A 4-year-old girl presented with abdominal distension and periorbital petechial rash, which had spread over the neck, face, and upper body. She was otherwise well without fever, weight loss, or other systemic symptoms. Her complete blood count revealed moderate thrombocytopenia (platelet count: 35 × 109/L; reference range: 150-400 × 109/L), a hemoglobin level of 10.7 g/dL (reference range: 10.2-12.7 g/dL), and a white cell count of 6.2 × 109/L (reference range: 4.9-13.2 × 109/L). Ultrasound imaging of the abdomen revealed hepatosplenomegaly. Computed tomography (CT) of the abdomen, pelvis, neck, and chest showed hepatomegaly without signs of lymphadenopathy. The patient was clinically diagnosed with immune thrombocytopenic purpura (ITP). She received intravenous immunoglobulins without response. Eventually, she underwent splenectomy and bone marrow examination. Histopathologic examination of the spleen (A-F) and bone marrow (G-I) is shown in the figure.
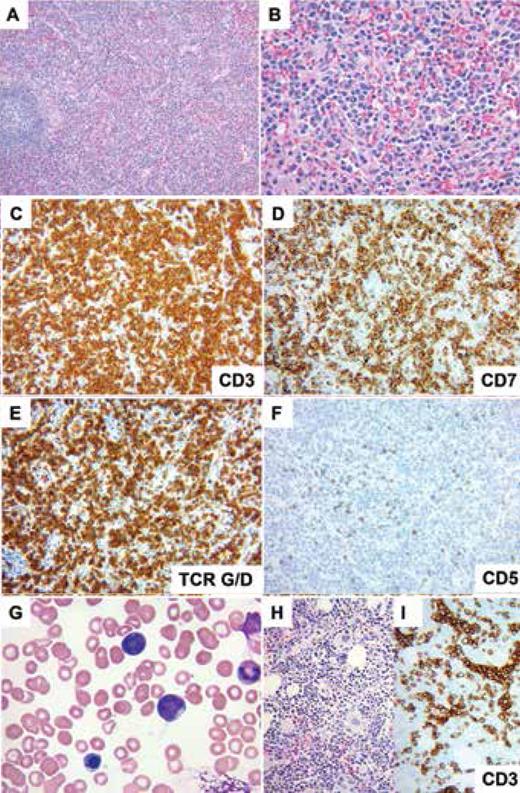
The spleen image shows monotonous proliferation of medium-sized lymphocytes with pale cytoplasm infiltrating dilated splenic sinuses (A, hematoxylin and eosin, 100x; B, hematoxylin and eosin, 400x). The cells are strongly positive for CD3 (C), CD7 (D), TCR gamma/delta (E), and negative for CD5 (F) (C-F, immunohistochemistry with hematoxylin counterstain, 200x).
The bone marrow aspirate smear shows intermediate-size lymphocytes with hyperchromatic nuclei, distinct nucleoli, and scant to moderate cytoplasm devoid of granules (G, Wright-Giemsa, 1,000x). The bone marrow biopsy shows normocellular marrow and a subtle lymphoid infiltrate (H, hematoxylin and eosin, 200x). Immunohistochemistry for CD3 highlights lymphocytes in the expanding sinuses (I, immunohistochemistry with hematoxylin counterstain, 200x).
The spleen image shows monotonous proliferation of medium-sized lymphocytes with pale cytoplasm infiltrating dilated splenic sinuses (A, hematoxylin and eosin, 100x; B, hematoxylin and eosin, 400x). The cells are strongly positive for CD3 (C), CD7 (D), TCR gamma/delta (E), and negative for CD5 (F) (C-F, immunohistochemistry with hematoxylin counterstain, 200x).
The bone marrow aspirate smear shows intermediate-size lymphocytes with hyperchromatic nuclei, distinct nucleoli, and scant to moderate cytoplasm devoid of granules (G, Wright-Giemsa, 1,000x). The bone marrow biopsy shows normocellular marrow and a subtle lymphoid infiltrate (H, hematoxylin and eosin, 200x). Immunohistochemistry for CD3 highlights lymphocytes in the expanding sinuses (I, immunohistochemistry with hematoxylin counterstain, 200x).
Hepatosplenic T-cell lymphoma (HSTCL) is a rare and clinically aggressive subtype of peripheral T-cell lymphoma seen predominantly in young adults, with a median age of approximately 35 years.1,3 Patients often present with marked hepatomegaly, splenomegaly, and B-symptoms. Lymphadenopathy and skin involvement are uncommon. Laboratory abnormalities commonly include cytopenias, as well as elevated serum levels of beta-2-microglobulin and lactate dehydrogenase. HSTCL is characterized by diffuse involvement including expansion of the red pulp cords and sinusoids, with atrophy or absence of white pulp.2 Sinusoidal infiltration, often with prominent sinusoidal expansion, can be observed in the liver and bone marrow.3,4
HSTCL cells are positive for CD2, CD3, and CD7, as well as cytotoxic markers such as TIA-1, perforin, granzyme M, and granzyme B. In contrast, HSTCL cells are negative for CD1a, CD4, CD5, CD8 (~20% positive), CD10, B-cell antigens, and terminal deoxynucleotidyl transferase (TdT). Positivity for the natural killer (NK)-cell-associated markers CD56 (~70%) and CD16 is also common. In situ hybridization results for Epstein-Barr virus-encoded RNA 1 (EBER1) are negative.4 Most cases express TCRγδ (~75%) followed by TCRαβ (~25%), while TCR receptors are absent in a small subset of cases (~5%).4,5 HSTCL carries monoclonal TCR rearrangements, isochromosome (7q) and/or trisomy 8, which are present in up to two-thirds and half of cases, respectively, with recurrent STAT3 (10%) and STAT5B (30%) mutations.2,5
The differential diagnosis for HSTCL includes other types of T-cell lymphoma and leukemia, including acute leukemia, and non-neoplastic processes such as immune thrombocytopenia or acute hepatitis.
What is the diagnosis?
T-cell large granular lymphocytic leukemia
T-cell lymphoblastic leukemia/lymphoma, gamma-delta (γ/δ) subtype
Hepatosplenic T-cell lymphoma
ALK-negative anaplastic large cell lymphoma
Competing Interests
Drs. Borkar, Khanlari, and Gheorghe indicated no relevant conflicts of interest.
For the solution to the quiz, visit The Hematologist online at www.hematology.org/TheHematologist/Image-Challenge.