1. Hematology-Oncology Fellow, Fred Hutchinson Cancer Research Center and University of Washington
2. Professor of Medicine (Hematology) Active Emeritus, Stanford University School of Medicine
More people in low- and middle-income countries die from cancer than from HIV, TB, and malaria combined, and two-thirds of the global cancer deaths occur in these nations.1, 2 Hematologic disorders contribute to a significant portion of these deaths, and, in fact, the incidence of non-Hodgkin lymphoma in most countries in Africa is two to five times higher than in the United States, according to the International Agency for Research on Cancer. Innovation is needed to address disparities in care that contribute to the observed major differences in survival in low- and middle-income countries when compared with resource-rich nations.
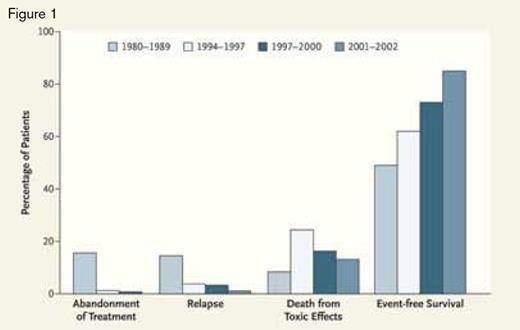
Frequency of treatment failure during the first year after diagnosis and two-year, event-free survival in pediatric ALL at the IMIP in Recife, Brazil, both before (1980-1989) and after (1994-2002) establishment of a twinning program.From The New England Journal of Medicine, Raul C. Ribeiro and Ching-Hon Pui, Saving the Children — Improving Childhood Cancer Treatment in Developing Countries, 352, 2159. Copyright © (2005) Massachusetts Medical Society. Reprinted with permission from Massachusetts Medical Society.
Frequency of treatment failure during the first year after diagnosis and two-year, event-free survival in pediatric ALL at the IMIP in Recife, Brazil, both before (1980-1989) and after (1994-2002) establishment of a twinning program.From The New England Journal of Medicine, Raul C. Ribeiro and Ching-Hon Pui, Saving the Children — Improving Childhood Cancer Treatment in Developing Countries, 352, 2159. Copyright © (2005) Massachusetts Medical Society. Reprinted with permission from Massachusetts Medical Society.
One model of intervention developed in response to this challenge involves collaborations between institutions in resource-abundant and resource-limited settings — referred to as “twinning.” St. Jude Children’s Research Hospital pioneered many of the approaches in this model as part of their International Outreach Program (IOP), which is currently active in 14 countries. One of their first twinning relationships was established with the Instituto Materno Infantil de Pernambuco (IMIP) in Recife, Brazil, where, in 1993, they helped establish standard treatment protocols for childhood acute lymphocytic leukemia (ALL). As seen in Figure 1, prior to the partnership, the event-free survival rate for children with ALL was less than 50 percent and eight years later was approaching that of resource-abundant nations at greater than 80 percent.3 With the goal of further improvement in outcome, the hospital in Recife has sustained those survival figures while treating about 80 cases of leukemia per year.4
An effective twinning collaboration such as this requires: 1) identifying people and institutions at both sites who are willing to make a long-term commitment to the process, 2) developing a long-term plan with regularly scheduled evaluations to enable necessary programmatic adjustments, 3) developing a cancer center of excellence with physicians and staff dedicated to oncologic care, and 4) enabling patient consultations between the two sites, usually through the use of Web-based conferencing, that involve physicians, nurses, pharmacists, and other clinic staff. Additional details on implementing twinning programs can be found in the online guide available on the St. Jude IOP website at www.stjude.org/internationalwww.stjude.org/international.5
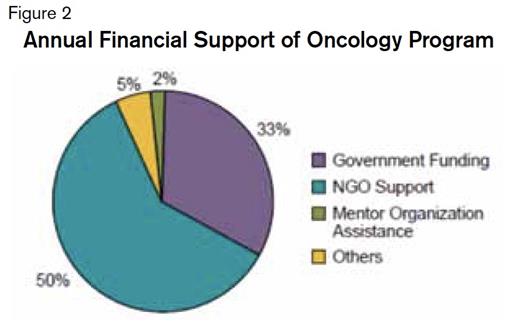
Distribution of annual financial support for an oncology program in a twinning initiative5.Pie chart used with permission from St. Jude Children’s Research Hospital.
Distribution of annual financial support for an oncology program in a twinning initiative5.Pie chart used with permission from St. Jude Children’s Research Hospital.
Funding for the entire IOP at St. Jude utilizes approximately 1 percent of the institution’s budget.6 Annual costs for each twinning program range from $200,000 to $300,000 for each of the first five years with the distribution of the cost responsibility shown in Figure 2, illustrating that nearly 90 percent of these costs are covered by government funding and support from non-governmental organizations (NGOs). Recent estimates suggesting that $131 billion could be saved globally each year through appropriate cancer care and prevention in low- and middle-income countries have made it more attractive for local governments and NGOs to invest in these programs. These projected savings result from the prevention of lost economic production associated with the morbidity and mortality of cancer diagnoses.6
That rapid, accurate diagnosis is a key to improved outcome in the management of many hematologic malignancies is axiomatic. Because acute promyelocytic leukemia (APL) is a potentially curable disease that can be diagnosed quickly and definitively [using molecular techniques to identify the pathognomonic t(15:17)], and because APL is associated with significant early mortality if aggressive, supportive care measures to manage the bleeding complications caused by APL-associated disseminated intravascular coagulation are not rapidly implemented, this disease was targeted by ASH when the Society launched its initial foray into global health care. Beginning in 2004, ASH, through its International Members Committee, developed the International Consortium on Acute Promyelocytic Leukemia (IC-APL) that involved hematologists in Brazil, Mexico, Uruguay, and Chile. The goal of the IC-APL was to use available local laboratory and morphological analyses to identify patients with a suspected diagnosis of APL, rapidly confirm the diagnosis using molecular techniques through a centralized laboratory, and initiate therapy quickly.
Prior to this initiative, the overall survival rate for patients with APL in Brazil was 53 percent. Subsequent to implementation of IC-APL in Brazil, a two-year overall survival rate of 80 percent has been reported in the 97 evaluable patients who were enrolled in the program.7 Based on the success of this project, an ASH-sponsored program designed to provide support for management of other types of acute leukemia (in addition to APL) in these countries is under development, and this new, broader initiative will operate as the International Consortium on Acute Leukemia (ICAL).
Crucial to the success of IC-APL was the ability of the local hematologists to use fundamental hematologic skills, chiefly peripheral film and bone marrow morphologic interpretation, to identify those patients who might have APL. It is those basic skills that have been targeted for improvement in the several international locations being covered by ASH since 2007 in partnership with Health Volunteers Overseas, a nonprofit organization dedicated to improving global health through education. Hematologists working at sites in Uganda, Cambodia, and Peru vary in their diagnostic abilities, and they have asked for programs to improve their skills, as they appreciate that this is the first step to improving treatment and management of hematologic diseases. This assessment applies not only to malignant diseases such as ALL and APL, but also to non-malignant hematologic disorders including sickle cell anemia, thalassemias, and even iron deficiency anemia.
Key technologies that assist with these successful collaborations include using Web-based conferencing, recording and sharing clinical data between sites through the use of the Pediatric Oncology Network Database (POND), and making other educational resources available to international providers on websites such as St. Jude’s www.cure4kids.org. Web-based case conferences between partners enable timely pre-treatment consultations. However, studies show that over the course of a twinning relationship, the frequency with which these consultations change management declines, suggesting that this model has an educational component that leads to clinical independence.8 With the completion in 2009 of a submarine cable system, Internet connectivity was improved and expanded in large parts of Eastern and Southern Africa, making it possible to view educational case conferences and share diagnostic images between Fred Hutchinson Cancer Research Center in Seattle and the Uganda Cancer Institute in Kampala.
As with any health-related intervention, reliable data are required to measure the impact of twinning relationships. The POND is a centralized server used by multiple international programs including those of St. Jude’s twinning initiatives and ASH’s ICAL. This technology was designed to allow rapid translation of a database to other languages while reserving a standard format so that data can be compared and followed concurrently in different countries. This standardization also allows accurate analysis of research on outcomes and provides a mechanism for measuring the impact of ongoing improvement projects.9
While these technologies can play a large part in improving care, they are ineffective without also addressing the barriers to care faced by patients in low- and middle-income countries, including difficulties with transportation, cost of care, inadequate nutrition, and limited access to medications and diagnostic tools. Twinning relationships improve patient care, education, and teaching at both of the partnering institutions. The need to address disparities in health care is great, and pioneering programs such as those initiated by ASH and St. Jude Children’s Research Hospital have established a framework that can be built upon by other institutions and organizations to improve global health through support, service, and education.