Oncogenic activation of kinases drives many hematologic and nonhematologic tumors, yet this very dependency on activated kinase signaling pathways also represents an Achilles' heel for the tumor — the oncogene or its pathway are often amenable to targeted pharmacologic inhibition. Since the advent of imatinib to effectively treat chronic myeloid leukemia and other BCR-ABL1–translocated hematologic neoplasms, several inhibitors have been developed that inhibit oncogenic kinases driving diverse types of neoplasms. The anaplastic lymphoma kinase (ALK) gene was initially cloned from the site of a recurrent translocation in anaplastic large cell lymphoma, which juxtaposed it to the NPM1 gene.1 Since then, ALK rearrangements have also been identified in diverse tumors, including diffuse large B-cell lymphoma, several carcinomas, and inflammatory myofibroblastic tumors.2 These rearrangements fuse ALK with various partners, producing fusion proteins in the tumors that dimerize, causing constitutive ALK kinase activity that drives tumor proliferation. In recent years, several small molecule tyrosine kinase inhibitors have been used to effectively treat ALK-translocated tumors3 ; thus, it is clinically important to identify tumors that bear these genetic rearrangements. Immunohistochemistry for ALK protein expression generally correlates with its activation through translocation and is helpful to identify ALK-rearranged lymphomas and other tumors.4
Dr. Paul G. Kemps and colleagues have further expanded the spectrum of ALK-rearranged tumors by studying a cohort of 39 cases of ALK-positive histiocytosis. This entity was first described in three infants in 2008 by Dr. John K. C. Chan and colleagues, who noted systemic infiltration of bone marrow and other organs by large histiocytes expressing ALK protein (not normally expressed in histiocytes) and identifying a TPM3-ALK translocation in one case.5 Since then, relatively few cases have been reported, and the series by Dr. Kemps and colleagues is by far the largest assembly of these cases. The authors retrospectively retrieved ALK-positive histiocytosis from several countries, confirmed the diagnoses by central review, and performed genetic testing to confirm an ALK rearrangement as needed. Their diagnostic criteria were a histologically confirmed lesion composed of histiocytic cells (expressing at least 2 macrophage/histiocyte markers) expressing ALK protein, in which an ALK rearrangement was confirmed by genetic methods; diffuse strong ALK immunostaining in histiocytes was considered sufficient for “classic” cases in infants with systemic disease.
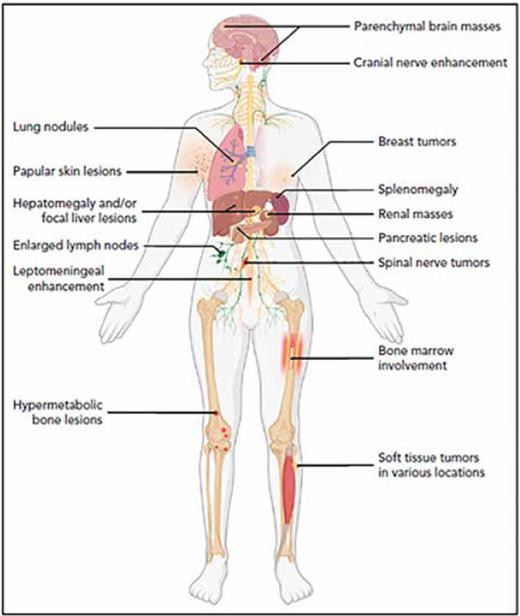
The authors described three main patterns of disease involvement. Group 1A consisted of infants (up to 5 months old) with systemic disease involving the liver and bone marrow who presented with hepatomegaly, anemia, and thrombocytopenia. Group 1B was made up of children and adults with disseminated disease involving the nervous system, bone, lungs, and other organs, often presenting with multiple masses in the brain and cranial and/or spinal nerves; and group 2 was composed of children and adults with single-system disease, most often affecting the nervous system and often presenting with diverse neurological symptoms. These findings indicate that ALK-positive histiocytosis involves a larger age range (including adults up to age 41 years), has a predilection for female individuals, and has a more diverse array of clinical presentations (including frequent neurologic manifestations) than previously thought (Figure). They also documented more diverse pathologic features than previously recognized; while the classic features of foamy histiocytes and giant cells were commonly observed, many cases had a more cellular or spindled morphologic appearance that may not be recognized as a histiocytosis or could be erroneously diagnosed as a histiocytic sarcoma. The pattern of ALK immunostaining was subtle in some cases, being limited to focal weak or dot-like cytoplasmic staining that could be missed in cases with bona fide ALK rearrangements. Despite frequent disseminated disease, most patients had favorable outcomes, including spontaneous regression of some group 1A cases. Approximately half of the patients were treated with systemic chemotherapy and/or ALK inhibitors, and 59 percent of patients were alive with no evidence of disease in the latest follow-up.
ALK-positive histiocytosis can affect numerous anatomic sites, with bone marrow and liver being most common in Group 1A, and nervous system, liver, lung, and bone being most common in Group 1B and Group 2 disease subgroups. Adapted from Figure 6, Kemps PG et al. ALK-positive histiocytosis: a new clinicopathologic spectrum highlighting neurologic involvement and responses to ALK inhibition. Blood. 2022;139:256-280.
ALK-positive histiocytosis can affect numerous anatomic sites, with bone marrow and liver being most common in Group 1A, and nervous system, liver, lung, and bone being most common in Group 1B and Group 2 disease subgroups. Adapted from Figure 6, Kemps PG et al. ALK-positive histiocytosis: a new clinicopathologic spectrum highlighting neurologic involvement and responses to ALK inhibition. Blood. 2022;139:256-280.
The work of Dr. Kemps and colleagues has not only better defined these features but also raised awareness of these rare and likely underrecognized tumors. Indeed, all patients in their cohort who were treated with ALK inhibition (including some who had failed conventional chemotherapy) achieved sustained objective responses. An important challenge is that physicians (both clinicians confronted by patients' diverse symptoms and pathologists who encounter affected biopsies) may not consider this diagnosis, thus missing the opportunity to identify a tumor amenable to effective targeted therapies. Histiocytes often “just don't get any respect” by pathologists since they are usually benign cells in the background accompanying inflammatory or infectious processes. Moreover, the histiocytes in ALK-positive histiocytosis are bland-appearing and may not suggest a clonal, neoplastic process. I recall a case of an infant presenting with bone marrow disease that was initially missed by several esteemed hematopathologists (including myself); once an ALK immunostain was done, the diagnosis became clear, but the pathologist must first consider this entity a diagnostic possibility. The authors recommend ALK immunostain as a screening test when considering a diagnosis of ALK-positive histiocytosis; however, it is important to determine that the ALK staining is actually in the histiocytes and not in other cell types. The authors also recommend confirming ALK rearrangement by cytogenetics, ALK fluorescent in situ hybridization (FISH), or an RNA-based fusion assay. While the previously reported KIF5B-ALK fusion was the most common in this cohort,6 there were several other ALK fusion partners identified.
In Brief
In summary, Dr. Kemps and colleagues have provided a comprehensive analysis of this rare histiocytosis, which has expanded the diverse array of tumors that are driven by ALK activation. Hematologists and hematopathologists who are confronted by a histiocytic proliferation of uncertain etiology, particularly in an infant with bone marrow disease or in a child or adult with tumors in the nervous system, liver, lung, or bone, should consider the possibility of an ALK-positive histiocytosis. Accurate diagnosis of this rare histiocytosis is important to identify patients who may benefit from targeted ALK-inhibitor therapy.
Competing Interests
Dr. Hasserjian indicated no relevant conflicts of interest.