I must admit to a certain amount of prognostic index fatigue in the lymphoma world. In diffuse large B-cell lymphoma (DLBCL), we have the original International Prognostic Index (IPI; with the age-adjusted subcategory), the Revised IPI (R-IPI), the NCCN (National Comprehensive Cancer Network) IPI, and the CNS (central nervous system) IPI. In follicular lymphoma, we have the FLIPI, the FLIPI-2, and the M7-FLIPI. In mantle cell lymphoma, we have the MIPI and the MIPI-C. In Hodgkin lymphoma, we have the IPS-7 and the IPS-3. In T-cell lymphomas we have four options: the IPI, the PIT, the IPTCLP, and the mPIT. We even have distinct prognostic indices for each marginal zone lymphoma subtype (nodal, splenic, and MALT type). Thank goodness for smartphone apps.
So, when I heard about a new prognostic index for Burkitt lymphoma (BL), I was dubious. However, upon further review, this index (BL-IPI) appears to be a significant contribution. Dr. Adam Olszewski and colleagues recently published the results of this international effort and made the case for a new index. Historical tools classified BL as low-risk or high-risk. The problem is that 85 to 90 percent of newly diagnosed patients typically fall into the high-risk category, yet most of these patients are cured. A prognostic index needs better discriminatory power. Using the risk factors in the IPI for DLBCL was also not optimal as most patients with BL have elevated lactate dehydrogenase, and most are under the age of 60 years.
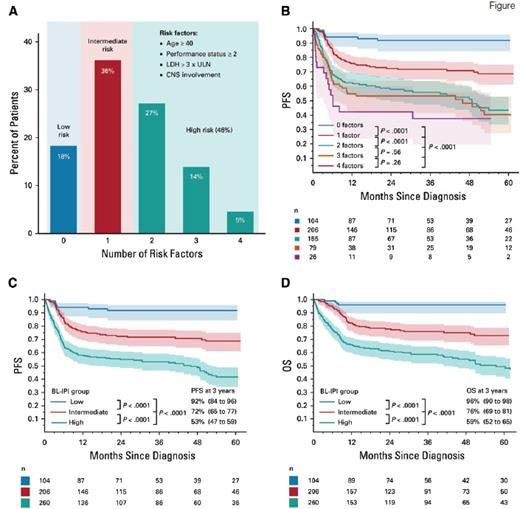
These investigators pooled retrospective data from 30 centers in the United States, involving 633 adult patients with BL treated between 2009 and 2018. Many potential factors were analyzed for their prognostic usefulness, and standard statistical techniques were applied to cull the list down to four variables with roughly equal risk estimates. The factors that made up the model included age older than 40 years, lactate dehydrogenase greater than three times the upper limit of normal, performance status greater than 2, and CNS involvement. Each factor contributes one point in the model, and three risk groups were generated: low-risk (0 risk factors; 18% of patients; 3-year progression-free survival [PFS], 92%), intermediate-risk (1 risk factor; 36% of patients; 3-year PFS, 72%), and high-risk (2-4 risk factors; 46% of patients; 3-year PFS, 53%; Figure). The investigators then used data from an international data set involving 457 patients as a validation cohort. The validation cohort demonstrated highly similar risk distribution and outcomes.
Characteristics of the BL-IPI I U.S. derivation cohort.
A) Proportion of patients according to the number of risk factors. B) Progression-free survival (PFS) according to the number of risk factors; PFS of patients with two versus three, and three versus four risk factors was not statistically significantly different, and hence, these groups were combined in the high-risk category. C) PFS according to Burkitt lymphoma International Prognostic Index (BL-IPI) risk group. D) Overall survival (OS) according to BL-IPI risk group; 3-year PFS and OS estimates are listed with 95% CIs (in parentheses); p values are from log-rank tests comparing groups sequentially and from an overall log-rank test. Abbreviations: LDH, lactate dehydrogenase; ULN, upper limit of normal. From J Clin Oncol, Olszewski AJ, Jakobsen LH, Collins GP, et al, Burkitt Lymphoma International Prognostic Index, vol. 39, pp 1129-1138, Copyright © 2021 Wolters Kluwer Health, Inc. Reprinted with permission from Wolters Kluwer Health, Inc.
A) Proportion of patients according to the number of risk factors. B) Progression-free survival (PFS) according to the number of risk factors; PFS of patients with two versus three, and three versus four risk factors was not statistically significantly different, and hence, these groups were combined in the high-risk category. C) PFS according to Burkitt lymphoma International Prognostic Index (BL-IPI) risk group. D) Overall survival (OS) according to BL-IPI risk group; 3-year PFS and OS estimates are listed with 95% CIs (in parentheses); p values are from log-rank tests comparing groups sequentially and from an overall log-rank test. Abbreviations: LDH, lactate dehydrogenase; ULN, upper limit of normal. From J Clin Oncol, Olszewski AJ, Jakobsen LH, Collins GP, et al, Burkitt Lymphoma International Prognostic Index, vol. 39, pp 1129-1138, Copyright © 2021 Wolters Kluwer Health, Inc. Reprinted with permission from Wolters Kluwer Health, Inc.
In Brief
The BL-IPI index has many good qualities. It is simple, appears robust, and is tailored to this unique disease. It will allow clinicians to talk to their patients with more precision than before. It will also aid in the design and interpretation of clinical trials. Clearly the high-risk patients have the greatest need for novel strategies. The low-risk patients might be appropriate for carefully designed trials evaluating therapeutic de-intensification. The interpretation of outcomes from single-arm trials will be much more straightforward. Overall, this was a tremendous effort by these investigators and a valuable addition to the lymphoma literature.
Competing Interests
Dr. Kahl indicated no relevant conflicts of interest.