to simplify these criteria further with less reliance on subjective clinical features or histologic interpretation of marrow trephines.
Does Improved Pathogenetic Understanding Equal Better Therapies for MPDs?
Current therapy of MPDs: an overview
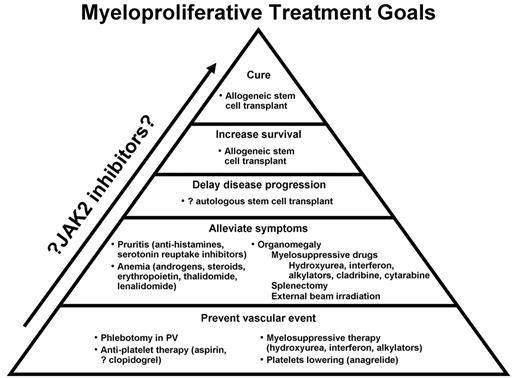
The natural history of MPDs has a variable period of risk of vascular events and a long-term risk of transformation to either an overt myelofibrotic phase or death. Current available therapies have rarely been able to impact this natural history beyond palliating symptoms or decreasing the risk of vascular events (Figure 2 ). Given these challenges, how should patients with MPD be optimally managed? Currently, incorporation of the modest numbers of randomized clinical trials, larger numbers of nonrandomized phase 2 trials, and clinical judgment all need to be considered in developing a therapeutic algorithm for the MPDs (Figure 3 ). Therapeutic algorithms for the MPDs will continue to evolve as therapeutic modalities improve and are vetted by appropriate clinical trials.
After the appropriate diagnosis of an MPD is established, or sometimes even suspected, patients need to be stabilized for immediate coagulopathies from severe erythrocytosis, thrombocytosis, or concurrent or pre-existing thrombotic events. Management decisions will then partially flow from the clinician’s estimation of overall disease prognosis and the separate estimation of the risk of vascular events (Figure 3 ). Patients with ET and PV are defined as high-risk when they have either had a prior vascular event or are older than 60 years of age; low-risk patients meet neither of these criteria (and have platelet counts < 1000 × 109/L). Intermediate-risk ET and PV lack these prior features but have cardiovascular risk factors. Newly identified potential vascular risk factors include leukocytosis at diagnosis (at least in PV; >15 × 109/L12) or high JAK2V617F mutation allele burden.13 Whether these new factors should be included in modeling MPD vascular risk is not yet known, and requires further study. Overall prognostic models for survival are best established in PMF, in which the Lille criteria14 (based on anemia or marked leukocytosis/leukopenia) and subsequent complete blood count score (the Lille criteria with further stratification if thrombocytopenia present) have been the most clinically relevant.15
Short-term plan
The immediate therapeutic concerns for patients with MPD at presentation are both an adequate prophylaxis against vascular events and palliation when possible of MPD symptomatology. Available therapies for both ET and PV, up this juncture, have only been successful in decreasing the risks of thrombotic or hemorrhagic (i.e., vascular) events. Management of patients with PV includes control of erythrocytosis (by phlebotomy) and, when no contraindication exists, the use of low-dose aspirin as validated by the ECLAP study (European Collaborative Low-Dose Aspirin Trial).16 The degree to which a patient needs to be phlebotomized has been questioned, with traditional dogma suggesting a goal hematocrit of less than 42% for women and 45% for men. Recent retrospective analysis of vascular events of patients on the ECLAP trial has suggested that modestly higher targets (perhaps up to hematocrits of 55%) may not increase the risk of vascular events.17 Whether hematocrit goals should be changed for PV is a question that should be addressed by appropriately designed trials.
What about myelosuppressive therapy for managing the MPDs? Hydroxyurea was shown in a randomized fashion to aid in the prevention of thrombotic events in patients with high-risk ET.18 The UK MRC (United Kingdom Medical Research Council) PT-1 (primary thrombocythemia-1) trial compared in a randomized fashion hydroxyurea and anagrelide (both along with low-dose aspirin) for patients with ET and found hydroxyurea plus aspirin to be superior in regards to preventing arterial events, hemorrhage, and transformation to post-ET MF.19 Similar randomized data for the use of hydroxyurea or other myelosuppressive agent in high-risk PV do not yet exist; however, in the absence of such data, it remains the most commonly used agent in practice.20 Therefore, hydroxyurea is the standard front-line therapy for high-risk patients with ET and PV (based on clinical experience) who require platelet-lowering therapy. Although concerns linger as to whether hydroxyurea accelerates an MPD towards leukemic transformation, this has never been proven when hydroxyurea is used as a single agent.21 The use of pegylated IFN-α 2A has shown intriguing activity, and potentially improved tolerability, over traditional IFN, especially for PV (Table 1 ).22 How IFN compares with hydroxyurea for control of vascular events has not yet been studied in a randomized fashion.
Palliating symptoms in patients with MPD can include therapies for pruritus (antihistamines and selective serotonin reuptake inhibitors), erythromelalgia (aspirin), and fatigue (no clear therapy has been proven efficacious, but exercise may help as it has in other malignancies23) (Figures 2 and 3 ). Cytopenias have improved in subsets of patients with erythropoietin supplementation,24 androgens,25 and/or corticosteroids. Similarly, the use of nonspecific myelosuppressive regimens such as oral hydroxyurea26 and cladribine27 have all been reported to provide palliative reduction in painful splenomegaly.
Long-term therapeutic plan
Currently, no therapy has been shown to be curative, to alter natural history, or to prolong survival in patients with MPD, with the exception of allogeneic stem cell transplantation. The long-term therapeutic plan for patients with MPD, and particularly those with PMF (and post-ET/PV MF), can be divided into observation, proceeding directly to an allogeneic stem cell transplant, and enrollment in an appropriate clinical trial. Observation as a medical plan implies continued vigilance and therapy for prevention of vascular events and appropriate therapy for palliation of MPD symptoms. Observation is most appropriate for those patients with low-risk PMF, and controlled ET and PV. In addition, observation requires continued vigilance of the patient’s disease status for disease progression to a point where a clinical trial would be appropriate or a stem cell transplantation would be considered.
The choice and role of allogeneic stem cell transplantation for patients with MPD remains an evolving question. Among the MPDs, allogeneic stem cell transplantation is most attractive for high-risk PMF, given that this MPD is the most likely to decrease survival among those afflicted. Recent reports describe a 58% 3-year survival in a group of 56 patients with PMF (and post-ET/PV MF) (age 10–66), with a 32% nonrelapse mortality rate.28 The significant toxicity of full allogeneic transplantation in PMF led to exploration of the use of reduced-intensity conditioning trials.29 The latter trials have been encouraging in terms of decreased nonrelapse mortality and increased age range of those who underwent transplantation successfully. However, allogeneic transplant still carries a significant risk of graft-versus-host disease (at least 33%), and the exact role and benefit depends on the long-term prognosis of the patient. The significant risks of any of the stem cell transplantation procedures make it difficult to justify this therapy for ET and PV given the overall good prognosis of these patients.
Clinical Trials for the MPDs: Current and Future
Immunomodulation and targeting the stroma
The group of immunomodulatory cytokine inhibitory and anti-angiogenic agents collectively known as IMIDs have shown promise in the MPDs, and most specifically in PMF and post-ET/PV MF. Initial pilot studies with thalidomide in PMF were dose escalating in nature, beginning at doses of 100 mg/day.30 Subsequent low-dose (50 mg/day) thalidomide with a prednisone taper31 resulted in significant responses for anemia (67%), thrombocytopenia (75%), and splenomegaly (33%) without demonstrating, however, any definitive improvement in marrow or karyotypic abnormalities. Subsequently, lenalidomide (a second-generation, more potent cytokine-inhibitory IMID) was been evaluated in 68 patients with symptomatic PMF, with overall response rates of 22% for anemia, 33% for splenomegaly, and 50% for thrombocytopenia;32 however, improved marrow histology is seen in small number of the responders (4 of the 68 enrolled). Mirroring the activity of lenalidomide in del(5q) myelodysplastic syndrome, the small number of patients with PMF with an abnormality of chromosome 5 have the potential for significant response.33 Given the promising results obtained with lenalidomide, a randomized, placebo-controlled, international clinical study to determine the activity of pomalidomide (20,000-fold more potent than thalidomide in inhibiting TNF-α ) with or without a prednisone taper in PMF and post-ET/PV MF is currently under way. Multiple other attempts at targeting the bone marrow stromal reaction in PMF (post-ET/PV MF), angiogenesis or DNA hypermethylation are underway in a series of ongoing trials (Table 1 ).
The next generation of targeted therapy for PMF will move beyond agents targeting the stromal reaction, or cytokines, to agents aimed at the aberrant clone and constitutively active proliferative stimuli. Tyrosine kinase inhibitors have been of great benefit to patients when a molecular target exists (e.g., imatinib mesylate and chronic myeloid leukemia). Attempts to use current tyrosine kinase inhibitors in MPDs have been modest,34 while other studies in PMF have shown activity with thrombocytopenia35 but potentially with severe toxicity,36 and trials investigating second generation agents are ongoing (Table 1 ).
JAK2 inhibitors
Although the currently identified molecular defects in patients with MPD do not yet fully explain many issues of MPD pathogenesis, they provide an exciting and hopefully more fruitful therapeutic target. There have already been multiple reports of agents in development that have demonstrated the ability to inhibit the aberrant JAK2V617F, along with the wild-type JAK2, such as TG101209,37 Go6976,38 erlotinib,39 MK0457,40 and CEP-701.41 Intriguingly, in primary cells from patients with wild-type JAK2 who have the c-MplW515L/K, growth inhibition can similarly be accomplished by JAK2 inhibitors such as TG 101209.37 These latter observations suggest the possibility that even in patients with JAK2 wild-type MPD, a growth dependence on the JAK-STAT pathway may exist, and agents targeting this pathway may be active regardless of the JAK2 mutation status. This hypothesis is further supported by the continual discovery of aberrations in this pathway, as in exon 12 of the JAK2 gene in patients with JAK2V617F-negative PV.8
What effects can we expect to observe from the inhibition of JAK2 (no medication is likely to strictly inhibit the JAK2V617F)? Will inhibition of the JAK-STAT pathway decrease myeloproliferation (Figure 1 )? Will JAK-STAT inhibition decrease the development of thrombo-hemorrhagic events, given the multifactorial nature of their origin? What about the major therapeutic endpoints desired by clinicians and patients, namely delaying or preventing disease progression, or increasing survival? Uncertainty exists as to whether the inhibition of JAK2 will accomplish these goals, since the exact role of the JAK2V617F mutation in disease progression or development of blast-phase PMF remains unclear. The observation that patients with JAK2-mutant MPD have the potential to develop acute leukemia from a JAK2 wild-type clone42 questions the role of this mutation in disease progression. Therefore, what effect JAK2 inhibition will have on disease progression is quite uncertain and will require close, long-term monitoring of patients taking JAK2 inhibitors to be certain no adverse impact arises from the use of these agents. Finally, if beneficial, will the JAK2 inhibitors lead to the cure? Although unlikely at this juncture, efficacy in short-and long-term control of the disease would be greatly welcomed by physician and patient alike.
Investigational medical therapies for the BCR-ABL–negative myeloproliferative disorders.
| Disease . | Agent . | Class/type of drug . | Route . | Phase . | Reference . |
|---|---|---|---|---|---|
| Abbreviations: PV, polycythemia vera; ET, essential thrombocythemia; PMF, primary myelofibrosis; MF, myelofibrosis; IV, intravenous; SQ, subcutaneous; TGF, tumor growth factor; VEGF, vascular endothelial growth factor | |||||
| Immunomodulatory agents | |||||
| PV/ET | Pegylated interferon-2a | Immunomodulatory agent | SQ | 2 | 22 |
| PMF/post-ET/PV MF | Lenalidomide + prednisone | Immunomodulatory agent | Oral | 2 | 43 |
| PMF/post-ET/PV MF | CC-4047 ± prednisone | Immunomodulatory agent | Oral | 2 | Ongoing |
| Targeting the stromal reaction | |||||
| PMF/post-ET/PV MF | GC-1008 | Pan-specific human | IV | 2 | 44 |
| anti–TGF-β antibody | |||||
| PMF/post-ET/PV MF | Bevacizumab | Anti-VEGF monoclonal antibody | IV | 2 | 45 |
| DNA hypomethylating agents | |||||
| PMF/post-ET/PV MF | Azacitidine | Hypomethylating agent | SQ | 2 | Ongoing |
| PMF/post-ET/PV MF | Decitabine | Hypomethylating agent | IV | 2 | Ongoing |
| Targeting apoptosis agents | |||||
| PMF/post-ET/PV MF | Bortezomib | Proteasome inhibitor | IV | 2 | 46 |
| Kinase inhibitory agents | |||||
| PMF/post-ET/PV MF | Dasatinib | Kinase inhibitor | Oral | 2 | 47 |
| JAK2 inhibitors in development | |||||
| PMF/post-ET/PV MF (at first) | TG 101209 | JAK2 inhibitor | Oral | 1/2 | 37 |
| PMF/post-ET/PV MF (at first) | Go6976 | FLT3-JAK2 inhibitor | Unknown | Preclinical | 38 |
| PMF/post-ET/PV MF (at first) | Erlotinib | JAK2 inhibitor | Oral | 1/2 | 39 |
| PMF/post-ET/PV MF (at first) | MK 0457 | Aurora kinase inhibitor | IV | 1/2 | 40 |
| PMF/post-ET/PV MF (at first) | CEP-701 | FLT3-JAK2 inhibitor | Oral | 1/2 | 41 |
| Disease . | Agent . | Class/type of drug . | Route . | Phase . | Reference . |
|---|---|---|---|---|---|
| Abbreviations: PV, polycythemia vera; ET, essential thrombocythemia; PMF, primary myelofibrosis; MF, myelofibrosis; IV, intravenous; SQ, subcutaneous; TGF, tumor growth factor; VEGF, vascular endothelial growth factor | |||||
| Immunomodulatory agents | |||||
| PV/ET | Pegylated interferon-2a | Immunomodulatory agent | SQ | 2 | 22 |
| PMF/post-ET/PV MF | Lenalidomide + prednisone | Immunomodulatory agent | Oral | 2 | 43 |
| PMF/post-ET/PV MF | CC-4047 ± prednisone | Immunomodulatory agent | Oral | 2 | Ongoing |
| Targeting the stromal reaction | |||||
| PMF/post-ET/PV MF | GC-1008 | Pan-specific human | IV | 2 | 44 |
| anti–TGF-β antibody | |||||
| PMF/post-ET/PV MF | Bevacizumab | Anti-VEGF monoclonal antibody | IV | 2 | 45 |
| DNA hypomethylating agents | |||||
| PMF/post-ET/PV MF | Azacitidine | Hypomethylating agent | SQ | 2 | Ongoing |
| PMF/post-ET/PV MF | Decitabine | Hypomethylating agent | IV | 2 | Ongoing |
| Targeting apoptosis agents | |||||
| PMF/post-ET/PV MF | Bortezomib | Proteasome inhibitor | IV | 2 | 46 |
| Kinase inhibitory agents | |||||
| PMF/post-ET/PV MF | Dasatinib | Kinase inhibitor | Oral | 2 | 47 |
| JAK2 inhibitors in development | |||||
| PMF/post-ET/PV MF (at first) | TG 101209 | JAK2 inhibitor | Oral | 1/2 | 37 |
| PMF/post-ET/PV MF (at first) | Go6976 | FLT3-JAK2 inhibitor | Unknown | Preclinical | 38 |
| PMF/post-ET/PV MF (at first) | Erlotinib | JAK2 inhibitor | Oral | 1/2 | 39 |
| PMF/post-ET/PV MF (at first) | MK 0457 | Aurora kinase inhibitor | IV | 1/2 | 40 |
| PMF/post-ET/PV MF (at first) | CEP-701 | FLT3-JAK2 inhibitor | Oral | 1/2 | 41 |
Current9 and proposed10 World Health Organization diagnostic criteria for the myeloproliferative disorders of polycythemia vera (PV), essential thrombocythemia (ET), and primary myelofibrosis (PMF).
*Vardiman JW et al. WHO histological classification of chronic myeloproliferative diseases. In: Jaffe ES, Harris NL, Vardiman JW, eds. World Health Organization Classification of Tumors: Tumours of the Haematopoietic and Lymphoid Tissues. Lyon, France: International Agency for Research on Cancer (IARC) Press; 2001.
#Diagnostic bone marrow changes for each diagnosis discussed in text.
Current9 and proposed10 World Health Organization diagnostic criteria for the myeloproliferative disorders of polycythemia vera (PV), essential thrombocythemia (ET), and primary myelofibrosis (PMF).
*Vardiman JW et al. WHO histological classification of chronic myeloproliferative diseases. In: Jaffe ES, Harris NL, Vardiman JW, eds. World Health Organization Classification of Tumors: Tumours of the Haematopoietic and Lymphoid Tissues. Lyon, France: International Agency for Research on Cancer (IARC) Press; 2001.
#Diagnostic bone marrow changes for each diagnosis discussed in text.
Current available therapies for the myeloproliferative disorders and their overall impact upon the disease.
Current available therapies for the myeloproliferative disorders and their overall impact upon the disease.
Therapeutic algorithm: “How I treat the MPDs” for the chronic myeloproliferative disorders of polycythemia vera (PV), essential thrombocythemia (ET), and primary myelofibrosis (PMF).
Therapeutic algorithm: “How I treat the MPDs” for the chronic myeloproliferative disorders of polycythemia vera (PV), essential thrombocythemia (ET), and primary myelofibrosis (PMF).
Associate Professor of Medicine, Division of Hematology, Mayo Clinic; Rochester, MN US