“My life amounts to no more than one drop in a limitless ocean. Yet what is any ocean, but a multitude of drops?”
“Our lives are not our own. We are bound to others, past and present, and by each crime and every kindness, we birth our future.”
-From David Mitchell’s Cloud Atlas
In November 2000, less than a month after exchanging wedding vows, a 38-year-old man developed nagging back pain. A CBC revealed mild leukocytosis, anemia, and marked eosinophilia. Within short order, he developed slurred speech, a rightward protrusion of the tongue, diminished patellar reflexes, and loss of sensation in his groin and thighs. MRI of the brain and spine showed a diffusely increased marrow signal and a collection of paraspinal masses choking his spinal cord. A bone marrow biopsy was effaced with eosinophils, markedly hypercellular and fibrotic, and left-shifted with slightly increased myeloblasts. Testing for BCR-ABL1 was negative. He was diagnosed with an eosinophilic leukemia with extensive extramedullary disease. Over the following year, he underwent treatment with hydroxyurea, decadron, and multiple rounds of radiation to the brain and spine. He was granted temporary respites from pain and neurologic deficits, only to have chloromas reappear like the infestation of a wicked weed, finding safe haven in the irradiated landscape stretching from his skull base to sacrum.
Manfred 'Manni' Segerer, a Patient with Refractory Idiopathic Hypereosinophilic Syndrome (HES).
Manfred 'Manni' Segerer, a Patient with Refractory Idiopathic Hypereosinophilic Syndrome (HES).
After the failure of three rounds of intensive chemotherapy, and development of recurrent pleural effusions, this self-taught electrical engineer headed to Stanford, carrying his grave prognosis and indomitable spirit across his tumor-riddled back like an overstuffed satchel. On January 22, 2002, Manfred “Manni” Segerer* (see Figure 1, online only) walked into our hematology clinic with his wife Shannon* to learn whether Dr. Stanley Schrier and I (then a 4th-year fellow) could deliver a therapeutic “Hail Mary.” Little did any of us appreciate that this encounter, like gravitational waves generating ripples in the curvature of space-time, would have lasting consequences that would touch patients for years to come.
At the time of our encounter with Manni, Stan and I heard that a few patients with refractory idiopathic hypereosinophilic syndrome (HES) at Mayo Clinic and MD Anderson Cancer Center were experiencing rapid and complete remissions with imatinib.1,2 We discussed Manni’s case with Dr. Ayalew Tefferi, and initiated imatinib 100 mg daily on an off-label basis. Within a few weeks, Manni felt substantially better, and his blood counts normalized; after three months of therapy, his bone marrow had been wiped clean of disease. We were stunned by the results; at our institution, Drs. Steven Coutre and Jim Malone subsequently treated another two patients with relapsed HES with similar dramatic outcomes. Similar observations were contemporaneously made by Drs. Dan DeAngelo and Rich Stone at Dana Farber Cancer Institute (DFCI). All of us who made these empiric leaps of faith with imatinib had witnessed similar responses in chronic myeloid leukemia (CML) and knew that something was amiss with one of its tyrosine kinase targets (e.g., ABL1, KIT, PDGFRA, or PDGFRB). We also knew that Dr. Gary Gilliland would be the perfect consignee of multiple institutions’ samples to pin down the answer. Led by postdoctoral researcher Dr. Jan Cools, the Gilliland group identified the FIP1L1-PDGFRA fusion tyrosine kinase, generated by an interstitial deletion on chromosome 4q12, as the molecular basis for response to imatinib.3 Arguably, the most important specimen in Dr. Cools’ rack of tubes was a July 2002 sample from Manni, who at that time began experiencing an agonizingly familiar back pain, just six months after commencing imatinib. His relapse was reminiscent of blast crisis CML, and the Gilliland team quickly discovered why: An imatinib-resistant PDGFRA T674I mutation had developed in the fusion gene—and was homologous to the common BCR-ABL1 T315I resistance mutation observed in CML and acute lymphocytic leukemia (ALL). Nature was consistent and cruel. Manni died in a few weeks’ time. He was a blazing comet that would leave an illuminating trail of stardust in its wake.
In 2003, Dr. Cools and colleagues published a murine model of myeloproliferative disease driven by FIP1L1-PDGFRA T674I.4 Imatinib failed in the mice as it did in Manni; however, the multikinase inhibitor midostaurin (PKC412; Novartis), which targets PKC, FLT3, VEGFR2, PDGFRA, PDGFRB, and KIT, reversed signs of disease and prolonged survival of the mice. This was the first demonstration in vivo that a structurally different tyrosine kinase inhibitor (TKI) could overcome resistance to another. A part of Manni lived on in these mice, and crystallized an important biologic paradigm that reached its full expression in imatinib-resistant CML and ALL patients who later derived benefit from second- and third-generation TKIs.
I pondered the implications of the Dr. Cools paper. My wife Lenn, a hematology nurse, recently reminded me of the moment when we were living in our Stanford West apartment and I rushed to her side with an epiphanous grin and a new elevator pitch. My idea was to test midostaurin in patients with advanced systemic mastocytosis (SM), a group of poorprognosis neoplasms in which more than 80 percent of cases harbor the imatinib-resistant KIT D816V mutation. If nature were indeed consistent, then midostaurin’s benefit in FIP1L1-PDGFRA T674I-positive disease could be recapitulated in SM, where no approved therapies existed. Neither of us realized that midostaurin was to emerge as “the other woman” who would co-opt our home life for the next 14 years.
In the spring of 2003, I shared my idea with Dr. Pam Cohen, head of Novartis’s midostaurin program. For more than a decade, the drug had been trialed in a variety of solid and liquid tumors, without any compelling hint of clinical activity. Around this time, Rich Stone had started his own journey of testing midostaurin in FLT3-mutated acute myeloid leukemia (AML), both as a single agent and in combination with chemotherapy. Pam acknowledged the logic of my hypothesis but was circumspect to move forward without supporting data. A few weeks after our conversation, a 48-year-old woman (N.S.) was transferred to the Stanford inpatient hematology service under the care of my colleague Dr. Caroline Berube. She presented with withering fatigue, diarrhea, liver function abnormalities, severe thrombocytopenia, hepatosplenomegaly with liver dysfunction, and hypoalbuminemia with weight loss. She was diagnosed with KIT D816V-positive mast cell leukemia with an associated unclassified myelodysplastic/myeloproliferative neoplasm (MCL+MDS/MPN-U). Knowing this patient was at death’s door, I contacted Gary Gilliland with the hope that he could provide pre-clinical data to substantiate treatment of this patient with midostaurin. In fact, Dr. Joe Growney in his lab had transformed Ba/F3 cells with KIT D816V and showed that the 50 percent inhibitory concentration (IC50) of midostaurin was 30 to 40 nM (concentrations achievable in vivo).5,6 In contrast, imatinib’s IC50 was >1 uM, confirming the mutation’s resistance to the drug.5,6 We conveyed these data to Pam, who, with the U.S. Food and Drug Administration (FDA), signed off on my petition for a singlepatient, compassionate-use protocol using midostaurin.
On June 20, 2003, N.S. became the first SM patient in the world to receive midostaurin. She achieved a partial response, with resolution of her liver dysfunction and portal vein thrombosis, disappearance of circulating mast cells, and a marked reduction of serum histamine levels.6 She was discharged home with a striking improvement in quality of life, taking joy in the most mundane of daily tasks. After three months, her SM was well controlled but her MDS/MPN transformed to secondary AML, betraying her progress and taking her life. However, we learned many lessons from N.S., which laid the foundation for further development of midostaurin in advanced SM. When she left this world, she hitched a ride on the tail of Manni’s comet at a time when it was gaining inevitable momentum.
In 2005, we initiated our investigator-initiated trial (IIT) of midostaurin with DFCI’s Dan DeAngelo, and Dr. Timothy Graubert, then at Washington University’s Siteman Cancer Center. Hematopathologist Dr. Tracy George, with whom I worked closely at Stanford, served as the central pathologist. Ultimately, it took us five years to accrue 26 patients from this rare disease population.7 In 2008, Tracy and I headed to Budapest to present our interim results at the annual meeting of European Competency Network in Mastocytosis (ECNM). This organization, led by Professor Peter Valent, represents the most authoritative group of lab-based and clinical mast cell disease researchers in the world. After Tracy and I presented our encouraging pathology and clinical trial data, we were peppered with enthusiastic questions. A palpable excitement spread throughout the conference. We knew this was a turning point.
Representatives from Novartis attended the Budapest meeting to finalize ongoing plans for a global trial of midostaurin in advanced SM. Along the banks of the Danube, European, North American, and Australian investigators came together to commit to the international trial, eventually numbering 29 sites. The year before, Tracy had travelled to the small town of Ansbach in central Bavaria to meet with Professor Hans-Peter Horny, the father of modern mast cell pathology.8 He had been recruited to be a central pathologist for the global study. At the microscope, Dr. Horny quizzed Tracy about her knowledge of mast cell disease diagnosis and pathology. She passed his interrogation and thereafter was recruited to evaluate samples from patients recruited at U.S. and Canadian sites, while Dr. Horny managed the review of European and Australian patients. Along with Horny and George, a Study Steering Committee (SSC) was convened with myself as Chairman, consisting of Professors Andreas Reiter, Hanneke Kluin-Nelemans, Cem Akin, Karin Hartmann, and Peter Valent. All was now in place to proceed. The trial accrued 116 patients from 2009 to 2013,9 and our SSC met on average every six months from 2008 to 2015 to adjudicate patient eligibility, histopathology, efficacy, and safety. The yearly ECNM conferences and lively discussions arising from our SSC meetings provided an incomparable education in mast cell disease and forged indelible relationships among us colleagues.
Shirley Baxter* came to Stanford from Plymouth, Minnesota, with a diagnosis of SM with chronic eosinophilic leukemia (SM-CEL). When she arrived on our doorstep in 2011, interferon had already failed to retard the ravaging effects of her disease. She was crippled by nausea, diarrhea, and severe malaise, as well as organ damage consisting of hypoalbuminemia with a 60-pound weight loss, hepatosplenomegaly, ascites, anemia, severe eosinophilia, and extensive cutaneous mastocytosis. Just before commencing the global trial in August of that year, she and her husband Bill* visited Yosemite and its historic Ahwahnee Hotel, ostensibly as a final sojourn to find peace and solitude in one of our country’s most glorious nature sanctuaries. Shirley Baxter would defy the odds. In 2015, she celebrated her 50th wedding anniversary, and in 2016, she made a triumphant return to Yosemite and the Ahwahnee (renamed the Majestic Yosemite). She was one of the 60 percent of responders on the study9 —in fact, a superresponder, with resolution of nearly all signs and symptoms of disease while maintaining good tolerance of midostaurin.
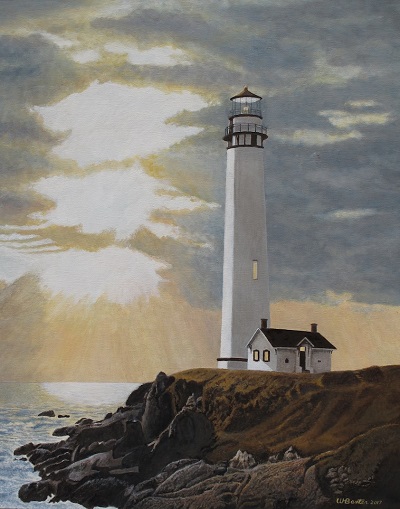
Based on the results of our IIT and the global study, midostaurin was approved by the FDA in April 2017.10 This past July, Shirley returned for her last visit to Stanford to transition to commercial drug supply, just short of six years on the trial. During a prior visit, Shirley and Bill travelled to the nearby Pigeon Point Lighthouse (see Figure 2), which was built in 1871 to help ships safely navigate the California coastline. When I view Bill’s painting of this landmark (see Figure above), I imagine that the heavenly light piercing the temperamental sky is the pending breach of Manni’s comet, returning to Earth in a gravity-defying orbit, eventually perching itself in the lantern room of the lighthouse. Tethered to his comet’s tail is N.S., our first SM patient treated with midostaurin, as well as L.R., who remained on our IIT for 11 years, only to succumb to acute leukemia just three months before FDA approval. Together,these souls light the path where Shirley and other survivors continue to walk the rocky promontory of their lives.
It’s hard to fathom all that has transpired in the 15 years since Manni visited our clinic. On a professional level, Stan still practices as he approaches his 89th birthday. I started as a senior fellow and recently advanced to the rank of Professor. On the home front, it’s well past time to let go of “the other woman” and make new elevator pitches to Lenn that engage our mutual interests. Shannon now lives in Nevada. She would be delighted to learn of the unforeseen bonds that link Manni to all of these patient warriors. While we all mark time by counting days, months, and years, it is impossible to know how time marks us for the accidental legacies we leave behind.
*Note: Permission was obtained to use the names of Manni and Shannon Segerer, as well as Shirley and Bill Baxter.
References
Competing Interests
Dr. Gotlib served as the Chairman of the Study Steering Committee for the global trial of midostaurin in advanced systemic mastocytosis; he received funding from Novartis to conduct the IIT and global trials of midostaurin. He has served on an advisory board and received honoraria from Novartis.