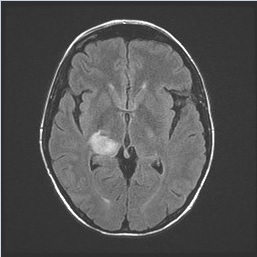
A 34-year-old woman presented to clinic on day 95 following allogeneic, myeloablative matched unrelated bone marrow transplantation with cyclophosphamide and total body irradiation conditioning for T-cell acute lymphoblastic leukemia. Transplantation had been complicated by pericardial effusion secondary to tacrolimus and by grade 1 graft-versus-host disease of the skin, both of which had resolved. She remained on sirolimus and prednisone 10 mg daily for immune suppression; she then developed sudden onset visual changes. A comprehensive eye examination noted no intraorbital pathology but demonstrated postchiasmal incongruous left hemianopsia. A brain MRI scan revealed a peripherally enhancing lesion centered in the right thalamus and subcentimeter enhancing lesions associated with petechial hemorrhage at the surface of the right superior colliculus and cerebellar vermis (Figure 1). Lumbar puncture was performed, but cerebrospinal fluid (CSF) analysis did not provide a diagnosis. The patient then underwent a brain biopsy with results below.
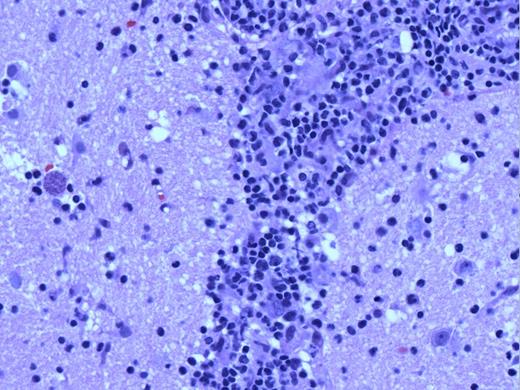
Low-power pathologic image showing fragments of brain tissue with areas of necrosis (arrowheads), as well as a patchy lymphoid infiltrate, including distinctly perivascular infiltrates (arrow).
Low-power pathologic image showing fragments of brain tissue with areas of necrosis (arrowheads), as well as a patchy lymphoid infiltrate, including distinctly perivascular infiltrates (arrow).
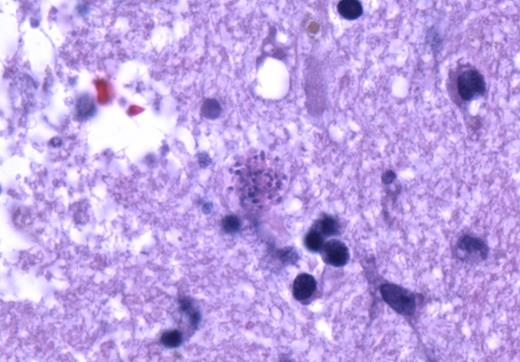
High-power image magnifying round structure seen to the left of the blood vessel in Figure 2.
High-power image magnifying round structure seen to the left of the blood vessel in Figure 2.
A. Central nervous system relapse of T-precursor acute lymphoblastic leukemia
B. Post-transplant lymphoproliferative disorder
C. Toxoplasmosis
D. Cryptococcus
Sorry, that was not the preferred response.
Correct!
A low-power image (Figure 2) shows fragments of brain tissue with areas of necrosis (arrowheads), as well as a patchy lymphoid infiltrate, including distinctly perivascular infiltrates (arrow). The arrowed area is shown at higher power in Figure 3. There is a dense lymphoid infiltrate surrounding the blood vessel, composed of small to medium-sized lymphocytes with condensed chromatin and variably irregular nuclei. Immunohistochemistry demonstrated that the lymphocytes were almost entirely CD3+ and CD5+, with a predominance of CD8+ over CD4+ cells; few CD20+ cells were present. They were negative for CD34, TdT, and CD117. The infiltrate was also negative for EBER. Additionally, there is a round structure seen to the left of the blood vessel, which is enlarged in Figure 4.
The round structure in Figures 3 and 4 represents a classical toxoplasmosis cyst, formed due to the host’s immune response to this organism. Multiple such structures were encountered in this biopsy. Toxoplasma cysts consist of bradyzoites aggregated within a membrane-bound cystic structure and are essentially diagnostic of Toxoplasma gondii. It usually is seen in the latent or chronic forms of infection and tends not to elicit an immune response, though in this case it is evident in an active tissue infection. The diagnosis of toxoplasmosis was also confirmed in this case by a positive qualitative polymerase chain reaction CSF test, which has a high degree of specificity.
The lymphoid infiltrate in this biopsy showed a mature phenotype with a predominance of CD8 over CD4. Early T-precursor lymphoblastic leukemia/lymphoma is characterized by dim or negative CD5, lack of CD8, and expression of myeloid and/or stem cell markers. This patient’s prior acute leukemia was dim for CD5 and negative for both CD4 and CD8, and additionally expressed CD34 and TdT. Thus, a recurrence of her leukemia was excluded.
Post-transplantation lymphoproliferative disorders most commonly are B-lineage, and most are associated with Epstein-Barr virus. The infiltrate in this case contained a paucity of B cells and was EBER negative. While uncommon T-lineage post-transplantation lymphoproliferative disorders are encountered, these tend to be of late onset. The lymphoid infiltrate in this case was deemed to have insufficient diagnostic features of T-cell lymphoma, especially considering the presence of toxoplasmosis in the biopsy, and was thus considered reactive.
Cryptococcus neoformans is a fungal organism that manifests as encapsulated yeast cells and would not form the cyst structure illustrated in this case.
References
References
Dr. Runaas and Dr. Kroft indicated no relevant conflicts of interest.