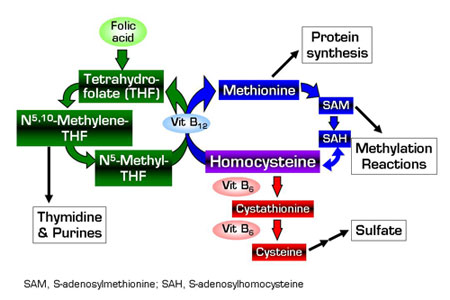
Mild hyperhomocysteinemia occurs in roughly 5–7 percent of the general population and is an independent risk factor for atherosclerosis, atherothrombosis, and venous thromboembolism. Homocysteine can directly injure and dysregulate endothelial cells, activate platelets and leukocytes, alter levels of coagulation and fibrinolytic mediators, stimulate vascular smooth muscle cell proliferation, oxidize LDL, and disturb extracellular collagen and matrix formation. As a key intermediary in the metabolism of methionine, folate, and cysteine (Figure), homocysteine is indirectly involved in transmethylation reactions, DNA and RNA synthesis (via generation of thymidine and purines), sulfate availability, and protein synthesis. Folic acid, vitamin B12 (cobalamin), and vitamin B6 (pyridoxine) are important regulators of these metabolic pathways (Figure), and low levels of these vitamins have been implicated as independent risk factors for venous and arterial disease. Hyperhomocysteinemia may result from deficiencies of these B vitamins, genetic defects involving remethylation (especially N5,10- methylene-THF reductase) and transsulfuration (especially cystathionine β-synthase), medical illnesses (especially renal failure and certain carcinomas), and medications (especially folate antagonists). Supplementation with folic acid and vitamin B12 can reduce normal or elevated homocysteine levels, and a number of recent and ongoing clinical trials are evaluating the efficacy of B vitamins in lowering homocysteine and preventing cardiovascular and venous thromboembolic disease. The primary prevention study reported by Lonn et al. (the Heart Outcomes Prevention Evaluation [HOPE] 2 trial) observed no benefit of supplementation with vitamin B12, folic acid, and vitamin B6 compared to placebo in reducing the incidence of death from cardiovascular causes, myocardial infarction (MI), and stroke among 5522 patients followed for an average of five years. Similarly, the Norwegian Vitamin [NORVIT] secondary prevention trial reported by Bønaa et al. found no improvement in the risks of recurrent MI, stroke, and sudden death over a 40-month median follow-up period among patients with a recent MI who received either vitamin B12, folic acid, and vitamin B6 (n = 937), folic acid and B12 (n = 935), or B6 alone (n = 934), compared to placebo (n = 943). Combined vitamin supplements (but not B6 alone) lowered the mean homocysteine levels by up to 20 percent in the HOPE 2 trial (33 percent had baseline levels ≥12.7 µmol/L) and 27 percent in the NORVIT study (40 percent had baseline levels >13 µmol/L). Of concern, the NORVIT study observed a trend toward increased risk of the primary endpoint among patients receiving any of the three vitamin supplement regimens (relative risk, 1.22; 95 percent CI, 1.00 to 1.50; P = 0.05), and this correlated with a baseline homocysteine level > 13 µmol/L.
In Brief
The results of these two studies, together with primary observations of the Vitamin Intervention for Stroke Prevention (VISP) trial1 , indicate that down-modulation of homocysteine with B-vitamin supplementation does not protect against primary or recurrent arterial vascular complications. By comparison, other recent data suggest that certain vascular complications2 or patient subgroups3 may derive benefit from B vitamins. The trend toward worse outcomes in the NORVIT study, along with observations of increased risk of in-stent restenosis among vitamin-supplemented patients4 , have spawned hypotheses that supraphysiologic vitamin levels "shunt" homocysteine toward metabolic pathways that adversely affect gene expression (via hypermethylation of DNA), protein synthesis, cell proliferation, and/or methylation of atherogenic molecules. It is not yet known whether these observations or mechanisms might be relevant to homocysteine modulation with vitamin supplementation for the prevention of venous thromboembolic disease. The current widespread use of dietary folate fortification and the relatively modest associations between homocysteine, B vitamins, and vascular disease limit the ability of these studies to assess a possible benefit or adverse effect of vitamin supplementation. A meta-analysis of pooled data from the many current clinical trials may offer important insights for clinical practice and public health policy. Future prospective studies will need well-defined stratification parameters, greater subject recruitment, and extended duration of treatment in order to achieve adequate statistical power for subgroup analyses.
References
Competing Interests
Dr. Linenberger indicated no relevant conflicts of interest.