Combined hormonal contraceptives (CHCs), including pills, vaginal rings, and transcutaneous patches, are associated with a three-to eight-fold increased risk for venous thromboembolism (VTE) in CHC users compared to women not taking CHCs.1 Increases in procoagulant factors relative to natural anticoagulants on hormone therapy may explain this risk, in what may be an evolutionary adaptation for preventing postpartum hemorrhage.2,3 Due to the increased risk of VTE, CHC use is generally not recommended in patients with other strong persistent risk factors for thrombosis, including a personal history of venous thrombosis, malignancy, or high-risk thrombophilia.4,5 However, people on CHCs may acquire transient risk factors for VTE such as surgery or hospitalization. To date, there is a lack of evidence on whether temporary interruption of CHCs decreases the risk of postoperative VTE in CHC users, and if so, the optimal duration of CHC interruption.6 ´
Justine Hugon-Rodin, MD, PhD, and colleagues shed light on this issue by examining the persistence of hypercoagulability markers associated with VTE risk on CHCs following CHC discontinuation. PILL-OFF was a prospective observational study comparing outcomes in 66 Swiss women (age range: 18-50 years) who were planning to discontinue CHCs and 28 healthy controls. Plasma was obtained from participants at various time points within 12 weeks of CHC discontinuation. Hypercoagulability was assessed using normalized activated protein C sensitivity ratios (nAPCsr) and normalized thrombomodulin sensitivity ratios (nTMsr), which are measures of resistance to the natural anticoagulants activated protein C (APC) and thrombomodulin (TM). These results were obtained using a thrombin generation assay according to the equation below.7 Higher values correlate with increased resistance to the natural anticoagulant, which is associated with increased risk of VTE.
Abbreviations: APC, activated protein C; ETP, endogenous thrombin potential.
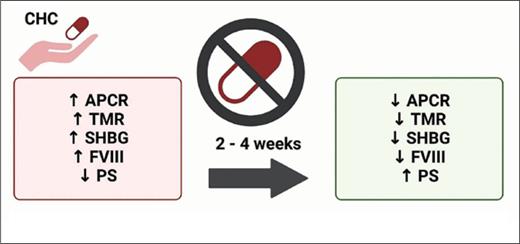
Baseline nAPCsr was 4.11 (standard deviation [SD]: 2.06) in CHC users compared to 1.09 (SD: 0.42) in controls. Baseline nTMsr was 2.53 (SD: 1.03) in CHC users compared to 1.00 (SD: 0.5) in controls. nAPCsr and nTMsr decreased to 1.27 (SD: 0.82) and 1.11 (SD: 0.58) by week 12, respectively, with more than 80% of this decrease occurring by week 2. Sex hormone binding globulin (SHBG), a marker of estrogen intake that may be correlated with VTE risk, also declined by a similar rate.8 A significant reduction in factor VIII activity was observed within a week of CHC discontinuation, and a significant increase in free protein S antigen was apparent by week 4. In a subgroup analysis, the type of CHC did not affect these parameters.
PILL-OFF is the most comprehensive longitudinal study to evaluate the persistence of hypercoagulability markers after CHC discontinuation. It found that biomarkers for VTE returned to control levels by approximately four weeks, with most of the reduction occurring during the first two weeks. A limitation of the study is the use of surrogate biomarkers for VTE, and thus it remains to be seen if temporary CHC interruption translates to a reduction in clinical VTE risk. It is also unknown how CHC interruption compares with a strategy of continuing CHCs while on extended postoperative thromboprophylaxis in the prevention of VTE. If confirmed, these findings will lend support to the practice of interrupting CHC prior to elective surgery with high VTE risk, including the care of transgender patients on hormone therapy undergoing gender-affirming surgery. Another potential application of these findings is guidance on the timing of CHC discontinuation in patients with hormone-associated VTE who remain on CHC and are nearing completion of anticoagulation therapy, because anticoagulation likely minimizes the risk for recurrent CHC-associated VTE.9
In Brief
CHC use is a risk factor for VTE. It is unclear whether patients on CHCs undergoing surgery should discontinue CHC or for how long prior to surgery its use should be discontinued to decrease the risk of postoperative VTE. PILL-OFF is a longitudinal cohort study demonstrating that plasma markers of coagulation return to baseline within two to four weeks of CHC discontinuation. The findings preliminarily support pausing CHCs one month prior to high-risk elective surgery, though confirmatory studies demonstrating a reduction in VTE risk are warranted prior to widespread adoption.
Competing Interests
Drs. Eswaran and Wilson indicated no relevant conflicts of interest.
Overview of the PILL-OFF trial design and its main outcomes
Abbreviations: CHC, combined hormonal contraceptive; POP, progestin only pill; APCR, activated protein C resistance; TMR, thrombomodulin resistance; SHBG, sex hormone binding globulin; FVIII, factor VIII; PS, free protein S. Created with BioRender.com
Overview of the PILL-OFF trial design and its main outcomes
Abbreviations: CHC, combined hormonal contraceptive; POP, progestin only pill; APCR, activated protein C resistance; TMR, thrombomodulin resistance; SHBG, sex hormone binding globulin; FVIII, factor VIII; PS, free protein S. Created with BioRender.com