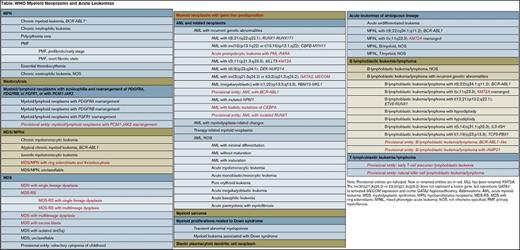
WHO table
The forthcoming 2016 revision of the WHO Classification of Tumours of the Hematopoietic and Lymphoid Tissues1 was recently previewed in two detailed summaries prepared by key members of the clinical advisory committee. The classification, last updated in 2008, now shows even more abundant evidence of the impact of genetic markers on diagnosis and disease management. This Mini Review is intended as a brief and high-level summary of some of the most critical and impactful changes associated with myeloid neoplasms (Table).
Myeloproliferative Neoplasms (MPNs)
First, chronic myeloid leukemia (CML), has undergone a nomenclature change, replacing “myelogenous” with “myeloid.” Second, it is noted that the presence of even low numbers of bona fide lymphoblasts should prompt concern for imminent blast phase. Third, revised criteria for diagnosing accelerated-phase (AP) CML have been proposed. Specifically, provisional “response to tyrosine kinase inhibitor (TKI)” criteria have been added to the definition of AP disease. These include 1) hematologic resistance to first TKI/failure to achieve a complete hematologic response to first TKI; 2) any hematologic, cytogenetic, or molecular indications of resistance to two sequential TKIs; or 3) occurrence of two or more mutations in BCR-ABL1 during TKI therapy. The clinical and laboratory characteristics that define AP CML have sometimes been considered vague, and often controversial. In the late 1980s, MD Anderson Cancer Center identified characteristics of CML acceleration that were associated with median survivals of less than 18 months.2,3 These criteria, which exist separately from the WHO criteria for AP CML, were subsequently incorporated into clinical trials, including those evaluating TKIs.4 It is unclear whether these new, provisional “response to TKI” criteria reflect the historical survivals of less than 18 months (since individuals meeting these criteria for TKI resistance may often live longer than 18 months), or whether a new conceptual framework for defining AP disease in the modern TKI era needs to be considered by clinicians and pathologists.
Chronic neutrophilic leukemia (CNL) now includes specific mention of CSF3R T618I or other activating CSF3R mutation as a major diagnostic criterion. Diagnosis is still permitted in the absence of this mutation if neutrophilia is present for three months with no identifiable cause or if another clonal finding is identified. (In contrast, the WHO notes that CSF3R mutations are uncommon in atypical CML [aCML], and if detected, should prompt review to exclude CNL. Conversely, a diagnosis of aCML is supported by SETBP1 and/or ETNK1 mutations, though these are not required for the diagnosis.)
Diagnostic criteria for polycythemia vera (PV) are notably changed to lower the hemoglobin threshold and thus prevent underdiagnosis. PV may now be diagnosed in patients with hemoglobin levels greater than 16.5 g/dL in males or 16 g/dL in females; or hematocrit greater than 49 percent in males or 48 percent in females. Bone marrow morphology is now considered a major diagnostic criterion, along with JAK2 V617F or exon 12 mutation. The rarely utilized, and primarily research-based endogenous erythroid colony (EEC) formation is no longer recognized. Despite the new emphasis on bone marrow morphology, a diagnosis of PV may still be rendered if patients meet the old (higher) hemoglobin threshold and show a JAK2 mutation, as well as a decreased serum erythropoietin level.
The diagnostic criteria for essential thrombocythemia now adds CALR and MPL mutations to JAK2 mutation as major findings, a change that also affects primary myelofibrosis (PMF). Additionally, the criteria for prefibrotic PMF, as opposed to overt PMF, are further clarified. For PMF specifically, additional mutations in ASXL1, EZH2, TET2, IDH1, IDH2, SRSF2, and SF3B1 are noted to be “of help in determining the clonal nature of the disease.”
Other major related changes include the removal of mastocytosis from the MPNs to its own major disease category, and the inclusion of the PCM1-JAK2 rearrangement characterized by t(8;9)(p22;q24.1) as a recurrent genetic finding in myeloid/lymphoid neoplasms associated with eosinophilia, similar to PDGFRA, PDGFRB, and FGFR1 rearrangements.
Myelodysplastic Syndrome (MDS)/MPN
In addition to the change described in the previous section for aCML, precise characterization of chronic myelomonocytic leukemia (CMML) is also updated, with a new CMML-0 category to describe cases with less than 2 percent blasts in the blood and less than 5 percent blasts in the bone marrow. A new diagnostic approach emphasizing genetic testing (including for PTPN11, KRAS, NRAS, NF1, and CBL) is also presented for juvenile myelomonocytic leukemia. “MDS/MPN with ring sideroblasts and thrombocytosis (MDS/MPN-RS-T)” is now an official (rather than provisional) entity, usually characterized by SF3B1 mutation, and replaces the prior name of refractory anemia with ring sideroblasts with thrombocytosis (RARS-T).
MDS
The new WHO classification removes descriptions of the cytopenic lineage (e.g., “refractory anemia”) in favor of a description of the dysplastic lineages (“MDS with single lineage dysplasia”). Erythroid-predominant cases no longer call for separate blast enumeration of the non-erythroid cells, a change that will result in the reclassification of most cases of acute erythroid leukemia, erythroid/myeloid type, as MDS. SF3B1 mutation, if present, permits a diagnosis of MDS with ring sideroblasts when as few as 5 percent ring sideroblasts are present. A diagnosis of MDS with isolated del(5q) may now be made if one additional cytogenetic abnormality is present, with the exception of monosomy 7 or del(7q). Finally, the detection of somatic gene mutations is specifically excluded as a diagnostic criterion for MDS, citing our evolving understanding of the phenomenon of clonal hematopoiesis of indeterminate potential.
Acute Myeloid Leukemia (AML)
A long-predicted change will require biallelic mutation of CEBPA to meet criteria for this recurrent genetic abnormality. De novo AML with BCR-ABL1 rearrangement is recognized as a new provisional entity with a targetable genetic change, and cases with RUNX1 (but without myelodysplastic-type cytogenetics) will be a provisional entity with worse prognosis. It is clarified that myelodysplastic morphologic changes alone do not exclude a diagnosis of AML with mutated NPM1 or CEBPA. Cases with germline mutations that predispose to the development of myeloid malignancies will be separately recognized. Finally, blastic plasmacytoid dendritic cell neoplasm is now an entity separate and distinct from AML.
In summary, these changes will drive diagnosis and therapy selection for many years to come. The reader is encouraged to consult the original article and the forthcoming classification for the complete details of our field’s new “blue bible.”
References
Competing Interests
Dr. Czuchlewski and Dr. George indicated no relevant conflicts of interest.