Abstract
The field of graft-versus-host disease (GvHD) has experienced significant growth, with increased number of clinical trials and the approval of several agents by the US Food and Drug Administration for both acute and chronic GvHD treatment. In addition, the development of prognostic biomarker algorithms has enabled risk stratification in acute GvHD. However, prevention remains the cornerstone of GvHD management. Notable recent changes include the expansion of donor options with the increased use of haploidentical donor and unrelated donor transplantation, the development of ex vivo selective T-cell depletion strategies, recent approval by the Food and Drug Administration of abatacept for GvHD prevention, and the application of posttransplant cyclophosphamide in matched and mismatched donor settings. In this article, we review the results of recent clinical trials in GvHD prophylaxis and discuss the changes in clinical practice and promising emerging strategies driving the field forward.
Learning Objectives
The field of graft-versus-host disease prophylaxis is changing, with expanded options and effective approaches in matched and alternate donor transplantation
The choice of graft-versus-host disease prophylaxis should consider factors including donor availability, primary disease characteristics, and comorbidities
Introduction
The landscape of graft-versus-host disease (GvHD) prevention is undergoing significant changes from the standard previously accepted calcineurin inhibitor and methotrexate regimens. Posttransplant cyclophosphamide (PTCy) and the incorporation of novel agents have gained broad use across various donor types. Innovative graft manipulation techniques beyond CD34+ selection and CD3+ depletion now allow for GvHD prevention with more robust immune reconstitution. Furthermore, there has been an increase in haploidentical transplants and matched unrelated donor (MUD) options.1 This expansion of donor options, coupled with the introduction of new regimens for disease control and advancements in supportive care, has allowed a greater number of patients to undergo hematopoietic stem cell transplantation (HCT). This review primarily focuses on the evolving landscape of acute GvHD (aGvHD) prevention while acknowledging the vital role of donor selection in minimizing GvHD risk.2
CLINICAL CASE 1
A 61-year-old man with FLT3+ acute myeloid leukemia in complete remission is referred for HCT. He has no matched sibling donor options. There are several matched unrelated donors available. He underwent HCT with fludarabine and melphalan reduced intensity conditioning and PTCy, tacrolimus, and mycophenolate mofetil with a 10/10 matched peripheral blood stem cell (PBSC) graft. He did not develop acute GvHD and developed mild oral chronic GvHD at 8 months posttransplant, which was treated with topical steroids. He developed recurrent cytomegalovirus reactivation requiring antiviral therapy between days 60 and 150 posttransplant. At 1 year posttransplant, he remains in remission with no evidence of GvHD.
Posttransplant cyclophosphamide
The use of PTCy, paired with mycophenolate mofetil (MMF) and tacrolimus, has broadly expanded access to haploidentical donor grafts. In nonmyeloablative and reduced intensity conditioning (RIC) HCT, low rates of grade 3 to 4 aGvHD (7%-9%) and chronic GvHD (cGvHD; 26%-27%) have recently been observed with relapse rates ranging from 42% to 48%.3,4 Myeloablative conditioning (MAC) approaches have also been used with similarly low GvHD rates.5-7 In a prospective multicenter trial in children undergoing MAC haploidentical HCT with bone marrow grafts for hematologic malignancies, no grade 3 to 4 aGvHD was observed, and the incidence of moderate to severe cGvHD was 4%. However, there was a high rate of graft failure (16%), possibly linked to lower cell doses.8
Given the success in haploidentical donor transplants, PTCy has been examined in matched and mismatched donor HCT (Table 1). The Blood and Marrow Transplant Clinical Trials Network conducted a phase 2 randomized study, using RIC and incorporating 3 arms for GvHD prophylaxis including PTCy, with each arm compared to a contemporaneous control cohort using tacrolimus/methotrexate (Tac/MTX) prophylaxis.9 Results for the PTCy arm were superior, and thus the approach was tested in the phase 3 study (BMTCTN 1703) using RIC for hematologic malignancies. Most patients received a matched related or unrelated PBSC graft.10 Patients were randomized to receive either PTCy/MMF/tacrolimus or Tac/MTX GvHD prophylaxis. The PTCy arm had significantly lower grade 3 to 4 aGvHD (6% vs 15%) and 1-year cGvHD (22% vs 35%). The primary end point, GvHD (including grade 3-4 aGvHD and cGvHD requiring systemic immune suppression) and relapse-free survival at 1 year, was significantly improved with PTCy (53% vs 35%). Of note, lymphocyte count >1000 by 1 year was lower in the PTCy arm, with a significantly increased incidence of infections compared to Tac/MTX, consistent with previous studies showing delayed T-cell immune reconstitution11 and increased viral reactivations.12 While increased infections were observed with PTCy, the difference was driven by grade 2 and not grade 3 infections. In a phase 3 trial using MAC for hematologic malignancies with matched related or unrelated donors, patients were randomized to CD34+ selected PBSC graft, PTCy with bone marrow graft, and Tac/MTX with bone marrow graft as options for GvHD prevention (CTN 1301).13 Rates of severe aGvHD and cGvHD in with PTCy were 10% and 27%, respectively, comparable to the control arm. In a phase 2 single-center trial in adults and pediatrics, with PTCy/MMF/tacrolimus prophylaxis, patients underwent total body irradiation–based MAC, and the rate of severe aGvHD and cGvHD requiring systemic treatment were low at 6% and 6%, respectively. However, the overall rate of relapse was 39% (and higher in children).14
Representative GvHD prophylaxis trials using posttransplant cyclophosphamide, abatacept, and ATG in unrelated donor transplantation
| Trial/Reference . | Study design . | GvHD prophylaxis . | Acute GvHD . | Chronic GvHD . | Relapse . | Graft failure . | Survival . |
|---|---|---|---|---|---|---|---|
| Phase II Trial of Costimulation Blockade With Abatacept for Prevention of Acute GVHD (ABA2) Ref.16 | Phase: 2 N: MUD (142), MMUD (43) Recipient Age: >6 years Donor: MUD, MMUD Graft Source: PBSC, BM Conditioning: MAC or RIC | CNI/MTX Randomized ± abatacept (MUD) CNI/MTX/ abatacept (MMUD) | MUD Grade 2-4: 43% Grade 3-4: 7% MUD Control Grade 2-4: 62% Grade 3-4: 15% MMUD Grade 2-4: 40% Grade 3-4: 2% | MUD Mild-Sev: 52% Mod-Sev: 45%, MUD control Mild-Sev: 45% Mod-Sev: 36% MMUD Mild-Sev: 22% Mod-Sev: 58% | 2-y Relapse: MUD 22% MMUD 9% MUD control 24% | Secondary graft failure N = 1 (MUD) | MUD 2-y NRM: 13% 2-y EFS: 66% 2-y OS: 74% MUD control 2-y NRM: 16% 2-y EFS: 60% 2-y OS: 64% MMUD 2-y NRM: 17% 2-y EFS: 74% 2-y OS: 74% |
| Addition of Anti-Thymocyte Globulin to Standard Graft-Versus-Host Disease prophylaxis Versus Standard Treatment Alone in Patients With Haematological Malignancies Undergoing Transplantation From Unrelated Donors: Final Analysis of a Randomized, Open-Label, Multicentre, Phase 3 Trial Ref.33 | Phase: 3 N: 203 Recipient Age: 16-70 y Donor: MUD, MMUD Graft Source: PBSC, BM Conditioning: MAC or RIC | CNI/MTX Or CNI/MMF + Randomized ± ATG | ATG Grade 2-4: NA Grade 3-4: 28% Control Grade 2-4: NA Grade 3-4: 28% | ATG Mild-Sev: 26% Mod-Sev: NA Control Mild-Sev: 40% Mod-Sev: NA | 2-y Relapse: ATG 16% Control 18% | NA | ATG 2-y NRM: 21% 2-y EFS: NA 2-y OS: 71% Control 2-y NRM: 31% 2-y EFS: NA 2-y OS: 53% |
| Post-Transplantation Cyclophosphamide-Based Graft-Versus-Host Disease Prophylaxis (CTN 1703) Ref.10 | Phase: 3 N: 431 Recipient Age: >18 y Donor: MSD, MUD, MMUD Graft Source: PBSC Conditioning: RIC | PTCy/Tac/MMF Or Tac/MTX | PTCy/Tac/MMF Grade 2-4: 54% Grade 3-4: 6% Tac/MTX Grade 2-4: 52% Grade 3-4: 15% | PTCy/Tac/MMF Mild-Sev: 22% Mod-Sev: NA Tac/MTX Mild-Sev: 35% Mod-Sev: NA | PTCy/Tac/MMF 1-y Relapse: 21% Tac/MTX 1-y Relapse: 20% | PTCy/Tac/MMF 3% Tac/MTX | PTCy/Tac/MMF 1-y NRM: 12% 1-y EFS: 67% 1-y OS: 77% Tac/MTX 1-y NRM: 17% 1-y EFS: 62% 1-y OS: 72% |
| National Marrow Donor Program-Sponsored Multicenter, Phase II Trial of HLA-Mismatched Unrelated Donor Bone Marrow Transplantation Using Post-Transplant Cyclophosphamide (15-MMUD) Ref.15 | Phase: 2 N: 40 MAC, 40 RIC Recipient Age: 18-70 Donor: MMUD Graft Source: BM Conditioning: MAC or RIC | PTCy/Sirolimus/ MMF | Grade 2-4: 48% MAC, 35% RIC Grade 3-4: 20% MAC, 3% RIC | Mild-Sev: 36% MAC, 18% RIC Mod-Sev: NA | 1-y Relapse: 30% MAC, 23% RIC | 0% MAC, 8% RIC | 1-y NRM: 8% MAC, 10% RIC 1-y EFS: 62% MAC, 68% RIC 1-y OS: 72% MAC, 79% RIC |
| Three Prophylaxis Regimens (Tacrolimus, Mycophenolate Mofetil, and Cyclophosphamide; Tacrolimus, Methotrexate, and Bortezomib; or Tacrolimus, Methotrexate, and Maraviroc) Versus Tacrolimus and Methotrexate for Prevention of Graft-Versus-Host Disease With Haemopoietic Cell Transplantation With Reduced-Intensity Conditioning: A Randomised Phase 2 Trial With a Non-Randomised Contemporaneous Control Group (BMT CTN 1203) Ref.9 | Phase: 2 N: 273 (92 PTCy) Recipient Age: 18-75 y Donor: MSD, MUD, MMUD Graft Source: PBSC Conditioning: RIC | PTCy/Tac/MMF Or Tac/MTX/ Bortezomib Or Tac/MTX/ maraviroc | PTCy/Tac/MMF Grade 2-4: 27% Grade 3-4:2% Tac/MTX Grade 2-4: 30% Grade 3-4: 13% | PTCy/Tac/MMF Mild-Sev: 28% Mod-Sev: NA Tac/MTX Mild-Sev: 38% Mod-Sev: NA | PTCy/Tac/MMF 1-y Relapse: 28% Tac/MTX 1-y Relapse: 25% | PTCy/Tac/MMF 4% Tac/MTX 0 | PTCy/Tac/MMF 1-y NRM: 11% 1-y EFS: 60% 1-y OS: 71% Tac/MTX 1-y NRM: 16% 1-y EFS: 56% 1-y OS: 71% |
| Randomized Phase 3 BMT CTN Trial of Calcineurin Inhibitor–Free Chronic Graft-Versus-Host Disease Interventions in Myeloablative Hematopoietic Cell Transplantation for Hematologic Malignancies (CTN 1301) Ref.13 | Phase: 3 N: 346 Recipient Age: <65 y Donor: MSD, MUD Graft Source: BM, PBSC (CD34+ selection) Conditioning: MAC | Tac/MTX or PTCy Or none (CD34+ selection) | Tax/MTX Grade 2-4: 30% Grade 3-4:4% PTCy Grade 2-4: 38% Grade 3-4: 10% CD34+ selection Grade 2-4: 16% Grade 3-4: 3% | Tax/MTX Mild-Sev: NA Mod-Sev: 34% PTCy Mild-Sev: NA Mod-Sev: 27% CD34+ selection Mild-Sev: NA Mod-Sev: 9% | Tax/MTX 2-y Relapse: 26% PTCy 2-y Relapse: 14% CD34+ selection 2-y Relapse: 21% | Secondary graft failure Tax/MTX 1% PTCy 0% CD34+ selection 3% | Tax/MTX 2-y NRM: 8% 2-y EFS: 67% 2-y OS: 76% PTCy 2-y NRM: 16% 2-y EFS: 70% 2-y OS: 76% CD34+ selection 2-y NRM: 22% 1-y EFS: 57% 2-y OS: 60% |
| Phase II Study of Myeloablative 7-8/8-Matched Allotransplantation With Post-Transplantation Cyclophosphamide, Tacrolimus, and Mycophenolate Mofetil Ref.14 | Phase 2 N: 125 Recipient Age: median 39 y Donor: MUD, MMUD Graft Source: BM, PBSC Conditioning: MAC | PTCy/Tac/MMF | Grade 2-4: 17% Grade 3-4: 6% | Mild-Sev: NA Requiring IST: 6% | 2-y Relapse: 39% | NA | 2-y NRM: 10% 2-y EFS: 2-y OS: 74% |
| Trial/Reference . | Study design . | GvHD prophylaxis . | Acute GvHD . | Chronic GvHD . | Relapse . | Graft failure . | Survival . |
|---|---|---|---|---|---|---|---|
| Phase II Trial of Costimulation Blockade With Abatacept for Prevention of Acute GVHD (ABA2) Ref.16 | Phase: 2 N: MUD (142), MMUD (43) Recipient Age: >6 years Donor: MUD, MMUD Graft Source: PBSC, BM Conditioning: MAC or RIC | CNI/MTX Randomized ± abatacept (MUD) CNI/MTX/ abatacept (MMUD) | MUD Grade 2-4: 43% Grade 3-4: 7% MUD Control Grade 2-4: 62% Grade 3-4: 15% MMUD Grade 2-4: 40% Grade 3-4: 2% | MUD Mild-Sev: 52% Mod-Sev: 45%, MUD control Mild-Sev: 45% Mod-Sev: 36% MMUD Mild-Sev: 22% Mod-Sev: 58% | 2-y Relapse: MUD 22% MMUD 9% MUD control 24% | Secondary graft failure N = 1 (MUD) | MUD 2-y NRM: 13% 2-y EFS: 66% 2-y OS: 74% MUD control 2-y NRM: 16% 2-y EFS: 60% 2-y OS: 64% MMUD 2-y NRM: 17% 2-y EFS: 74% 2-y OS: 74% |
| Addition of Anti-Thymocyte Globulin to Standard Graft-Versus-Host Disease prophylaxis Versus Standard Treatment Alone in Patients With Haematological Malignancies Undergoing Transplantation From Unrelated Donors: Final Analysis of a Randomized, Open-Label, Multicentre, Phase 3 Trial Ref.33 | Phase: 3 N: 203 Recipient Age: 16-70 y Donor: MUD, MMUD Graft Source: PBSC, BM Conditioning: MAC or RIC | CNI/MTX Or CNI/MMF + Randomized ± ATG | ATG Grade 2-4: NA Grade 3-4: 28% Control Grade 2-4: NA Grade 3-4: 28% | ATG Mild-Sev: 26% Mod-Sev: NA Control Mild-Sev: 40% Mod-Sev: NA | 2-y Relapse: ATG 16% Control 18% | NA | ATG 2-y NRM: 21% 2-y EFS: NA 2-y OS: 71% Control 2-y NRM: 31% 2-y EFS: NA 2-y OS: 53% |
| Post-Transplantation Cyclophosphamide-Based Graft-Versus-Host Disease Prophylaxis (CTN 1703) Ref.10 | Phase: 3 N: 431 Recipient Age: >18 y Donor: MSD, MUD, MMUD Graft Source: PBSC Conditioning: RIC | PTCy/Tac/MMF Or Tac/MTX | PTCy/Tac/MMF Grade 2-4: 54% Grade 3-4: 6% Tac/MTX Grade 2-4: 52% Grade 3-4: 15% | PTCy/Tac/MMF Mild-Sev: 22% Mod-Sev: NA Tac/MTX Mild-Sev: 35% Mod-Sev: NA | PTCy/Tac/MMF 1-y Relapse: 21% Tac/MTX 1-y Relapse: 20% | PTCy/Tac/MMF 3% Tac/MTX | PTCy/Tac/MMF 1-y NRM: 12% 1-y EFS: 67% 1-y OS: 77% Tac/MTX 1-y NRM: 17% 1-y EFS: 62% 1-y OS: 72% |
| National Marrow Donor Program-Sponsored Multicenter, Phase II Trial of HLA-Mismatched Unrelated Donor Bone Marrow Transplantation Using Post-Transplant Cyclophosphamide (15-MMUD) Ref.15 | Phase: 2 N: 40 MAC, 40 RIC Recipient Age: 18-70 Donor: MMUD Graft Source: BM Conditioning: MAC or RIC | PTCy/Sirolimus/ MMF | Grade 2-4: 48% MAC, 35% RIC Grade 3-4: 20% MAC, 3% RIC | Mild-Sev: 36% MAC, 18% RIC Mod-Sev: NA | 1-y Relapse: 30% MAC, 23% RIC | 0% MAC, 8% RIC | 1-y NRM: 8% MAC, 10% RIC 1-y EFS: 62% MAC, 68% RIC 1-y OS: 72% MAC, 79% RIC |
| Three Prophylaxis Regimens (Tacrolimus, Mycophenolate Mofetil, and Cyclophosphamide; Tacrolimus, Methotrexate, and Bortezomib; or Tacrolimus, Methotrexate, and Maraviroc) Versus Tacrolimus and Methotrexate for Prevention of Graft-Versus-Host Disease With Haemopoietic Cell Transplantation With Reduced-Intensity Conditioning: A Randomised Phase 2 Trial With a Non-Randomised Contemporaneous Control Group (BMT CTN 1203) Ref.9 | Phase: 2 N: 273 (92 PTCy) Recipient Age: 18-75 y Donor: MSD, MUD, MMUD Graft Source: PBSC Conditioning: RIC | PTCy/Tac/MMF Or Tac/MTX/ Bortezomib Or Tac/MTX/ maraviroc | PTCy/Tac/MMF Grade 2-4: 27% Grade 3-4:2% Tac/MTX Grade 2-4: 30% Grade 3-4: 13% | PTCy/Tac/MMF Mild-Sev: 28% Mod-Sev: NA Tac/MTX Mild-Sev: 38% Mod-Sev: NA | PTCy/Tac/MMF 1-y Relapse: 28% Tac/MTX 1-y Relapse: 25% | PTCy/Tac/MMF 4% Tac/MTX 0 | PTCy/Tac/MMF 1-y NRM: 11% 1-y EFS: 60% 1-y OS: 71% Tac/MTX 1-y NRM: 16% 1-y EFS: 56% 1-y OS: 71% |
| Randomized Phase 3 BMT CTN Trial of Calcineurin Inhibitor–Free Chronic Graft-Versus-Host Disease Interventions in Myeloablative Hematopoietic Cell Transplantation for Hematologic Malignancies (CTN 1301) Ref.13 | Phase: 3 N: 346 Recipient Age: <65 y Donor: MSD, MUD Graft Source: BM, PBSC (CD34+ selection) Conditioning: MAC | Tac/MTX or PTCy Or none (CD34+ selection) | Tax/MTX Grade 2-4: 30% Grade 3-4:4% PTCy Grade 2-4: 38% Grade 3-4: 10% CD34+ selection Grade 2-4: 16% Grade 3-4: 3% | Tax/MTX Mild-Sev: NA Mod-Sev: 34% PTCy Mild-Sev: NA Mod-Sev: 27% CD34+ selection Mild-Sev: NA Mod-Sev: 9% | Tax/MTX 2-y Relapse: 26% PTCy 2-y Relapse: 14% CD34+ selection 2-y Relapse: 21% | Secondary graft failure Tax/MTX 1% PTCy 0% CD34+ selection 3% | Tax/MTX 2-y NRM: 8% 2-y EFS: 67% 2-y OS: 76% PTCy 2-y NRM: 16% 2-y EFS: 70% 2-y OS: 76% CD34+ selection 2-y NRM: 22% 1-y EFS: 57% 2-y OS: 60% |
| Phase II Study of Myeloablative 7-8/8-Matched Allotransplantation With Post-Transplantation Cyclophosphamide, Tacrolimus, and Mycophenolate Mofetil Ref.14 | Phase 2 N: 125 Recipient Age: median 39 y Donor: MUD, MMUD Graft Source: BM, PBSC Conditioning: MAC | PTCy/Tac/MMF | Grade 2-4: 17% Grade 3-4: 6% | Mild-Sev: NA Requiring IST: 6% | 2-y Relapse: 39% | NA | 2-y NRM: 10% 2-y EFS: 2-y OS: 74% |
BM, bone marrow; CNI, calcineurin inhibitor; EFS, event-free survival; IST, immunosuppressive treatment; Mod, moderate; MSD, matched sibling donor; NA, not available; NRM, nonrelapse mortality; OS, overall survival; Sev, severe.
A phase 2 study also recently evaluated PTCy in mismatched unrelated donor (MMUD) transplant (including <7/8 human leukocyte antigen [HLA] matched donors) where it was added to sirolimus and MMF in patients receiving MAC or RIC. Grade 2 to 4 and 3 to 4 aGvHD was 47.5% and 20% in the MAC setting and 35% and 2.5% in the RIC, respectively. One-year cGvHD incidence was 36% and 18% in MACs and RICs, respectively.15 The follow-up study (NCT04904588) in MMUD transplant (≤7/8 HLA matched) examines this approach in adults receiving PBSC graft following MAC, adults receiving a PBSC graft following a nonmyeloablative or RIC regimen, and children receiving bone marrow grafts following a MAC regimen.
Alternate donor and GvHD prophylaxis considerations
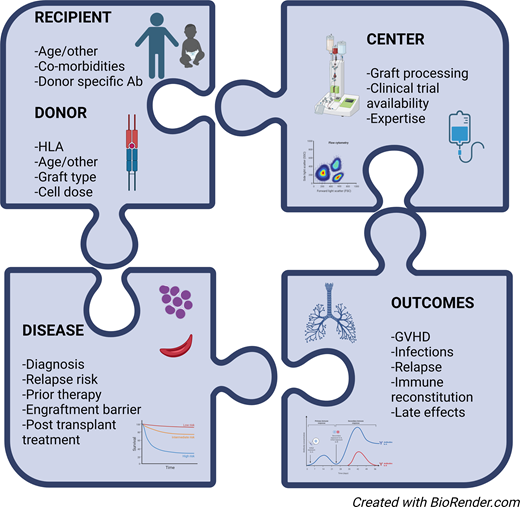
In the absence of a matched donor, there are 2 primary options, MMUD or haploidentical donors. The choice between the options must be considered within the context of planned GvHD prophylaxis and should take into consideration other donor and recipient characteristics, an overall assessment of GvHD and disease relapse risks, and center resources and experience, including the capabilities for graft selection, and the availability of clinical trials.
A haploidentical donor with PTCy is an option that is favored by many centers and is associated with low rates of GvHD but has been associated with delayed immune reconstitution and increased infection risk. Abatacept was recently approved by the US Food and Drug Administration (FDA) for GvHD prevention in MUD and MMUD HCT and is associated with low rates of severe aGvHD, robust immune reconstitution, and engraftment but is not effective in preventing cGvHD. Antithymocyte globulin (ATG) has been a commonly used approach in the prevention for GvHD but appears to have a greater impact on cGvHD than aGvHD (Table 1). Graft manipulation is an option and is associated with the low rates of GvHD, but few centers have the expertise or resources needed. There are also several emerging strategies that have shown promise in GvHD prevention offered in the context of a clinical trial.
CLINICAL CASE 2
A 17-year-old girl with acute myeloid leukemia and end of induction minimal residual disease (MRD) positive is referred for HCT. Her mother is 44 years old and is in good health. She has no MUD options, but several 9/10 MMUDs <35 years of age. She has good organ function and has tolerated therapy well. Disease evaluation was positive for 0.01% MRD prior to HCT. The patient underwent busulfan and fludarabine myeloablative conditioning and GvHD prophylaxis with tacrolimus, methotrexate, and abatacept and a 9/10 HLA-matched unrelated bone marrow graft. She developed stage 1 skin aGvHD treated with topical triamcinolone. She was diagnosed with moderate cGvHD of the skin at 8 months post-HCT and required systemic therapy with sirolimus and short-course prednisone. She is 1 year post-HCT in MRD-negative remission, GvHD is quiescent, and she remains on sirolimus.
Abatacept
T-cell costimulation pathways play an integral role in T-cell activation and the GvHD response. Abatacept blocks the CD28-CD80/86 interaction and prevents T-cell activation. The efficacy of abatacept for prevention of severe aGvHD was tested in a phase 2 multicenter trial in MUD and MMUD transplantation. In MMUD HCT, the addition of abatacept to calcineurin inhibitor and methotrexate in patients with hematologic malignancies receiving MAC or RIC conditioning was effective in preventing severe aGvHD (with a low observed incidence of 2%) and improved day 180 severe aGvHD-free survival of 98%, both significantly lower than control cohorts receiving calcineurin inhibitor/methotrexate alone or with ATG.16 Day 180 severe aGvHD-free survival was significantly better in MUD HCT with abatacept compared to placebo (93% vs 82%), with lower incidence of severe aGvHD in patients receiving abatacept (15% vs 7%). The additional immune suppression did not result in increased relapse or severe infections or delay in immune reconstitution. The abatacept phase 2 study findings were validated in real-world analyses, comparing abatacept to calcineurin inhibitor/MTX in MUD and in MMUD.17,18 The results for MMUD transplantation using abatacept for prophylaxis were similar to MUD using standard calcineurin inhibitor and methotrexate (compared among trial arms and in real-world analysis) in all survival outcomes, including nonrelapse mortality, overall survival, relapse-free survival, and GvHD-free survival.18,19 Studies incorporating abatacept in GvHD prophylaxis for nonmalignant hematologic diseases were recently reported, with similarly promising results.20,21 The 4-dose regimen of abatacept did not effectively prevent the development of cGvHD, and ongoing trials (NCT03924401, NCT04380740) are examining the use of extended-dose abatacept for this purpose.
Ex vivo graft manipulation
The 3- to 4-log reduction in T cells through ex vivo CD34+ cell enrichment effectively prevents GvHD in related and unrelated donor transplantation. Earlier approaches with CD34+ selection or CD3+ depletion were hampered by increased infections and increased nonrelapse mortality. In BMTCTN1301, moderate to severe cGvHD-free, relapse-free survival was 50% for CD34+ selection, 48% for PTCy, and 41% for Tac/MTX. While CD34+ selection had lower rates of GvHD, nonrelapse mortality was inferior, attributed to increased infection and organ failure.13
Selective ex vivo depletion of specific T-cell populations has been investigated as a strategy for preventing GvHD while improving immune reconstitution (Table 2).22-28 Alpha beta T-cell receptor depletion can protect against GvHD, while retaining gamma delta T cells and natural killer cells, resulting in a low incidence of GvHD. ATG is usually included in the conditioning regimen. The approach is combined with CD19+ depletion, which may further prevent GvHD and also protect against posttransplant lymphoproliferative disorder. In a recent study in children and adults,24 the incidence of aGvHD was 10%, and moderate to severe cGvHD was 21%, with findings reproduced in multicenter experiences.29 Alternatively, naive T-cell (CD45RA+) depletion offers another approach that selectively removes naive T cells that contribute to GvHD development while retaining memory T cells, which enhance antiviral immunity. In a single-center study, CD45RA+ depletion combined with CD34+ selection in adults with hematologic malignancies had low severe acute and chronic GvHD (4% and 7%, respectively) and rapid T-cell recovery, with similar results for patients receiving matched sibling and MUD grafts.25 The generalizability of these techniques is limited by the required resources, including cost, equipment, staff training, and regulatory burden.26 In addition, in adults, cell dose constraints often require an additional CD34+ selected graft infusion, further adding to the donor burden and center resource requirements. The success of ex vivo selective T-cell depletion has been the basis for further donor graft engineering, with the aim to enrich immunoregulatory populations. A recent study used a combined approach of CD34+ selected cell infusion with a high-purity Treg infusion, followed by a conventional T-cell infusion with set Treg/Tcon ratios (Orca-T) in MRD and MUD. The results from the single-institution and multi-institution studies demonstrate low risk of both severe aGvHD and moderate to severe cGvHD at 5% and 6%, respectively.30,31
Representative graft manipulation trials for GvHD prophylaxis in patients undergoing stem cell transplantation for hematologic malignancies
| Approach . | Study design . | GvHD prophylaxis . | Acute GvHD . | Chronic GvHD . | Relapse . | Graft failure . | Survival . |
|---|---|---|---|---|---|---|---|
| Tn-depleted PBSC + CD34+-selected PBSC Ref.25 | Phase: 2 N: 138 Recipient Age: 1-60 y Donor: MRD, MUD Conditioning: MAC | Tac Tac/MTX Tac/MMF | Grade 2: 71% Grade 3-4: 4% | Mild-Sev:6% Mod-Sev:1% | 3-y Relapse: 23% | Primary graft failure: 0 Secondary graft failure: N = 2 | 3-y NRM: 8% 3-y EFS: 69% 3-y OS: 77% |
| TCRab-depleted/ CD19-depleted PBSC Ref.27 | Phase: 2 N: 60 Recipient Age: >20 y Donor: Haplo Conditioning: MAC | CSA | Grade 2-4: 34% Grade 3-4: N = 18 | Mild-Sev: 25% Mod-Sev: N = 12 | Median follow-up 28 months Relapse 27% | Primary graft failure N = 4 | Median follow-up 28 months NRM: 23% EFS: 52% OS: NA |
| ORCA-T Manufactured cellular therapy with stem cells and Tregs Ref.31 | Phase: 1b, 2 N: 127 Recipient Age: 19-69 y Donor: MRD, MUD Conditioning: MAC | Tac or sirolimus | Grade 2-4: NA Grade 3-4: 5% | Mild-Sev: NA Mod-Sev: 6% | Relapse: NA | Primary graft failure 2% | 1-y NRM:5% 1.5-y EFS: 81% 1.5-y OS: 86% |
| CD34+-selected PBSC graft + Tn-depleted PBSC graft Ref.23 | Phase: NA N: 25 Recipient Age: 2-17 y Donor: Haplo Conditioning: MAC | CSA = 3 CSA/MTX = 1 MMF = 21 | Grade 2-4: 39% Grade 3-4: 33% | Mild-Sev: 22% Mod-Sev: N = 2 | 2.5-y Relapse: 17% | Primary graft failure: 0 Secondary graft failure: N = 2 | 2.5-y NRM: 22% EFS: NA 2.5-y OS: 58% |
| TCRab-depleted PBSC graft Ref.28 | Phase: 1/2 N: 35 Recipient Age: 19-69 y Donor: MRD, MUD, MMUD Conditioning: MAC | ATG MMF | Grade 2-4: 26% Grade 3-4: 14% | Mild-Sev: 23% Mod-Sev: 17% | 2-y Relapse: 29% | Primary graft failure: 0 Secondary graft failure: N = 1 | 2-y NRM: 32% 2-y EFS: 40% 2-y OS: 54% |
| TCRab-depleted/ CD19-depleted PBSC graft Ref. 22 | Phase: NA N: 60 Recipient Age: 1-23 y Donor: MUD, MMUD Conditioning: MAC | ATG = 22 | Grade 2-4: NA Grade 3-4: 13% | Mild-Sev: 26% Mod-Sev: NA (Extensive 11%) | Median follow-up 3.1 y Relapse: 21% | Primary graft failure: 1 | 3-y NRM: 15% 4-y EFS: 64% 4-y OS: 69% |
| TCRab-depleted/ CD19-depleted PBSC graft Ref.24 | Phase: 1/2 N: 60 Recipient Age: 1-63 y Donor: Haplo Conditioning: RIC | MMF ± ATG | Grade 2-4: 10% Grade 3-4: 0% | Mild-Sev: 31% Mod-Sev: 21% | 2-y Relapse: 21% | Primary graft failure: 9 | 2-y NRM: 17% 2-y EFS: 50% 2-y OS: 63% |
| Approach . | Study design . | GvHD prophylaxis . | Acute GvHD . | Chronic GvHD . | Relapse . | Graft failure . | Survival . |
|---|---|---|---|---|---|---|---|
| Tn-depleted PBSC + CD34+-selected PBSC Ref.25 | Phase: 2 N: 138 Recipient Age: 1-60 y Donor: MRD, MUD Conditioning: MAC | Tac Tac/MTX Tac/MMF | Grade 2: 71% Grade 3-4: 4% | Mild-Sev:6% Mod-Sev:1% | 3-y Relapse: 23% | Primary graft failure: 0 Secondary graft failure: N = 2 | 3-y NRM: 8% 3-y EFS: 69% 3-y OS: 77% |
| TCRab-depleted/ CD19-depleted PBSC Ref.27 | Phase: 2 N: 60 Recipient Age: >20 y Donor: Haplo Conditioning: MAC | CSA | Grade 2-4: 34% Grade 3-4: N = 18 | Mild-Sev: 25% Mod-Sev: N = 12 | Median follow-up 28 months Relapse 27% | Primary graft failure N = 4 | Median follow-up 28 months NRM: 23% EFS: 52% OS: NA |
| ORCA-T Manufactured cellular therapy with stem cells and Tregs Ref.31 | Phase: 1b, 2 N: 127 Recipient Age: 19-69 y Donor: MRD, MUD Conditioning: MAC | Tac or sirolimus | Grade 2-4: NA Grade 3-4: 5% | Mild-Sev: NA Mod-Sev: 6% | Relapse: NA | Primary graft failure 2% | 1-y NRM:5% 1.5-y EFS: 81% 1.5-y OS: 86% |
| CD34+-selected PBSC graft + Tn-depleted PBSC graft Ref.23 | Phase: NA N: 25 Recipient Age: 2-17 y Donor: Haplo Conditioning: MAC | CSA = 3 CSA/MTX = 1 MMF = 21 | Grade 2-4: 39% Grade 3-4: 33% | Mild-Sev: 22% Mod-Sev: N = 2 | 2.5-y Relapse: 17% | Primary graft failure: 0 Secondary graft failure: N = 2 | 2.5-y NRM: 22% EFS: NA 2.5-y OS: 58% |
| TCRab-depleted PBSC graft Ref.28 | Phase: 1/2 N: 35 Recipient Age: 19-69 y Donor: MRD, MUD, MMUD Conditioning: MAC | ATG MMF | Grade 2-4: 26% Grade 3-4: 14% | Mild-Sev: 23% Mod-Sev: 17% | 2-y Relapse: 29% | Primary graft failure: 0 Secondary graft failure: N = 1 | 2-y NRM: 32% 2-y EFS: 40% 2-y OS: 54% |
| TCRab-depleted/ CD19-depleted PBSC graft Ref. 22 | Phase: NA N: 60 Recipient Age: 1-23 y Donor: MUD, MMUD Conditioning: MAC | ATG = 22 | Grade 2-4: NA Grade 3-4: 13% | Mild-Sev: 26% Mod-Sev: NA (Extensive 11%) | Median follow-up 3.1 y Relapse: 21% | Primary graft failure: 1 | 3-y NRM: 15% 4-y EFS: 64% 4-y OS: 69% |
| TCRab-depleted/ CD19-depleted PBSC graft Ref.24 | Phase: 1/2 N: 60 Recipient Age: 1-63 y Donor: Haplo Conditioning: RIC | MMF ± ATG | Grade 2-4: 10% Grade 3-4: 0% | Mild-Sev: 31% Mod-Sev: 21% | 2-y Relapse: 21% | Primary graft failure: 9 | 2-y NRM: 17% 2-y EFS: 50% 2-y OS: 63% |
CSA, cyclosporine; haplo, haploidentical; Tn, naive T cells; TCRab, αβ + T cells; Tregs, regulatory T cells.
Antithymocyte globulin
ATG results in antibody-mediated destruction of T cells and has been widely used for the prevention of GvHD when combined with a calcineurin inhibitor and methotrexate or MMF. There are multiple preparations of ATG (horse and rabbit derived) with differing degrees of lymphodepletion and half-life, with rabbit ATG being the most commonly used for GvHD prevention.32 A recent randomized phase 3 trial of adults receiving MUD or MMUD transplant with rabbit ATG, calcineurin inhibitor, and methotrexate or MMF showed no difference in grade 3 to 4 aGvHD, but a significant improvement was observed in cGvHD (26% with ATG vs 41% with standard prophylaxis). There was no difference in relapse and nonrelapse mortality at 16% vs 17% and 21% vs 31% in the ATG and standard prophylaxis groups, respectively.33 A retrospective analysis from the European Society for Blood and Marrow Transplantation registry comparing ATG with PTCy in haploidentical transplant did not show a difference in GvHD, but the ATG group had an increased risk of relapse and lower leukemia-free survival and overall survival compared to ATG.34 Alemtuzumab (humanized anti-CD52 antibody) also results in antibody-mediated destruction of lymphocytes and has been shown to be effective in the prevention of acute and chronic GvHD.35
Emerging strategies and ongoing trials
New approaches to the prevention of aGvHD have recently shown promise, with several ongoing trials (Table 3). These trials encompass repurposing of drugs from other diseases and indications, including FDA-approved agents such as sitagliptin and alpha-1 antitrypsin, the extension of drugs with efficacy in GvHD treatment to prevention such as ruxolitinib, and testing of novel combinations to optimize the prevention of both acute and chronic GvHD such as combinations of abatacept and PTCy.
Ongoing phase 2/3 clinical trials for GvHD prophylaxis
| Trial . | Agents/approach . | Study design . | Study population . |
|---|---|---|---|
| A Randomized Double-Blind Trial of Abatacept Extended Dosing Versus Abatacept Short-Term Dosing for GVHD Prophylaxis (ABA3) NCT04380740 | Abatacept, CNI/MTX Extending dosing of abatacept for GvHD prevention | Phase: 2 N: 160 | Disease: Malignant Recipient Age: >2 y Donor: MUD/MMUD Graft Source: PBSC or BM Conditioning: MAC/RIC |
| Acute GVHD Suppression Using Costimulation Blockade to Expand Non-malignant Transplant (ASCENT) NCT03924401 | Abatacept, CNI/MTX Extended dosing of abatacept for GvHD prevention | Phase: 2 N: 30 | Disease: Nonmalignant Recipient Age: 0-20 y Donor: MUD/MMUD Graft Source: PBSC or BM Conditioning: MAC/RIC |
| Cyclophosphamide, Abatacept, and Tacrolimus for the Prevention of GVHD NCT05621759 | PTCy, Abatacept, short-course tacrolimus | Phase: 2 N: 92 | Disease: Malignant Recipient Age: >18 y Donor: Haploidentical Graft Source: PBSC Conditioning: MAC/RIC |
| Optimizing PTCy Dose and Timing NCT03983850 | PTCy, Sirolimus, MMF Reduced-dose PTCy | Phase: 1/2 N: 400 | Disease: Malignant Recipient Age: >12 y Donor: Haploidentical Graft Source: BM or PBSC Conditioning: MAC |
| HLA-Mismatched Unrelated Donor Hematopoietic Cell Transplantation With Post-Transplantation Cyclophosphamide (ACCESS) NCT04904588 | PTCy, Tacrolimus, MMF | Phase: 2 N: 300 | Disease: Malignant Recipient Age: >1 y Donor: MMUD Graft Source: PBSC, BM Conditioning: MAC, RIC, NMA |
| A Randomized Pilot Trial Comparing Anti-Thymocyte Globulin (ATG) With ATG Plus Post Transplant Cyclophosphamide (PTCy) for Prophylaxis Against Acute and Chronic Graft Versus Host Disease NCT04202835 | ATG ± PTCy | Phase 2 N: 80 | Disease: Malignant Recipient Age: 16-70 y Donor: MRD, MUD Graft Source: PBSC Conditioning: MAC, RIC |
| A Phase II Pediatric Study of GVHD Prophylaxis Regimen With No Calcineurin Inhibitors After Day +60 Post First Allogeneic Hematopoietic Cell Transplant for Hematological Malignancies NCT05579769 | CNI/MTX, Ruxolitinib ± ATG | Phase: 2 N: 32 | Disease: Malignant Recipient Age: >12 y Donor: MRD, MUD Graft Source: BM Conditioning: MAC |
| Bendamustine With or Without Cyclophosphamide in Preventing GVHD in Patients Undergoing Stem Cell Transplant NCT04022239 | Bendamustine, Tac, MMF, ± PTCy Posttransplant bendamustine | Phase: 1/2 N: 40 | Disease: Malignant Recipient Age: 18-70 y Donor: MMUD, Haploidentical Graft Source: NA Conditioning: RIC |
| Tocilizumab for the Prevention of Graft Failure and GVHD in Haplo-Cord Transplantation NCT04395222 | Tocilizumab, ± ATG Tocilizumab day −1 | Phase: 2 N: 70 | Disease: Malignant Recipient Age: >18 y Donor: Haplo Graft Source: Haplo NA + UCB Conditioning: RIC |
| Haplo-identical Transplantation for Severe Aplastic Anemia, Hypo-plastic MDS and PNH Using Peripheral Blood Stem Cells and Post-transplant Cyclophosphamide for GVHD Prophylaxis NCT03520647 | PTCy | Phase: 2 N: 56 | Disease: Nonmalignant Recipient Age: 4-75 y Donor: Haploidentical Graft Source: PBSC Conditioning: NA |
| The Safety and Efficacy of Alpha-1 Antitrypsin (AAT) for the Prevention of Graft-Versus-host Disease (GVHD) in Patients Receiving Hematopoietic Cell Transplant (MODULAATE) NCT03805789 | Alpha-1 Antitrypsin | Phase: 2/3 N: 310 | Disease: Malignant Recipient Age: >12 y Donor: MUD, MMUD Graft Source: PBSC and BM Conditioning: MAC |
| Comparison of Triple GVHD Prophylaxis Regimens for Nonmyeloablative or Reduced Intensity Conditioning Unrelated Mobilized Stem Cell Transplantation NCT03246906 | CNI, sirolimus ± MMF, ± PTCy | Phase: 2 N: 160 | Disease: Malignant Recipient Age: >18 y Donor: MUD, MMUD Graft Source: PBSC Conditioning: NMA, RIC |
| GvHD Prophylaxis in Unrelated Donor HCT: Randomized Trial Comparing PTCY Versus ATG (GRAPPA) NCT05153226 | PTCy Or ATG | Phase: 3 N: 540 | Disease: Malignant Recipient Age: >18 y Donor: Haploidentical Graft Source: PBSC Conditioning: NA |
| High-Dose Post-Transplant Cyclophosphamide, Bortezomib and Abatacept for the Prevention of Graft-versus-Host-Disease (GvHD) Following Allogenic Hematopoietic Stem Cell Transplantation (HSCT) Study NCT05289167 | PTCy, Bortezomib, Abatacept ± ATG | Phase: 1/2 N: 74 | Disease: Malignant Recipient Age: >18 y Donor: MRD, MUD, MMUD Graft Source: PBSC Conditioning: NA |
| Tildrakizumab for Prevention of Acute Graft-Versus-Host Disease NCT04112810 | Tildrakizumab (anti–IL-23 antibody), CNI/MTX | Phase: 2 N: 55 | Disease: Malignant Recipient Age: >18 y Donor: MRD, MUD Graft Source: PBSC Conditioning: MAC |
| Ustekinumab for the Prevention of Acute Graft-Versus-Host Disease After Unrelated Donor Hematopoietic Cell Transplant NCT04572815 | Ustekinumab | Phase: 2 N: 116 | Disease: Malignant Recipient Age: 18-70 y Donor: MRD, MUD Graft Source: PBSC Conditioning: MAC, RIC |
| Adding Itacitinib to Cyclophosphamide and Tacrolimus for the Prevention of Graft Versus Host Disease in Patients Undergoing Hematopoietic Stem Cell Transplants NCT05364762 | Itacitinib, PTCy, and Tacrolimus | Phase: 2 N: 50 | Disease: Malignant Recipient Age: 0-80 y Donor: MRD, MUD Graft Source: PBSC Conditioning: RIC |
| The Lowest Effective Dose of Post-Transplantation Cyclophosphamide in Combination With Sirolimus and Mycophenolate Mofetil as Graft-Versus-Host Disease Prophylaxis After Reduced Intensity Conditioning and Peripheral Blood Stem Cell Transplantation NCT05436418 | PTCy, Sirolimus, MMF Reduced dose PTCy | Phase: 1/2 N: 220 | Disease: Malignant Recipient Age: >12 y Donor: Haploidentical, MRD, MUD Graft Source: PBSC Conditioning: RIC |
| Vorinostat for GVHD Prevention in Children, Adolescents and Young Adults Undergoing Allogeneic Blood and Marrow Transplantation NCT03842696 | Vorinostat, CNI, MTX, ± PTCy | Phase: 1/2 N: 49 | Disease: Malignant Recipient Age: 3-39 y Donor: Haploidentical, MRD, MUD Graft Source: PBSC, BM Conditioning: MAC/RIC |
| PTCy + Sirolimus/VIC-1911 as GVHD Prophylaxis in Myeloablative PBSC Transplantation NCT05120570 | PTCy, sirolimus combined with VIC-1911 (Aurora Kinase A inhibitor) | Phase: 1/2 N: 75 | Disease: Malignant Recipient Age: >18 y Donor: MRD, MUD Graft Source: PBSC Conditioning: MAC |
| High Dose Thymoglobulin Instead of Cyclosporine With a Low Dose of Thymoglobulin for GVHD Prophylaxis (ATG2017) NCT03456817 | ATG, CSA, MTX High-dose ATG with low-dose CSA | Phase: 2 N: 200 | Disease: Malignant Recipient Age: >18 y Donor: MSD, MUD, MMUD Graft Source: PBSC Conditioning: MAC |
| Naive T Cell Depletion for Preventing Chronic Graft-Versus-Host Disease in Children and Young Adults With Blood Cancers Undergoing Donor Stem Cell Transplant NCT03779854 | Naive T-cell depletion, CNI/MTX | Phase: 2 N: 68 | Disease: Malignant Recipient Age: 6 mo to 22 y Donor: MRD, MUD Graft Source: PBSC, BM Conditioning: MAC |
| Trial . | Agents/approach . | Study design . | Study population . |
|---|---|---|---|
| A Randomized Double-Blind Trial of Abatacept Extended Dosing Versus Abatacept Short-Term Dosing for GVHD Prophylaxis (ABA3) NCT04380740 | Abatacept, CNI/MTX Extending dosing of abatacept for GvHD prevention | Phase: 2 N: 160 | Disease: Malignant Recipient Age: >2 y Donor: MUD/MMUD Graft Source: PBSC or BM Conditioning: MAC/RIC |
| Acute GVHD Suppression Using Costimulation Blockade to Expand Non-malignant Transplant (ASCENT) NCT03924401 | Abatacept, CNI/MTX Extended dosing of abatacept for GvHD prevention | Phase: 2 N: 30 | Disease: Nonmalignant Recipient Age: 0-20 y Donor: MUD/MMUD Graft Source: PBSC or BM Conditioning: MAC/RIC |
| Cyclophosphamide, Abatacept, and Tacrolimus for the Prevention of GVHD NCT05621759 | PTCy, Abatacept, short-course tacrolimus | Phase: 2 N: 92 | Disease: Malignant Recipient Age: >18 y Donor: Haploidentical Graft Source: PBSC Conditioning: MAC/RIC |
| Optimizing PTCy Dose and Timing NCT03983850 | PTCy, Sirolimus, MMF Reduced-dose PTCy | Phase: 1/2 N: 400 | Disease: Malignant Recipient Age: >12 y Donor: Haploidentical Graft Source: BM or PBSC Conditioning: MAC |
| HLA-Mismatched Unrelated Donor Hematopoietic Cell Transplantation With Post-Transplantation Cyclophosphamide (ACCESS) NCT04904588 | PTCy, Tacrolimus, MMF | Phase: 2 N: 300 | Disease: Malignant Recipient Age: >1 y Donor: MMUD Graft Source: PBSC, BM Conditioning: MAC, RIC, NMA |
| A Randomized Pilot Trial Comparing Anti-Thymocyte Globulin (ATG) With ATG Plus Post Transplant Cyclophosphamide (PTCy) for Prophylaxis Against Acute and Chronic Graft Versus Host Disease NCT04202835 | ATG ± PTCy | Phase 2 N: 80 | Disease: Malignant Recipient Age: 16-70 y Donor: MRD, MUD Graft Source: PBSC Conditioning: MAC, RIC |
| A Phase II Pediatric Study of GVHD Prophylaxis Regimen With No Calcineurin Inhibitors After Day +60 Post First Allogeneic Hematopoietic Cell Transplant for Hematological Malignancies NCT05579769 | CNI/MTX, Ruxolitinib ± ATG | Phase: 2 N: 32 | Disease: Malignant Recipient Age: >12 y Donor: MRD, MUD Graft Source: BM Conditioning: MAC |
| Bendamustine With or Without Cyclophosphamide in Preventing GVHD in Patients Undergoing Stem Cell Transplant NCT04022239 | Bendamustine, Tac, MMF, ± PTCy Posttransplant bendamustine | Phase: 1/2 N: 40 | Disease: Malignant Recipient Age: 18-70 y Donor: MMUD, Haploidentical Graft Source: NA Conditioning: RIC |
| Tocilizumab for the Prevention of Graft Failure and GVHD in Haplo-Cord Transplantation NCT04395222 | Tocilizumab, ± ATG Tocilizumab day −1 | Phase: 2 N: 70 | Disease: Malignant Recipient Age: >18 y Donor: Haplo Graft Source: Haplo NA + UCB Conditioning: RIC |
| Haplo-identical Transplantation for Severe Aplastic Anemia, Hypo-plastic MDS and PNH Using Peripheral Blood Stem Cells and Post-transplant Cyclophosphamide for GVHD Prophylaxis NCT03520647 | PTCy | Phase: 2 N: 56 | Disease: Nonmalignant Recipient Age: 4-75 y Donor: Haploidentical Graft Source: PBSC Conditioning: NA |
| The Safety and Efficacy of Alpha-1 Antitrypsin (AAT) for the Prevention of Graft-Versus-host Disease (GVHD) in Patients Receiving Hematopoietic Cell Transplant (MODULAATE) NCT03805789 | Alpha-1 Antitrypsin | Phase: 2/3 N: 310 | Disease: Malignant Recipient Age: >12 y Donor: MUD, MMUD Graft Source: PBSC and BM Conditioning: MAC |
| Comparison of Triple GVHD Prophylaxis Regimens for Nonmyeloablative or Reduced Intensity Conditioning Unrelated Mobilized Stem Cell Transplantation NCT03246906 | CNI, sirolimus ± MMF, ± PTCy | Phase: 2 N: 160 | Disease: Malignant Recipient Age: >18 y Donor: MUD, MMUD Graft Source: PBSC Conditioning: NMA, RIC |
| GvHD Prophylaxis in Unrelated Donor HCT: Randomized Trial Comparing PTCY Versus ATG (GRAPPA) NCT05153226 | PTCy Or ATG | Phase: 3 N: 540 | Disease: Malignant Recipient Age: >18 y Donor: Haploidentical Graft Source: PBSC Conditioning: NA |
| High-Dose Post-Transplant Cyclophosphamide, Bortezomib and Abatacept for the Prevention of Graft-versus-Host-Disease (GvHD) Following Allogenic Hematopoietic Stem Cell Transplantation (HSCT) Study NCT05289167 | PTCy, Bortezomib, Abatacept ± ATG | Phase: 1/2 N: 74 | Disease: Malignant Recipient Age: >18 y Donor: MRD, MUD, MMUD Graft Source: PBSC Conditioning: NA |
| Tildrakizumab for Prevention of Acute Graft-Versus-Host Disease NCT04112810 | Tildrakizumab (anti–IL-23 antibody), CNI/MTX | Phase: 2 N: 55 | Disease: Malignant Recipient Age: >18 y Donor: MRD, MUD Graft Source: PBSC Conditioning: MAC |
| Ustekinumab for the Prevention of Acute Graft-Versus-Host Disease After Unrelated Donor Hematopoietic Cell Transplant NCT04572815 | Ustekinumab | Phase: 2 N: 116 | Disease: Malignant Recipient Age: 18-70 y Donor: MRD, MUD Graft Source: PBSC Conditioning: MAC, RIC |
| Adding Itacitinib to Cyclophosphamide and Tacrolimus for the Prevention of Graft Versus Host Disease in Patients Undergoing Hematopoietic Stem Cell Transplants NCT05364762 | Itacitinib, PTCy, and Tacrolimus | Phase: 2 N: 50 | Disease: Malignant Recipient Age: 0-80 y Donor: MRD, MUD Graft Source: PBSC Conditioning: RIC |
| The Lowest Effective Dose of Post-Transplantation Cyclophosphamide in Combination With Sirolimus and Mycophenolate Mofetil as Graft-Versus-Host Disease Prophylaxis After Reduced Intensity Conditioning and Peripheral Blood Stem Cell Transplantation NCT05436418 | PTCy, Sirolimus, MMF Reduced dose PTCy | Phase: 1/2 N: 220 | Disease: Malignant Recipient Age: >12 y Donor: Haploidentical, MRD, MUD Graft Source: PBSC Conditioning: RIC |
| Vorinostat for GVHD Prevention in Children, Adolescents and Young Adults Undergoing Allogeneic Blood and Marrow Transplantation NCT03842696 | Vorinostat, CNI, MTX, ± PTCy | Phase: 1/2 N: 49 | Disease: Malignant Recipient Age: 3-39 y Donor: Haploidentical, MRD, MUD Graft Source: PBSC, BM Conditioning: MAC/RIC |
| PTCy + Sirolimus/VIC-1911 as GVHD Prophylaxis in Myeloablative PBSC Transplantation NCT05120570 | PTCy, sirolimus combined with VIC-1911 (Aurora Kinase A inhibitor) | Phase: 1/2 N: 75 | Disease: Malignant Recipient Age: >18 y Donor: MRD, MUD Graft Source: PBSC Conditioning: MAC |
| High Dose Thymoglobulin Instead of Cyclosporine With a Low Dose of Thymoglobulin for GVHD Prophylaxis (ATG2017) NCT03456817 | ATG, CSA, MTX High-dose ATG with low-dose CSA | Phase: 2 N: 200 | Disease: Malignant Recipient Age: >18 y Donor: MSD, MUD, MMUD Graft Source: PBSC Conditioning: MAC |
| Naive T Cell Depletion for Preventing Chronic Graft-Versus-Host Disease in Children and Young Adults With Blood Cancers Undergoing Donor Stem Cell Transplant NCT03779854 | Naive T-cell depletion, CNI/MTX | Phase: 2 N: 68 | Disease: Malignant Recipient Age: 6 mo to 22 y Donor: MRD, MUD Graft Source: PBSC, BM Conditioning: MAC |
Study agent/approach in bold.
Noncomprehensive list of actively recruiting trials extracted from ClinicalTrials.gov.
UCB, umbilical cord blood.
Sitagliptin is a dipeptidyl peptidase 4 inhibitor that was evaluated in a multicenter phase 2 nonrandomized trial of 36 patients receiving matched related or unrelated donors for hematologic malignancies, combined with tacrolimus and sirolimus.36 They observed low rates of grade 2 to 4 and 3 to 4 aGvHD at 5% and 3%, respectively. The 1-year cGvHD rate was 37%. These early results are promising and should be validated in a larger cohort of patients.
Ruxolitinib is a Janus kinase 1/2 inhibitor with efficacy in GvHD treatment. An analysis of GvHD outcomes from 2 trials using ruxolitinib maintenance after transplantation in acute myeloid leukemia (NCT03286530) and starting prior to transplant and continued as maintenance for myelofibrosis (NCT03427866) showed a low incidence of grade 2 to 4 aGvHD (24%) with no grade 3 to 4 disease, and low incidence of cGvHD (21%), including only 3.8% with moderate to severe disease.37
Vorinostat is a histone deacetylase inhibitor that has been evaluated as GvHD prophylaxis in combination with Tac/MTX.38 In patients receiving MAC for hematologic malignancies using MUD, vorinostat was given from day −10 through day +100. The grade 2 to 4 aGvHD rate was 22%, grade 3 to 4 was 8%, and cGvHD was 29%. The follow-up multicenter study is ongoing (NCT03842696).
Vedolizumab is a humanized monoclonal antibody that inhibits α4β7 integrin adhesion to MAdCAM-1 on gut endothelial cells. A phase 1b study evaluated vedolizumab combined with Tac/MTX for GvHD prophylaxis, reporting a 19% incidence of grade 2 to 4 aGvHD, with 5% grade 3 to 4 aGvHD. Results of the subsequent phase 3 randomized double-blind placebo- controlled study in unrelated donor HCT were recently presented.39 The primary end point, lower gut aGvHD-free survival, was significantly improved in patients receiving vedolizumab compared to placebo (86% vs 71%), with a decrease in lower gut aGvHD (7% with vedolizumab vs 19% with placebo).
The combination of PTCy with other agents has been evaluated in single-center studies. In a phase 1b to 2 study of patients undergoing haploidentical transplant with abatacept, PTCy, and short-course tacrolimus, grade 3 to 4 aGvHD and moderate to severe cGvHD were 5.1% and 17.1%, respectively.40 PTCy has also been combined with ATG in the MRD, unrelated donor, and haploidentical settings with encouragingly low rates of acute and chronic GvHD.41,42 Both approaches, as well as other combinations, require further study.
Conclusions
The field of GvHD prophylaxis is rapidly changing with many approaches showing superiority to standard Tac/MTX. With the many new promising options, each carrying their own distinct risks and benefits, there is not a “one-size-fits-all” approach to GvHD prevention (Table 4).
Comparison of select GvHD prevention approaches in transplant for hematologic malignancies
| Approach . | Severe aGvHD . | cGvHD . | Graft failure . | Relapse . | Immune reconstitution/ viral infections . | Optimal use . |
|---|---|---|---|---|---|---|
| Abatacept | Decreased | No impact | No impact | No impact observed | No impact/increased reactivation without severe disease | Unrelated donor (especially mismatched) |
| Posttransplant cyclophosphamide | Decreased | Decreased | Possibly increased | Increased in some studies | Delayed in some studies/ increased grade 2 infections | Unrelated, haploidentical |
| Selective ex vivo graft manipulation | Decreased | Decreased | Increased | No impact observed | Varies by approach, enhanced related to other T-cell depletion approaches | Unrelated, haploidentical (clinical trial) |
| Approach . | Severe aGvHD . | cGvHD . | Graft failure . | Relapse . | Immune reconstitution/ viral infections . | Optimal use . |
|---|---|---|---|---|---|---|
| Abatacept | Decreased | No impact | No impact | No impact observed | No impact/increased reactivation without severe disease | Unrelated donor (especially mismatched) |
| Posttransplant cyclophosphamide | Decreased | Decreased | Possibly increased | Increased in some studies | Delayed in some studies/ increased grade 2 infections | Unrelated, haploidentical |
| Selective ex vivo graft manipulation | Decreased | Decreased | Increased | No impact observed | Varies by approach, enhanced related to other T-cell depletion approaches | Unrelated, haploidentical (clinical trial) |
Comparing results of clinical trials is hindered by differences in patient populations, conditioning intensity, outcomes reported, and variable follow-up. One-year end points are more feasible, but longer follow-up is imperative to assess cGvHD, relapse, and immune reconstitution. Additionally, understanding the interactions between prophylaxis regimens and donor characteristics, including degree of matching and donor age, is also important. Only by integrating all this information can we make personalized treatment decisions for patients, taking into account their donor options, disease characteristics, comorbidities, and long-term toxicities risk.
In the current era where GvHD prevention is both feasible and safe, the expectations have been raised. There is a need to continue refining existing and emerging therapies, with the aim of preventing GvHD and associated toxicities, including infections, while optimizing primary disease control and minimizing long-term morbidities.
Conflict-of-interest disclosure
Benjamin Watkins: no competing financial interests to declare.
Muna Qayed: Honoraria, Novartis, and Vertex.
Off-label drug use
Benjamin Watkins: All the drugs discussed for GVHD prophylaxis are used off-label (except Abatacept).
Muna Qayed: All the drugs discussed for GVHD prophylaxis are used off-label (except Abatacept).