Study Title: A Phase 1b Dose Escalation Study Evaluating the Safety and Pharmacokinetics of Venetoclax in Combination with Azacitidine in Subjects with Treatment-Naïve Higher-Risk Myelodysplastic Syndromes (MDS)
CTN Number: NCT02942290
Sponsor: AbbVie, Inc.
Accrual Goal: Approximately 80 participants
Participating Centers: Approximately 30 sites globally
Study Design: This trial will enroll adults 18 years and older who have previously untreated de novo MDS with International Prognostic Scoring System (IPSS) risk categories intermediate-2 or high (i.e., minimum IPSS score of 1.5), less than 20 percent bone marrow blasts, Eastern Cooperative Oncology Group performance status of at most 2, currently ineligible for intensive chemotherapy or allogeneic hematopoietic stem cell transplantation (allo-HCT), and white blood cell count of at most 10,000/μL. Patients with therapy-related MDS or MDS/myeloproliferative neoplasm overlap will be excluded. Treatment will include standard azacitidine 75 mg/m2 for seven days either consecutively on days one to seven or with a two-day break (5-2-2) every 28 days, with venetoclax per dose level (100 mg, 200 mg, or 400 mg) on days 1 to 14, every 28 days. The study is designed to evaluate the safety and preliminary efficacy of the combination of venetoclax and azacitidine. Guided by a Bayesian optimal interval design, dose-escalation will occur at three dose levels. A safety expansion cohort will evaluate safety and efficacy at the preliminary recommended phase II dose (RP2D), and a second expansion cohort, if necessary, will evaluate alternative scheduling.
The primary objectives of the study are to 1) assess the safety profile and pharmacokinetics of venetoclax in combination with azacitidine and 2) determine the RP2D and dosing schedule of venetoclax in combination with azacitidine. Secondary objectives are to assess preliminary efficacy data including the overall response rate, duration of response, overall survival, and progression-free survival.
Rationale: Management of patients with higher-risk MDS remains challenging owing to the limited approved therapeutic options, median age of onset, and complex disease biology.1,2 This clonal disorder is characterized by a set of recurrently mutated genes involved in RNA splicing, epigenetic and traditional transcriptional regulation, and signal transduction.3 While cure can only be achieved by allo-HCT, disease-modifying therapies are necessary for effective cytoreduction and to minimize leukemic transformation. Frontline therapy for higher-risk MDS has been limited to hypomethylating agents and in some cases cytotoxic induction chemotherapy. Clinical trial strategies throughout the past decade have focused on using epigenetic targets and optimizing frontline chemotherapy regimens with novel agents. Despite advances in our genetic understanding of MDS, there has been little change to upfront management of higher-risk MDS. Small-molecule inhibitors of mutant isocitrate dehydrogenase enzymes, however, have some clinical activity for a minority of patients.4 Small-molecule spliceosome inhibitors5,6 and pharmacologic reactivation of mutant p537 are still being investigated.
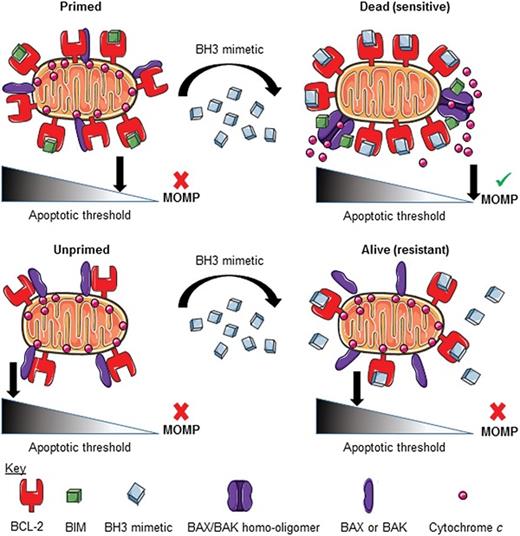
Incorporating novel agents into treatment with hypomethylating agents (HMAs) may be a more promising approach to improve outcomes for higher-risk MDS. Venetoclax is a selective, potent, orally bioavailable, small molecule inhibitor of B-cell lymphoma-2 (BCL-2) that promotes apoptosis by acting as a BH3 mimetic.8 The BH3 domain is found in all proapoptotic BCL-2 family of proteins. Venetoclax acts by displacing pro-apoptotic proteins such as BIM or BAX from BCL-2 to induce BAX- or BAK-dependent mitochondrial outer membrane permeabilization (MOMP), which commits the cell to apoptosis (Figure).9-11 This readiness to undergo apoptosis indicates how “primed” the tumor cells are for BCL-2 inhibition. Priming can be determined by the functional assay called BH3 profiling,12 which exposes the cancer cell’s mitochondria to synthetic BH3 peptides that mimic the proapoptotic function of BH3-only proteins to determine MOMP and apoptosis initiation. Results from BH3 profiling of myeloblasts correlated with clinical response to venetoclax in acute myeloid leukemia (AML).13
Although data are limited, two studies in AML support the use of venetoclax in MDS. In a phase II venetoclax monotherapy trial for relapsed/refractory AML, the complete remission (CR) plus CR with incomplete blood count recovery (CRi) rate was 19 percent (6 of 32 patients). Notably, half of these responders (3 of 6 patients) had an antecedent hematologic disorder. A second phase Ib study examined venetoclax in combination with the HMA azacitidine for the treatment of newly diagnosed AML in patients ineligible for intensive chemotherapy. The combination therapy resulted in a striking CR plus CRi rate of 73 percent in the venetoclax 400 mg plus HMA cohort, leading to the recent accelerated approval of the combination by the U.S. Food and Drug Administration.14 Although the number of patients with prior/underlying MDS was not explicitly reported, nearly a quarter of the subjects (36 of 145 patients) enrolled on the latter AML trial had a prior hematologic disorder and response rates did not differ among those with de novo and secondary AML. These practice-changing results raise the question of whether this combination has activity in related diseases such as MDS.
Though no dose-limiting toxicities including laboratory or clinical tumor lysis syndrome were reported in the AML setting,14 it comes as no surprise that hematologic and gastrointestinal adverse events (AEs) were common and expected giving the underlying disease and known AEs associated with HMA use.15 One concern about adding venetoclax to azacitidine in the MDS setting is the potential for prolonged neutropenia and associated infectious complications, which was reported in the phase Ib study of frontline venetoclax in combination with azacitidine for AML.14 To minimize the risk of febrile neutropenia complications, the current MDS study protocol was amended to reduce the duration of venetoclax exposure (continuous 14 days vs. 28 days) to allow for hematologic recovery. Furthermore, dose modifications were implemented to reduce the dose of venetoclax and azacitidine in the event of recurrent prolonged neutropenia. For these reasons, patients will be observed for infection-related complications and a second dose expansion was built to re-evaluate dosing and scheduling as needed once the optimal venetoclax dose is identified.
By using a combination approach in the upfront treatment of MDS that has been proven effective in secondary AML, this trial represents an effort to continue to reduce the number of patients who ultimately experience disease progression. It is anticipated that patients who were previously ineligible for allo-HCT might become eligible with disease modification and thus come off study treatment.
Comment: Results from this MDS trial are highly anticipated given the promising activity and known tolerability of the combination of venetoclax and azacitidine for the elderly population with AML. Though determining the safety and preliminary clinical efficacy of combining venetoclax with azacitidine is the critical question being addressed by this trial, testing the utility of BH3 mimetics across myeloid malignancies is of great interest given their large therapeutic window and lack of genotoxicity, which makes them great candidates for combination therapies. The issue of whether a more active combination therapy leads to survival benefit or delays leukemic transformation remains to be seen. This study is accruing well and on target to complete enrollment by the end of 2019.
Planned exploratory correlative studies to identify a biomarker of response include evaluation for the presence or absence of myeloid mutations and BCL-2 family molecular expression (protein or RNA). Recently, this study has cleared the initial dose-escalation phase and is accruing to the safety expansion cohorts. This trial represents a promising approach to improving outcomes for untreated MDS beyond the current standard of care.
References
Competing Interests
Dr. Garcia receives research funding from AbbVie, Pfizer, and Genentech. Dr. Letai received research support and consultation payment from Astra-Zeneca, Novartis, and AbbVie. He has served as a consultant for AbbVie, Genentech, and F. Hoffmann-La Roche and has received grants from AbbVie, Genentech, Eli Lilly, Cellectis, Calithera, Stemline, Threshold, Flexus, Biosciences, and Novartis. Dr. Kim indicated no relevant conflicts of interest.