Did Mark McGwire use it or not? We all have our opinions, but we do know that his wife used it. The drug is human growth hormone. Human growth hormone (HGH) is known to improve muscle strength and has been claimed as an anti-aging agent because it can increase lean body mass and bone mineral density, although there are limited data to support this claim. However, growth hormone is important in thymopoiesis. Administration of HGH or its proximal mediator, insulin-like growth factor-1 (IGF-1), can reverse thymic involution in aging mice and accelerate immune recovery in immune-compromised animals, including hematopoietic cell transplants (HCTs). HGH is produced by thymocytes, thymic epithelial cells, and mature lymphocytes. Under steady state, HGH and IGF-1 do little, but under periods of stress, they do have a beneficial effect.
There are accumulating data suggesting that following ablative HCT, especially in adults in the setting of T-cell depletion or cord blood transplantation, lack of adequate immune reconstitution is an important source of morbidity and mortality. We know that the thymus is the major site for the generation of new T cells and that functional recovery of the thymus is likely the single most important factor in allowing a patient to recover his or her adaptive immunity. Therefore, methods to improve and accelerate thymic function are an area of great interest and clinical need.
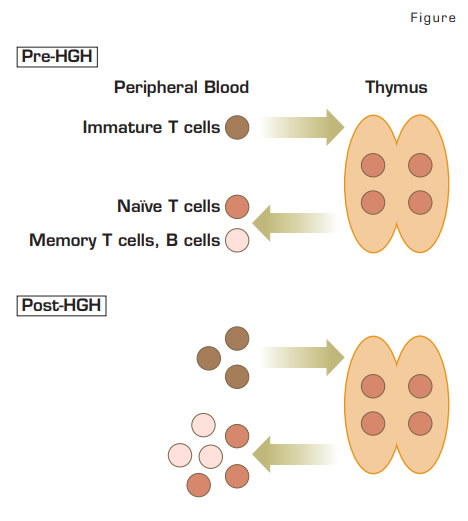
In this article, investigators performed a prospective, randomized study in 22 HIV-1–infected adult patients who were on highly active antiretroviral therapy (HAART). They received either daily subcutaneous injections of HGH for 12 months or were observed and then were crossed over to the other arm. This study confirmed the group’s previous observation that there was an increase in thymic mass and moderate increased numbers of naïve CD4+ T cells. HGH use increased de novo T-cell production as measured by the T-cell receptor excision circles (TRECs) and also increased peripheral T-cell expansion. An increase in thymic mass was also documented by CT scans. It is not clear how long this increase was sustained after the completion of the study.
Can we apply this study to patients receiving an HCT? In many ways, patients receiving an HCT can also have a significant impairment in T-cell numbers and function. CD4+ T cells may take several years to normalize, and peripheral homeostatic proliferation of a limited T-cell repertoire may result in significant skewing of these T cells as demonstrated by TCR spectratyping results. The overall result may be a limited ability of T cells to respond to new challenges. This restricted response can also be seen in aging individuals’ response to viruses, where fewer naive T cells result in a lower frequency of responder cells.
In Brief
Would HGH or IGF-1 work in HCT? Based on the results reported above, the expectation is that this approach could have a beneficial effect on immune recovery with certain caveats. For example, the effects of prior radiation to the chest or total body irradiation will destroy thymic epithelial cells. Graft-versus-host disease (GVHD) is another complication that has a direct effect on the thymus. In these two circumstances, there may not be sufficient residual thymic tissue for HGH to have an impact in thymopoiesis, although it could still expand the peripheral T cells. There is also the concern for increasing the risk of GVHD and other known side effects of this agent. Understanding how T cells are increased could identify specific patients that could benefit from HGH. Ultimately, we need a clinical trial with HGH transplantation to enhance the immune system’s performance.
Competing Interests
Dr. Chao indicated no relevant conflicts of interest.