Invasive aspergillosis (IA) is a severe fungal infection that affects our most vulnerable populations. This includes patients having prolonged neutropenia, undergoing hematopoietic stem cell transplantation (HSCT), taking immunosuppressive agents (including newer monoclonal antibodies and small molecule agents), and having inherited or acquired immunodeficiencies.1 Incidences as high as 23 percent have been reported in the allogeneic HSCT population.2 Moreover, in recent decades the incidence of pulmonary IA has increased in many parts of the world due to an upsurge of immunocompromised patients. Global multinational prevalence estimates 250,000 cases of IA per year.3 Treatment of IA remains challenging, and the mortality rate remains high. Antifungal agents approved for the first-line treatment of IA include voriconazole, isavuconazole, and amphotericin B (lipid formulation).4,5 Furthermore, many international guidelines have recommended voriconazole as the preferred agent in this setting.6 Important toxicities associated with voriconazole are well known (e.g., neurotoxicity, visual disturbances) and are not uncommon, often causing premature cessation of this antifungal agent.7 Establishing the efficacy of a less-toxic and better-tolerated alternative first-line therapy is of significant clinical value.
Professor Johan A. Maertens and colleagues present a well-designed randomized, double-blind, controlled, noninferiority trial comparing posaconazole to voriconazole. The study used standard dosing for 12 weeks, in patient requiring primary treatment of IA, with the primary endpoint being cumulative all-cause mortality up to 42 days. The authors prespecified a 10 percent noninferiority margin. The primary endpoint was met in 44 participants in the posaconazole group (15%) and in 59 participants in the voriconazole group (21%), with a treatment difference of –5.3 percent (95% CI, –11.6 to 1.0; p<0.0001) in the intention-to-treat population. Because the upper limit of the 95% CI (1.0%) was less than 10 percent, the authors conclude that the study met the primary objective of demonstrating noninferiority of posaconazole. This result was further supported in the population with proven or probable IA only. Treatment-related adverse events were common and occurred in 86 participants in the posaconazole group (30%) and in 115 participants in the voriconazole group (40%), with a treatment difference of –10.2 percent (95% CI, –17.9 to –2.4). This led to discontinuation of study drug in 18 and 28 participants in the posaconazole and voriconazole groups, respectively (95% CI, –8.1 to 1.0). Three deaths due to treatment-related adverse events occurred, all in the voriconazole group. More patients in the voriconazole group experienced eye disorders (e.g., visual impairment, dyschromatopsia) and psychiatric disorders (e.g., hallucinations).
The clinical importance of the trial findings is significant. It reveals improved tolerability and less-frequent treatment discontinuation in patients receiving posaconazole. Toxicity, adverse events, and drug-drug interactions plague the current antifungal drug armamentarium. Up to 48 percent of patients receiving voriconazole may discontinue treatment due to side effects.7 Deaths have also been reported due to its toxicity. Use of the broad-spectrum antifungal amphotericin B is often avoided due to its deleterious effects on kidney function, which often causes difficulties in other crucial parts of patient management. Rates of acute kidney injury can be as high as 40 percent, which often prompts early cessation.8 Overall, poor treatment tolerance and discontinuity have been associated with inferior clinical outcomes and excess mortality, in addition to poor quality of life. The absence of reporting of therapeutic drug monitoring data from this study makes interpretation of excess triazole toxicity more difficult given its direct correlation with plasma trough concentrations. It remains possible, due to chance, that there was a higher mean plasma trough concentration in the voriconazole group, though unlikely given effective randomisation.
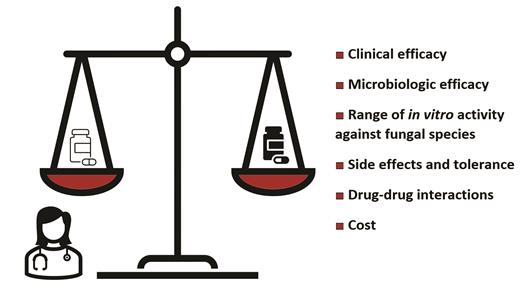
Posaconazole has a broader and more potent in vitro range of activity against mould species when compared to voriconazole. This includes activity against the Mucorales, Fusarium spp. Given the poor specificity in the diagnosis of IA in the possible and indeterminant categories (42% of the total study population) of the EORTC/MSG criteria, alternative fungal or bacterial pathogens may have resulted in infection in these groups. Inclusion of true infections due to Mucor spp., for example, would have resulted in fewer deaths in the posaconazole group and could partially explain the different primary endpoints between treatment groups. This highlights the significant limitations in fungal diagnostics that need to be addressed. Limitations of posaconazole do exist, including an increased cost to the health care service. Cost-benefit or economic analysis was not undertaken as a part of this study. Furthermore, both drugs inhibit activity of cytochrome P450 3A, leading to interactions with antileukemic drugs including venetoclax.
Weighing the risks and benefits of primary antifungal therapy for invasive aspergillosis.
Weighing the risks and benefits of primary antifungal therapy for invasive aspergillosis.
In Brief
In conclusion, this trial establishes the improved tolerance of posaconazole over voriconazole, with at least the same clinical efficacy in the treatment of IA. However, there were still 86 (30%) of 288 trial participants receiving posaconazole who experienced treatment-related adverse events, including 18 who had to discontinue therapy. Moreover, recently a rising incidence of triazole-resistance among invasive Aspergillus spp. has been recorded globally, often leading to clinical failures, breakthrough invasive fungal infection on prophylaxis, and death. Newer antifungal agents that are better tolerated, have fewer drug-drug interactions, and have potent activity against multidrug resistant fungal pathogens are required to further improve care of this vulnerable population.
Competing Interests
Dr. Stewart and Dr. Lane indicated no relevant conflicts of interest.