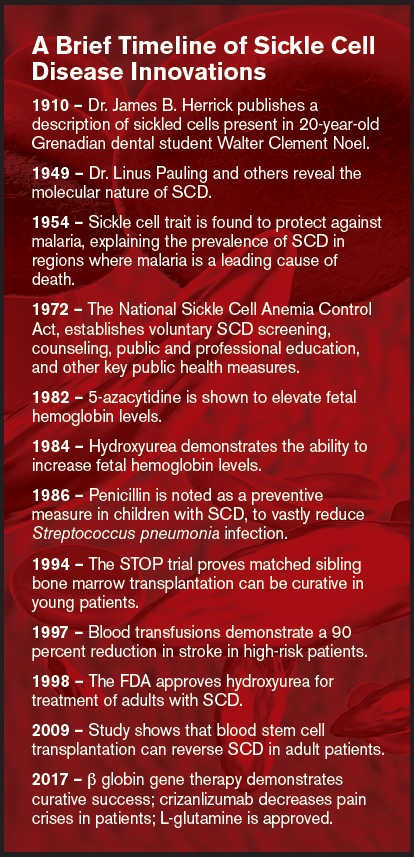
A timeline of some discoveries and innovations pertaining to sickle cell disease diagnosis and treatment
A brief timeline of sickle cell disease innovations.
A brief timeline of sickle cell disease innovations.
It has been more than a century since the first U.S. case of “sickle-shaped cells” was described by Dr. James B. Herrick and his resident after they examined the peripheral blood of a young Chicago dental student reporting episodic pain.1 It was more than six decades ago in 1956 that Dr. Vernon Ingram, building on the discoveries of Drs. Linus Pauling and Harvey Itano, elucidated the biochemical explanation by showing that the substitution of glutamic acid with valine in the β globin chain of hemoglobin accounts for the unique shape of the affected red blood cells and their sensitivity to low-oxygen states.2
Sickle cell disease (SCD) was the first disease understood at the molecular level. Yet, in the 62 years since that discovery, cure has been achieved only for the rare patient able to undergo successful stem-cell transplantation — a procedure that is viable for only the 20 percent of affected individuals having a matched sibling donor. Infection prophylaxis, folate supplementation, and hydroxyurea therapy, introduced in the 1980s to bolster the production of fetal hemoglobin, remain the most common interventions. L-glutamine recently has been shown to reduce the number of pain crises throughout a 48-week period.3 However, treatments targeting the root cause of the illness remain elusive despite our exquisite understanding of its origins and pathophysiology.
In a monogenetic disease, gene replacement therapy is an attractive option. Why then hasn’t that insight led to cure? To hear him tell it, this is one of the key questions that has vexed Dr. Francis Collins, director of the National Institutes of Health (NIH) and a lifelong student of human genetics. Two years ago, Dr. Collins turned his eye toward SCD and convened a high-level brainstorming retreat to answer exactly that question. “Not just treat it but cure it,” Dr. Collins has been quoted as saying. “I think we can do that, and we should not rest until we do.”
The Cure Sickle Cell Initiative is the result of this retreat. The core aim is to utilize a funding mechanism that is more nimble and more flexible than the traditional grants and contracts paradigm. It was clear to all the participants in the retreat that the traditional NIH mechanisms are structurally too slow for what is needed for late-stage translational research. Where a traditional grant may take 12 to 18 months from submission to contracting, the hope was to build a program where federal funding could be available in days or weeks.
Taking as a model the Defense Advanced Research Projects Agency (DARPA, the early federal funding that helped kick-start the internet), this national funding mechanism is called Other Transactional Authority (OTA). Traditionally, funding from NIH or the National Heart, Lung, and Blood Institute (NHLBI) favors hypothesis-driven research, largely focused on discovery and early translation. But the gap in SCD is development and deployment — the so-called “valley of death” in developing new therapies. The OTA will allow for funding projects that are aimed at accelerating advancement from concept to bedside.
Dr. Collins has said that this new funding mechanism exemplifies a new systemic approach to this disease. But it is not just the commitment to deliver financial support rapidly and to projects that are highly translational. The programmatic effort will include:
Assistance to investigators in how to navigate the federal regulatory process. What are the administrative hurdles in activating a clinical trial or multicenter effort?
Strengthening the input of patients and families in the design and implementation of clinical trials and novel treatments. A key part of this will be leveraging ASH's development of a registry and a sickle cell disease clinical trials network. ASH has built the core data collection infrastructure of the registry and is soliciting initial participants. ASH will also be soliciting applications for the network later this year.
Directing support to technical advancements that are aimed at making novel approaches more universally available. For instance, scaling up production of key reagents needed to advance clinical studies to the next stage, or
Encouraging novel endpoints and clinical trial designs. It has long been known that too often, only patients with the most advanced disease participate in higher-risk investigational endeavors. For example, most gene therapy or gene editing trials are likely to be undertaken in adults, yet those individuals are more likely to have organ dysfunction or comorbidities. How can we more rapidly get innovative treatments to patients before their disease makes them unlikely to benefit?
Dr. Collins will give a keynote talk at the Presidential Symposium taking place at the 2018 ASH Annual Meeting in San Diego, December 1-4, 2018, and is expected to touch on the Initiative in his talk on “Accelerating Cures in the Genomic Age.” Dr. Collins will describe not only how fundamental advances in understanding viral vectors, targeted cells, and genetic modification are advancing the field, but also what government entities such as NHLBI and NIH can do to foster these advances.
Skeptics might regard this initiative as lofty or even nonviable. Lofty, perhaps, but certainly realistic. After all, it is by envisioning a perfect outcome that one can devise a plan to get there.
The Method to Our Movement
It is exciting to see so much traction in the field of sickle cell research in the past decade. The number of therapeutic clinical trials currently available for sickle cell disease on clinicaltrials.gov has increased exponentially between 2008 and 2018. We have had the second FDA-approved drug for reducing pain episodes in sickle cell, L-glutamine, announced in July 2017. And for the first time, there was a new therapeutic intravenous agent, crizanlizumab, proven in randomized phase II-III clinical trials to be effective in preventing sickle cell vaso-occlusion for all sickle cell genotypes, including the often-forgotten double heterozygotes Hgb SC and SB+ thalassemia.
This is all good news for the individual living with SCD and for their treating providers. Curative therapies for SCD are no longer just whispered about and considered a pipe dream but are now front and center in the Cure Sickle Cell Initiative. This bold initiative will catapult curative therapy to nearly every patient, using novel regimens and stem cell sources as well as gene editing technology. The role of the patient and the sickle cell community has also become more visible, and they are being truly engaged as equal partners in investigating therapeutic and supportive care options for persons living with SCD, including the older adults who are now living well into their sixth decade and beyond.
A friend of mine living with homozygous SS recently shared her thoughts. “What about us ’mature’ sickle cell adults? Why do clinical trials have to cap at age 45 or 50? I am planning to live to be 99 years old with no teeth and a walker, so how long will I have to wait to benefit from emerging therapies that can help me?” Having benefitted from past scientific successes that brought comprehensive care and hydroxyurea to the mainstream management of SCD she states, “I am ready for the future, but y'all researchers and clinicians need to keep up.”
This article by Dr Benz brings visibility to the fact that clinicians, researchers, and funders are indeed trying to “catch up,” borrowing a phrase from my dear friend. The Cure Sickle Cell Initiative demonstrates a pragmatic approach to move the sickle cell research needle further and faster to keep up with the improvement in care outcomes we have seen in pediatrics. SCD is now considered an adult disease as patients are living longer. However, we are also seeing more of the long-term impact of chronic organ damage as adults with SCD age, and this forces us to not be complacent. It is not enough to show that we have improved infant mortality rates and that children are surviving 98 percent of the time into adulthood. We must take it a step further to ensure that every patient everywhere and at every time in their life trajectory has access to age-specific comprehensive care that includes shared decision making that gives each individual the ability to avail themselves of novel therapies to improve long term morbidity and mortality and yes, to cure their disease.
The Cure Sickle Cell Initiative is also about timeliness of delivering these innovative interventions for SCD As my friend said, her window of benefit from science to improve her long-term outcomes is “now,” at age 62 years, so that she can safely and securely make it to age 99 years, with no teeth and a walker.”
–Ifeyinwa (Ify) Osunkwo, MD, MPH, Atrium Healthcare (formerly Carolinas HealthCare System), Levine Cancer Institute, Charlotte, NC
References
Competing Interests
Dr. Benz and Dr. Osunkwo indicated no relevant conflicts of interest.