1. Clinical Fellow, Norris Cotton Cancer Center, Dartmouth-Hitchcock Medical Center, Lebanon, NH
2. Hematology/Oncology Fellowship Director, Scott & White Healthcare, Associate Professor of Medicine, Texas A&M HSC College of Medicine, Temple, TX
Diffuse large B-cell lymphoma (DLBCL) is one of the most common lymphoid malignancies worldwide. The incidence increases steeply with age with half of the cases occurring in patients older than 65 years. The elderly frequently have co-morbid conditions, rendering the intensive treatment required for cure inapplicable for many of them. Consequently, a treatment plan for an elderly patient can pose a challenge, but developing such a plan has significant educational value for hematology trainees.
Formulating a treatment plan for a patient with a hematologic disorder is a core medical-knowledge competency issue of hematology training. Prescribing cytotoxic chemotherapy should be regarded as an educational opportunity to be vigilantly taught, and trainee competency should be evaluated and tested on an ongoing basis. We suggest a methodical approach to conceiving, implementing, and adjusting a treatment plan to accompany patient engagement. We also suggest methods to evaluate and provide feedback to trainees based on level of training.
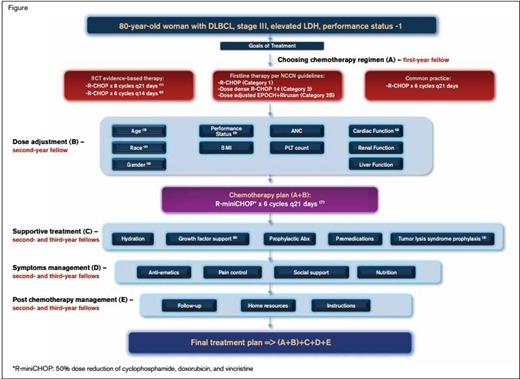
Example Treatment Plan. Treatment plan illustrating the case of an 80-year-old woman with advanced-stage DLBCL and a good performance status.
Example Treatment Plan. Treatment plan illustrating the case of an 80-year-old woman with advanced-stage DLBCL and a good performance status.
Let’s look at the case of an 80-year-old woman with advanced-stage DLBCL and a good performance status (Figure). Given her advanced age and the potential for treatment-related toxicity, it is imperative to clarify with the patient and her family the goals of care. Since elderly patients may have a good performance status, it is reasonable to discuss the use of cytotoxic chemotherapy with curative intent in this subset. The following steps are recommended to formulate a treatment plan.
Step 1: Choosing the chemotherapy regimen
The introduction of rituximab to the backbone of the CHOP regimen (cyclophosphamide, doxorubicin, vincristine, prednisone) for the treatment of DLBCL resulted in significantly better treatment outcomes in elderly patients (age 60-80) that included a 10 to 13 percent improvement in overall survival.1,2 The recommended frequency of chemotherapy cycles (every 14 vs. 21 days) and the number of cycles (6 vs. 8, respectively) can vary among treatment centers. The NCCN task force category 1 recommendation is for six cycles of R-CHOP. The data from the LNH03-6B GELA study suggest that a 21-day cycle (R-CHOP-21) trends toward higher efficacy and lower toxicity than a 14-day cycle in elderly patients, and although no randomized controlled trial has been done to compare the two, it is a common practice to use R-CHOP-21 for six cycles in DLBCL patients.
Step 2: Dose modification
Multiple factors affect treatment outcome in the elderly, including comorbidities, functional status, and support systems. Although age is an important prognostic factor in DLBCL, it should not be used as the sole criteria to determine eligibility for treatment. Over the last decade, geriatricians have developed tools for functional assessment that can be implemented for treatment decisions in cancer patients. Comorbidities can be assessed by the Cumulative Illness Rating Scale for Geriatrics (CIRS-G). This scoring system can help guide dose modification or inform about deletion of drugs that would improve tolerability (e.g., omitting vincristine in patients with neuropathy). The Activities of Daily Living (ADL) scale includes items that assess the performance of basic self-care activities (e.g., bathing). The Instrumental ADL (I-ADL) assesses higher levels of physical and cognitive function (e.g., shopping). ADL and I-ADL should be used to help determine dose modification and assessment of patient needs. A recent study showed that applying these scales in elderly patients with DLBCL to determine the chemotherapy regimen and dose adjustment was associated with a complete response rate of 81 percent.3
According to the National Cancer Database, the addition of rituximab was found to improve overall survival, but it demonstrated that racial and socio-economic disparities are likely affecting outcomes in elderly African-American patients.4 In addition, gender and weight can influence the metabolism of rituximab. Rituximab clearance is significantly reduced in females with half-life of 30 days compared with 24 days in males.5 This pharmacokinetic difference was associated with a decreased response in elderly men, and further studies need to clarify whether dose modification is needed for this population. Many elderly patients have decreased cardiac function that may limit the use of doxorubicin. Etoposide substitution for doxorubicin can achieve a similar response rate with decreased myocardial toxicity and should be considered in patients with mild to moderate myocardial impairment.3,6 Additional factors that should be taken into consideration when deciding on a treatment plan are decrease bone marrow function and altered drug metabolism due to aging. These factors are difficult to quantify and integrate, but they are the subject of ongoing research in this expanding population. A recent phase II study tested the R-miniCHOP regimen that includes upfront reduction by ~50 percent of the cytotoxic drugs cyclophosphamide, doxorubicin, and vincristine in fit patients older than 80 years of age.7 The overall response rate was 73 percent, and complete response or unconfirmed complete response rate was 62 percent. Treatment-related mortality was 8 percent, and the median survival was 29 months.
Step 3: Supportive care
Elderly patients are at an increased risk for treatment-related toxicity. Hematologic toxicity (primarily neutropenia and thrombocytopenia) is the most common adverse effect in these patients. The risk of febrile neutropenia and infection is greater in the elderly, resulting in unplanned hospitalization and suboptimal treatment delivery.8 The use of growth factor support and consideration of prophylactic antibiotics in high-risk patients can decrease the incidence of febrile neutropenia. Patients with DLBCL are at risk for tumor lysis syndrome, and elderly patients with poor renal function are particularly vulnerable. A careful hydration plan should be implemented, and prophylactic use of xanthine oxidase inhibitors (allopurinol), or recombinant urate oxidase (rasburicase) should be considered to prevent acute urate nephropathy.9
Step 4: Considering support systems
Malnutrition and lack of social support often influence treatment outcomes in the elderly and therefore should be part of the treatment plan, including the use of visiting nurses. Many centers have support groups that can help elderly patients cope with the emotional part of this difficult illness. Finally, detailed, written instruction and close follow-up can provide patients with the needed reassurance to cope with treatment-related toxicities.
The Teaching Perspective
The steps outlined above parallel a trainee’s development and competency in prescribing chemotherapy. Expert faculty members likely do not follow a step-by-step approach, but rather integrate the methodology unconsciously when seeing individual patients. However, it is necessary for faculty to break down the process when teaching novice hematologists. During the first year of hematology training, the task is to recognize standard therapy (step 1), and to learn from the parent speciality a completely different language. Frequent use of chemotherapy regimen books and NCCN guidelines should be encouraged. Intermediate trainees should incorporate supportive care practices and be able to recognize that guidelines and regimen books represent average populations and that individual patients require individualized approaches (steps 2-3). A senior trainee is preparing to enter unsupervised practice and should recognize the systems implications of care, including caregiver engagement and recruitment of multidisciplinary teams to share the management of special patient groups (step 4).
Fellows benefit from frequent feedback, ideally on a weekly basis. Prescription of chemotherapy in hematology is a high-risk and complex task. Competency in this area can and should be taught and evaluated in a systematic way. Why not present these general steps in the first continuity clinic and provide feedback with the first patient checkout? By recognizing and assessing treatment planning as a core medical-knowledge competency, we hope to improve patient care and the standard for teaching and evaluating fellows.
References
Competing Interests
Dr. Preis and Dr. Cable indicated no relevant conflicts of interest.