What is the differential diagnosis in a 35-year-old male with a lifelong history of easy bruising, epistaxis, and prolongation of both the prothrombin time (PT) and the activated partial thromboplastin time (APTT)? So began the evaluation by Dr. Shao-Qing Kuang et al. in the laboratory of Dr. Dianna Milewicz at the University of Texas Health Science Center in Houston, Texas.1 The family history revealed an autosomal bleeding disorder in an east Texas kindred consisting of 46 family members spanning four generations. Surprisingly, coagulation factor assays for fibrinogen and factors II, V, VII, VIII, IX, X, XI, and XII were normal. Linkage analysis demonstrated that the factor V (FV) gene (F5) mapped to the disease interval. Sequencing of the F5 gene revealed an A2440G mutation in exon 13 at position 2440, predicting a S756G mutation in the B domain of FV. However, because FV levels were normal, the mutation was considered an unlikely cause of the bleeding diathesis.
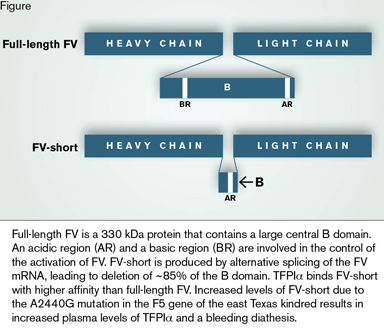
The cause of this mysterious bleeding disorder remained unknown for more than another decade until it was elucidated by Dr. Lisa Vincent and colleagues from the laboratories of Dr. Milewicz in Houston and Dr. Björn Dahlbäck of Lund University Hospital in Malmö, Sweden. The authors began by looking for abnormalities in the plasma FV in the kindred by Western blotting. Full-length FV is 330 kDa procofactor that is proteolytically activated by thrombin or factor Xa. During this process, the large, central B domain is removed (Figure). The product, FVa, is a heavy chain/light chain heterodimer that is a cofactor for factor Xa in the prothrombinase complex. Analysis of 36 family members revealed that in addition to full-length FV, plasma from affected family members contained a prominent ~250 kDa variant, which they named FV-short. FV-short was also identified in much smaller amounts in unaffected family members. RT-PCR analysis of whole blood from affected family members using primers spanning exon 13 identified an expected 2946 bp product and, additionally, large amounts of a smaller 840 bp product. The 840 bp fragment was also found in unaffected family members but, as with FV-short protein, in much smaller amounts. Sequencing of the 840 bp product revealed that the F5 gene variant produces an in-frame deletion of 2,106 base pairs, resulting in the deletion of nearly 85 percent of the B domain (Figure).
A thrombin generation assay was used as a potentially more sensitive method to detect abnormalities in the tissue factor-initiated extrinsic coagulation pathway in the kindred. Despite having normal coagulation factor levels, all affected family members demonstrated decreased thrombin generation. The addition of recombinant FV-short to immunodepleted FV-deficient plasma resulted in normal thrombin generation, indicating that the abnormality was not due to an intrinsic procoagulant defect in FV-short per se. However, addition of affected plasma to unaffected plasma resulted in decreased thrombin generation, revealing the presence of a coagulation inhibitor in affected plasma.
To identify the inhibitor, the authors took advantage of the recent discovery by Dr. Connie Duckers et al. that FV binds to tissue factor pathway inhibitor α (TFPIα).2 This finding was a result of the clinical observation that patients with severe FV deficiency often only have a mild bleeding disorder. This finding suggests that FV deficiency produces a secondary deficiency of a coagulation inhibitor with which it is associated. Dr. Duckers et al. made the key observation that plasma levels of TFPIα, a candidate coagulation inhibitor, is decreased in FV deficient individuals. They then demonstrated that TFPIα binds FV in a purified system.
These observations led Dr. Vincent et al. to the hypothesis that the inhibitor in affected family members is TFPIα and that the greater inhibitor activity must be a consequence of the high concentration of FV-short. The addition of anti-TFPIα antibodies to affected plasma increased thrombin generation to normal levels, indicating that TFPIα is the culprit producing the coagulant abnormality in the kindred. Furthermore, addition of anti-TFPIα antibodies to affected plasma removed FV-short, but not full-length FV, suggesting a stronger association of TFPIα with FV-short. This interpretation was confirmed by a semi-quantitative immunoprecipitation assay showing that TFPIα binds with higher affinity to FV-short than to full-length FV. The authors also found that TFPIα levels are increased several-fold in affected free, 40 kDa TFPIα is cleared by kidneys, and that this clearance is prevented when TFPIα is bound in a high-molecular-weight complex with FV or FV-short. Thus, the increased association of TFPIα with FV-short leads to higher plasma levels.
The authors speculated that the normal levels of FV and other coagulation factors in affected plasmas are due to the strong procoagulant stimulus in coagulation assays (tissue factor in the PT and activated partial thromboplastin in the APTT). Accordingly, the rapid production of high concentrations of Factor VIIa and Factor Xa would overwhelm TFPIα, even when its concentration is elevated in affected plasmas. In contrast, thrombin generation assays were performed in diluted plasma and at low concentrations of tissue factor, leading to more sensitive detection of a coagulant defect due to elevated levels of TFPIα.
The role of the large B domain in FV function has been enigmatic. Recently, Dr. Mettine H.A. Bos and Dr. Rodney M. Camire demonstrated that the B domain serves to maintain FV in an inactive, procofactor state.3 A basic region and an acidic region in the B domain have been identified that are necessary for this function (Figure). Interestingly, the basic region is not present in FV-short (Figure), which has implications for FV and TFPIα structure and function that remain to be investigated.
In Brief
An A2440G mutation in exon 13 of the F5 gene results in increased usage of an alternative splice-donor site, leading to production of a previously undetected protein, FV-short. Alternative splicing and expression of FV-short also occurs in the absence of the mutation, albeit to a lesser extent. TFPIα binds to full-length FV and FV-short, but with higher affinity to the latter. The association of TFPIα with FV-short reduces the clearance of TFPIα by preventing renal filtration. The resulting increase in TFPIα produces a bleeding diathesis due to an increased inhibition of Factor VIIa and Factor Xa. The results of this study have identified an important new mechanisms underlying FV and TFPIα biology in the regulation of coagulation.
References
Competing Interests
Dr. Lollar indicated no relevant conflicts of interest.