The complete blood count (CBC) is approaching its 100th anniversary. Its inception can be dated to the 1930s, shortly after Maxwell Wintrobe, MD, wrote his impactful PhD thesis at Tulane University entitled The Erythrocyte in Man, and introduced the hematocrit and red cell indices.1 (The term “hematocrit” initially referred to the measuring tube used to determine packed red cell volume; however, the term was so appealing that hematologists and hematopathologists began to refer to the measurement itself as the hematocrit.) Further, more than 60 years have passed since Wallace Coulter introduced the first electronic particle counter, the Coulter Model A.2 This technique eventually led to the automated counting of red blood cells (RBCs), reticulocytes, specific types of white blood cells (WBCs), and platelets, as well as techniques for measuring hemoglobin content, mean corpuscular volume (MCV), and mean platelet volume (MPV), thus revolutionizing the availability and accuracy of blood cell counting and the ease of generating RBC indices.
Revolutionary technology has been applied to the generation of CBC data for more than half a century. We believe the CBC can be more impactful if applied with more precision and, therefore, propose a new strategy for its use, depending on the clinical situation. In the decades after the introduction of the Coulter counter, the CBC evolved into a growing hodgepodge of variables, which, depending on the lab, now includes up to 20 variables. Today, in the U.S., almost 2 million CBCs are performed daily, generating hundreds of millions of laboratory values annually.3 The CBC is a Dr. Frankenstein’s monster, containing low-value appendages (mean corpuscular hemoglobin [MCH], MCH concentration [MCHC]), anachronistic relics of the pre-Coulter era (percentage of WBC subtypes), and redundant measures reflecting approaches favored by different laboratories in the past (e.g., hematocrit and RBCs in addition to hemoglobin).
Trivial deviations from “normal” occur in about 30% of CBCs performed on healthy individuals. Thus, the CBC produces “abnormal” values, sparking patient anxiety and needless referrals. In addition, the clutter of redundant and obsolete values obscures the medically meaningful ones, particularly for the non-hematologist who orders most of the CBCs.
In an article recently published in the Annals of Internal Medicine, two of us proposed a strategy for revising the CBC, eliminating archaic and redundant values, and adding two streamlined versions of the CBC while maintaining the comprehensive CBC only when clinically indicated.4 That perspective sparked animated feedback.5 For some, changing the CBC “hit a nerve,” whereas others could not wait to reformulate the CBC at their institutions. While our discussion began in the wider internal medicine community, it is important that the hematology community be heard. We offer the following for consideration: 1) elimination of low-impact and outdated variables, including MCH, MCHC, and relative white cell counts; 2) selection of hemoglobin as the sole value representing blood oxygen-carrying capacity; and 3) elimination of total WBC when a white cell differential is performed. Also, given the innumerable CBCs performed for well individuals and patients with known diagnoses, we propose that a simplified version of the CBC could meet those needs.
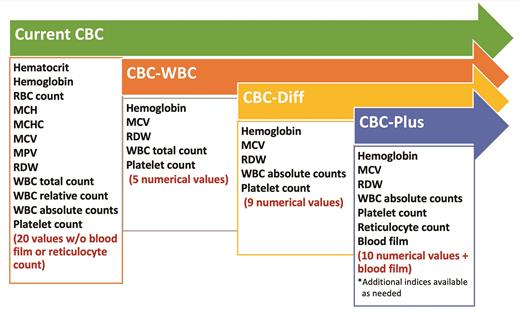
We propose the following three options (Figure):
1. CBC-WBC (or CBC-screen)
CBCs are a “routine” component of hospital admissions, initial outpatient visits, and periodic medical examinations in healthy individuals. The five variables required for screening in this group are quite different from those examined during evaluations for blood cell abnormalities or an acute or chronic illness.
2. CBC-Diff (or CBC-follow-up)
For patients who have completed chemotherapy, stem cell transplant, antibiotic therapy, and in other medical situations of a similar nature, incorporating the absolute counts of WBC subtypes is essential for promoting pathophysiological or diagnostic specificity.
3. CBC-Plus (or CBC-diagnostic)
The full CBC examination for patients undergoing any diagnostic evaluation or assessment for hematological abnormalities requires a blood film and reticulocyte count. Our array includes 10 numerical variables and the blood film. Additional blood cell indices, such as reticulocyte hemoglobin content, immature reticulocyte fraction, or mean platelet volume can be requested if necessary.
Each of these suggestions has drawn applause and criticism.5 A principal concern has been the absence of the MCHC, an index of spherocytosis; however, the MCHC is neither sensitive nor specific for spherocytosis. When there is concern about spherocytic hemolytic anemia, the inclusion of an absolute reticulocyte count and the blood smear in our CBC-Plus addresses this concern. Others expressed concern about the inability to calculate an index that can distinguish iron deficiency from thalassemia trait, although such indices are not as accurate as measurements of serum iron, ferritin, and hemoglobin A2 and F. Moreover, basophilic stippling on the blood film is the best screening method for differentiating these two entities, as basophilic stippling is a feature of thalassemia but not iron deficiency. Others, particularly surgeons, felt strongly that neutrophil percentage, but not the absolute neutrophil count, provided key information for the early detection of infection. We do not agree. As a fail-safe, the laboratory, for its own internal quality control reasons, will have variables not included in the report should these be required in a very rare case (if ever), such as MCH or MCHC.
There is precedence for streamlining the CBC. Since 1993, the CBC at Mayo Clinic in Rochester, Minnesota, reports only 12 variables, and these reports do not include leukocyte percentage. While this is not the norm, Mayo Clinic’s reporting is not an isolated phenomenon. A recent study conducted across 139 U.S. academic and community hospitals reported a median of 22 values included in the CBC (range: 12-24), with roughly 1 in 20 hospitals reporting less than 15 values in their CBCs.6
When considering updates to the CBC, it is critical that the hematologist and hematopathologist recognize that the vast numbers of CBCs are ordered without any likelihood of the patient having a hematological abnormality. In the unlikely case an abnormality is present, the proposed CBCs would identify it for further study.
We hope that our proposal is of interest to readers of The Hematologist and can generate productive discussions that lead to meaningful change for both institutions and patients.
Competing Interests
Drs. Burack, Go, and Lichtman indicated no conflicts of interest.