In the late 1940s, new techniques of electrophoresis replaced the pioneering but insensitive moving boundary method of the Swedish Nobelist in chemistry, Arne Tiselius. These advanced methods used solid or gel matrices to separate compound mixtures into readily definable bands or zones. By the mid to late 1950s, “zonal electrophoresis” on solid matrices, including paper, provided a simple technology to identify minute differences in protein mixtures. With this technique in hand, the presence of small, stable human lymphohematopoietic cell clones (neoplasms) became evident in the late 1950s because of the ability to identify small concentrations of serum immunoglobulins that migrated as monoclonal bands on zonal plasma or serum protein electrophoresis.1 This ability was enhanced as more sensitive immunological techniques for measuring monoclonal proteins in serum and urine were developed. These small, stable B-cell clones could be inferred at that time because they had a phenotype, a detectable plasma, or urinary monoclonal immunoglobulin.
The presumptive clones initially were referred to as asymptomatic or benign monoclonal gammopathy. In some cases, they were not asymptomatic or benign because the monoclonal protein was capable, idiosyncratically, of causing tissue damage, for example, to nerve, kidney, or cornea, or of inactivating or simulating a plasma protein leading to a variety of pathological states.1 Moreover, soon after their discovery, it became apparent that some clones were not invariably stable but developed subsequent cooperating mutations leading to clonal evolution and a morbid and potentially lethal neoplasm of B lymphocytes. Dr. Robert Kyle and his colleagues have provided singular insights into the epidemiology, pathobiology, and consequences of monoclonal gammopathies broadly. A report from Dr. Kyle's program at the Mayo Clinic in 2002 showed the quantitative risk of clonal evolution to a potentially lethal neoplasm was approximately 1.0 percent of patients per year over two decades of observation.2 This estimate was later reconfirmed and extended.3 Since the development of small B-cell clones is a function of age, increasing in incidence in a quasiexponential manner after age 45 years, most patients die of an unrelated cause. Contrariwise, virtually all cases of myeloma have as their antecedent a variable period of an indolent monoclonal gammopathy. It was proposed, not unreasonably, that the prefix “asymptomatic” or “benign” should be replaced. The suffix “of unknown significance” was suggested 45 years ago.4 This proposal became the defining term: monoclonal gammopathy of unknown significance (M-GUS). Today, the suffix “of unknown significance” is imprecise and misleading because the significance of a monoclonal gammopathy has clearly come into view; it occasionally results in symptomatic disease as an idiosyncratic effect of the monoclonal protein on a specific tissue, such as nerve or kidney, and has a semiquantitatively defined risk of progression to a B-lymphocytic malignancy, notably myeloma, lymphoma, macroglobulinemia, or amyloidosis. It is analogous to an adenoma of epithelial tissue (e.g., adenomatous villus polyp of the colon).5,6 Certain features of the lymphocytic clone increase the risk of its evolution to a potentially lethal neoplasm (e.g., concentration or isotype of immunoglobulin and ratio of serum immunoglobulin light chains).3
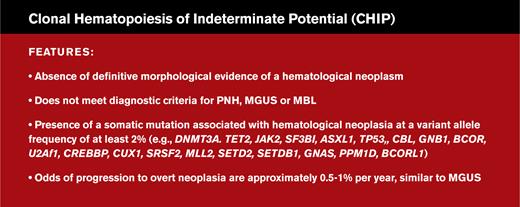
With the ability to use advanced genetic techniques to identify stable hematopoietic (myeloid) clones, the designation clonal hematopoiesis of indeterminate potential (CHIP) was coined.7 These clones, characteristically, do not have a phenotype and have a low risk of progression to, usually but not exclusively, a myeloid neoplasm, especially myelodysplastic syndrome or acute myeloid leukemia. They also indicate a predilection for vascular, and possibly inflammatory and immunologic disease. These intriguing relationships are being studied to better understand their pathogenesis.8,9 More recently, genetic analysis has permitted the distinction between a myeloid CHIP and a lymphoid CHIP, so designated because of the predisposition to undergo clonal evolution to either a myeloid or lymphoid neoplasm, respectively.10
A proposed definition of CHIP. A mutation that is commonly associated with clonal expansion of hematopoietic cells in older persons should be present, whereas criteria for other diagnoses should not be met. From Steensma DP et al. Clonal hematopoiesis of indeterminate potential and its distinction from myelodysplastic syndromes. Blood. 2015;126(1):9-16.
A proposed definition of CHIP. A mutation that is commonly associated with clonal expansion of hematopoietic cells in older persons should be present, whereas criteria for other diagnoses should not be met. From Steensma DP et al. Clonal hematopoiesis of indeterminate potential and its distinction from myelodysplastic syndromes. Blood. 2015;126(1):9-16.
The physician-scientists initially reporting this important new finding, CHIP, eschewed the suffix “of unknown significance” because the significance of such small, usually stable clones was evident.5 However, the choice of the suffix “indeterminate potential” was perhaps just off point. Their “potential” also had been determined. Their time of progression could not be. Thus, “indeterminate progression” is a more precise and relevant term.
Monoclonal gammopathy (B-cell clonal lymphopoiesis) and (mono) clonal hematopoiesis (clonal myelopoiesis or lymphopoiesis) without a phenotype should be unified pathogenically. They are the same fundamental process. This unity can be achieved by using the suffix “indeterminate progression,” resulting in monoclonal gammopathy of indeterminate progression with the acronym M-GIP and clonal hematopoiesis of indeterminate progression, maintaining the acronym CHIP, whether myeloid or lymphoid. Such a change in nosology would clarify their nature and unify precisely similar pathogenetic processes of related tissues, each tissue a derivative of the totipotential lymphohematopoietic stem cell. The World Health Organization Classification of Tumours of Haematopoietic and Lymphoid Tissues should consider revising the designation of small indolent lymphohematopoietic clones, harmonizing diagnostic terms with pathogenesis.
There is much we have yet to learn about the process of age-related clonal evolution and the progression from clonal hematopoiesis to a potentially lethal neoplasm. As suggested when first reported, the goal of interrupting the evolution of indolent CHIP or M-GIP to a lethal derivative neoplasm is an outcome to be sought.11
Competing Interests
Dr. Lichtman indicated no relevant conflicts of interest.