Some patients with antiphospholipid antibodies have a clinical syndrome composed of thrombosis, fetal wastage, and, frequently, autoimmune cytopenias, livedo reticularis, and marantic endocarditis. In this report by Galli and colleagues, the authors analyzed the significance of a variety of antibodies found in patients with persistent antiphospholipid antibodies who participated in an international and prospective registry. Confirming the observations of previous studies, this analysis found that antibodies directed against ß2-glycoprotein I (ß2-GPI), or prothrombin, were associated with recurrent thrombosis and pregnancy loss. This analysis also confirmed some, but not all, previous studies demonstrating that anticardiolipin antibodies were not significantly associated with either of these two adverse events.
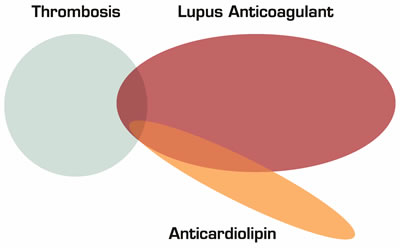
Figure 1: Anticardiolipin Antibodies Alone are not a Risk Factor for Thrombosis. Some patients with lupus anticoagulants have thrombi and some also have anticardiolipin antibodies. Anticardiolipin antibodies are not associated with thrombi unless a lupus anticoagulant is also present.
Figure 1: Anticardiolipin Antibodies Alone are not a Risk Factor for Thrombosis. Some patients with lupus anticoagulants have thrombi and some also have anticardiolipin antibodies. Anticardiolipin antibodies are not associated with thrombi unless a lupus anticoagulant is also present.
Antiphospholipid antibodies are a heterogenous group of autoantibodies directed against phospholipid-binding proteins. Some antiphospholipid antibodies will induce their target protein to soak up the small amount of phospholipid added to plasma during the PT and aPTT assays. These particular antibodies will prolong phospholipid-dependent coagulation tests and are called lupus anticoagulants. Other phospholipid antibodies are directed against cardiolipin, a phospholipid component of mitochondria originally described in bovine cardiac cells.
Approximately five to 10 percent of healthy people will have detectable antiphospholipid antibodies in their blood, although only a minority of people will have the persistent presence of these antibodies and have thrombotic or adverse pregnancy events. Since only a minority of patients with antiphospholipid antibodies have symptoms, several studies have investigated whether certain types of phospholipid antibodies better predict the subset of patients that will develop the full syndrome. The study by Galli, et al. confirms previous studies showing that the correlation between the antiphospholipid antibody syndrome and autoantibodies is most prevalent for lupus anticoagulants and anti-ß2-GPI (a common phospholipid-binding protein). But, what is the significance of antibodies against cardiolipin?
The Physicians’ Health Study produced the most widely quoted evidence that anticardiolipin antibodies are associated with venous thrombosis (Annals of Internal Medicine 1992;117:997-1002). In this large cohort of 22,071 male physicians, subjects with anticardiolipin antibody titers greater than the 95th percentile had an approximately five-fold increased risk of DVTs and PEs. Since this publication, the significance of these antibodies has been readdressed in numerous trials. Several of these trials are quite noteworthy because of their large size and findings that contradicted the Physicians’ Health Study. The LITE study, another very large trial of 21,680 subjects, found no increased risk of venous thrombosis in participants with greater than the 95th percentile of anticardiolipin antibodies (Br. J. Haematology 2002;119:1005-1010). Also notable is the lack of association between anticardiolipin antibodies and venous thrombosis in the HUNT trial that derived data from the 66,140 participants in the Health Study of Nord-Trondelag in Norway (J. Thrombosis and Haemostasis 2006;4:44-49). In a meta-analysis, again anticardiolipin antibodies were not associated with venous thrombosis (Blood 2003;101:1827-1832).
In Brief
What should we do with patients who have anticardiolipin antibodies and thrombosis? Certainly, in patients with recurrent thrombosis, fetal loss, livedo reticularis, and autoimmune cytopenias, the presence of anticardiolipin antibodies merely confirms the clinical diagnosis of an autoimmune-mediated thrombotic disorder. A much tougher decision has to be made when we find the presence of anticardiolipin antibodies in patients who have their first DVT, but no other laboratory tests or symptoms consistent with the antiphospholipid syndrome. If we let evidence be our guide, there is little to support treating such a patient any differently from the patient with a DVT and no laboratory abnormalities.
Competing Interests
Dr. Abrams indicated no relevant conflicts of interest.